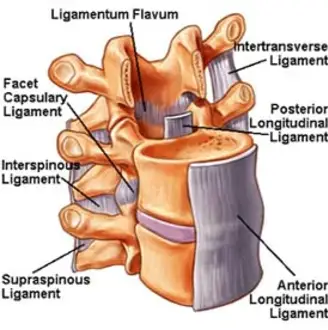
Posterior Longitudinal Ligament (PLL) Injury
Introduction:
The Posterior Longitudinal Ligament (PLL) is a key spinal structure that runs along the back (posterior) of the vertebral bodies inside the spinal canal, helping to stabilize the spine and limit excessive spinal flexion.
An injury to the PLL can result from trauma, repetitive stress, or degenerative changes, and may contribute to spinal instability, pain, or nerve compression. Such injuries are often associated with disc herniation or spinal cord impingement, particularly in the cervical and lumbar regions.
Causes of Posterior Longitudinal Ligament (PLL) Injury:
- A traumatic or whiplash injury occurs when the spine suddenly flexes or extends violently, as happens in auto accidents.
- Degenerative Disc Disease: Over time, disc degeneration can cause stress and harm to the PLL.
- Instrumentation or Spinal Surgery: Surgical operations have the potential to unintentionally damage the PLL.
- Inflammatory Conditions: Conditions that cause inflammation or weakening of the ligament include ankylosing spondylitis.
- Spinal instability: Spondylolisthesis is one condition that might make the PLL more stressed.
- The ligament may be directly invaded or weakened by tumors or infections.
- Age-Related Changes: Ligament damage may result from spinal tissues losing their flexibility and moisture.
- Improper Lifting Techniques: Poor posture when lifting large objects can put stress on the PLL and other spinal ligaments.
Symptoms of the Posterior Longitudinal Ligament Injury:
- Localized spinal pain, typically in the lumbar or cervical area
- severe or dull pain in the back.
- Aggravated by specific postures or movements.
- Radiculopathy or Referred Pain
- The legs (lumbar) or arms (cervical) may experience radiating pain.
- Muscle Weakness
- If the damage results in disc herniation, as a result to nerve root compression.
- Reduced Range of Motion
- Unstable Spine
- a sensation of spine weakening or instability, particularly when engaging in specific activities.
- Postural Changes
- In order to alleviate pain or discomfort, the patient may assume unusual positions.
- Flexion Pain
- Because of the strain on the PLL, bending forward may make you more uncomfortable.
Risk Factors of the Posterior Longitudinal Ligament Injury:
- Age: Older persons, especially those over 50, are more likely to have posterior longitudinal ligaments.
- Genetics: Given that the posterior longitudinal ligament tends to run in families, there may be a hereditary component to its formation.
- Obesity: Being obese or overweight increases the chance of developing the posterior longitudinal ligament by putting undue strain on the spinal column.
- Trauma.
- Spinal surgery: The likelihood of developing posterior longitudinal ligament is further increased by prior spinal surgery.
- Arthritis: Rheumatoid arthritis and osteoarthritis are two forms of arthritis that can raise the likelihood of posterior longitudinal ligament development.
- Diabetes.
- Smoking.
- Bad posture: Over time, poor posture can increase the likelihood of developing a posterior longitudinal ligament by placing additional strain on the spinal column.
It is important to remember that a person does not always develop a posterior longitudinal ligament just because they have one or more of these risk factors. People who have these risk factors, however, should be conscious of their elevated risk and take precautions to avoid or treat the condition should it materialize.
Diagnosis:
Imaging investigations and clinical assessment are usually used in conjunction to diagnose a posterior longitudinal ligament (PLL) damage. In a clinical setting, a doctor may evaluate symptoms such as weakness or numbness, restricted movement, and localized spinal pain. Imaging methods like MRI are best for confirming the diagnosis since they offer fine-grained images of soft tissue structures like ligaments and intervertebral discs.
The PLL and related disc pathologies may be thickened, inflamed, or disrupted on MRI. Although they are less useful for directly seeing ligament injury, CT scans and X-rays can occasionally be utilized to assess bone abnormalities or spinal alignment.
Treatment of the Posterior Longitudinal Ligament Injury:
Conservative methods are usually used to treat a posterior longitudinal ligament injury to minimize pain and inflammation, encourage healing, and prevent further harm. In the early stages, rest and activity adjustment are frequently advised to prevent the injury from getting worse.
To treat pain and inflammation, doctors may give analgesics or nonsteroidal anti-inflammatory medications (NSAIDs). The main goals of physical therapy are to strengthen the surrounding muscles, increase spinal flexibility, and improve posture to lessen ligament strain. Spinal braces may occasionally be used to temporarily support the spine while it heals.
Interventional techniques like epidural steroid injections may be used for pain relief if conservative treatments are inadequate and the injury results in serious consequences like disc herniation or nerve compression. Surgical alternatives, such as spinal fusion or decompression, may be necessary in more severe or chronic cases, particularly when neurological symptoms are present, to relieve pressure on the spinal cord or nerves and restore spinal stability. The extent of the damage, the patient’s general condition, and how well the patient responds to initial care all influence the treatment decision.
How to prevent posterior longitudinal ligament injuries:
To lower the chance of developing a posterior longitudinal ligament or, in the event that one has already occurred, to stop more damage, there are a number of actions that can be taken.
- Exercise frequently: Frequent exercise helps build stronger bones and muscles throughout the body, including the spine.
- Avoid smoking: Smoking can reduce blood supply to the spinal column, which raises the possibility of posterior longitudinal ligament development. As a result, smoking cessation or abstinence can help prevent posterior longitudinal ligament damage.
- Seek immediate medical assistance for any spinal injuries: Early management can lower the likelihood of developing posterior longitudinal ligament and potentially stop further spine injuries.
Prognosis:
The degree of the injury and the existence of related spinal disorders, such as disc herniation or spinal cord compression, significantly influence the prognosis of a posterior longitudinal ligament (PLL) injury. Conservative care, such as rest, physical therapy, and pain control, can result in a full recovery and notable improvement in mild cases.
However, if the spinal cord or nerve roots are affected, more serious injuries or long-term strain may cause neurological problems, restricted mobility, or ongoing pain. When conservative treatment is ineffective or there is severe spinal instability, surgery may be required. Many people can anticipate a positive outcome with the right care and therapy, but depending on the severity of the damage, some people may have long-term disabilities.
Complications:
When damage to the Posterior Longitudinal Ligament (PLL) causes instability or compression in the spinal column, complications may result. Since the PLL typically aids in disc material containment, one of the most frequent side effects is an elevated risk of intervertebral disc herniation. Muscle weakness, decreased spinal mobility, and persistent neck or back pain can also be symptoms of ligament damage.
Neurological consequences like numbness, tingling, or even paralysis can happen in more severe cases, particularly when the spinal cord or nerve roots are crushed. Furthermore, if left untreated, chronic inflammation or instability can lead to degenerative changes in the spine and raise the risk of long-term impairment.
Conclusion:
To sum up, a Posterior Longitudinal Ligament (PLL) injury is a serious spinal disorder that can affect neurological function, movement, and stability, particularly when it is linked to trauma or degenerative changes. Although conservative treatment works effectively in many circumstances, surgery may be necessary for serious injuries. Most people can retain a good quality of life and gain functional improvement with prompt care and therapy.
FAQs:
How is a PLC injury treated?
For milder cases of posterolateral corner (PLC) injuries, non-surgical methods such as rest, ice, compression, and elevation (RICE) can be used. For more serious injuries, particularly those affecting other ligaments or persistent instability, surgical reconstruction may be necessary. For best results, early action is essential, including timely medical examination and suitable management.
How are posterior longitudinal ligaments tested?
The diagnosis is made using lateral radiographs of the cervical spine. For determining the thickness and extent of ossification, a CT scan is the recommended technique.
The posterior longitudinal ligament limits what range of motion?
It just marginally stops the spinal column from hyperflexing. Although ligament issues may result in posterior spinal disc herniation, they also prevent it.
Which symptoms indicate a posterior longitudinal ligament injury?
OPLL usually starts out with little to no symptoms. Hand numbness, tingling, and/or slight pain are examples of minor symptoms. Unpleasant feelings can occasionally exist without any physical contact.
What is the posterior longitudinal ligament’s unique characteristic?
This is crucial for knowing the normal position of a spinal disc herniation and other pathological disorders of the spine.
How is a posterior longitudinal ligament damage treated?
A posterior longitudinal ligament injury can be treated with rest, physical therapy, painkillers, and, in extreme situations, surgery.
References
- Patel, D. (2023e, August 22). Posterior longitudinal ligament – anatomy, structure, function. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/posterior-longitudinal-ligament/
- Hacking, C., & Wong, A. (2015). Posterior longitudinal ligament. Radiopaedia.org. https://doi.org/10.53347/rid-36586
- Tan, J., Shen, L., Fang, L., Chen, D., Xing, S., Shi, G., He, X., Wang, J., Zhang, J., Liao, T., & Su, J. (2015). Correlations between posterior longitudinal injury and parameters of vertebral body damage. Journal of Surgical Research, 199(2), 552–556. https://doi.org/10.1016/j.jss.2015.04.068