Hypothenar hammer syndrome (HHS)
Introduction
Hypothenar Hammer Syndrome (HHS) is a vascular condition caused by repeated trauma to the ulnar artery in the hypothenar region of the hand (palm side near the little finger). It commonly affects individuals who use the palm forcefully, such as mechanics, construction workers, or martial artists.
Symptoms include pain, cold sensitivity, numbness, and discoloration of the fingers due to reduced blood flow. Diagnosis involves imaging studies like Doppler ultrasound or angiography, and treatment ranges from lifestyle modifications to surgical intervention in severe cases.
Hypothenar Hammer Syndrome: What is it?
The muscles that control the little finger’s mobility are referred to as hypothenar. The hypothenar eminence, the palm’s edge, comprises some of these muscles. It happens when employees often break, push, and twist hard objects with their palms—particularly the hypothenar eminence—as a hammer. These activities have the potential to harm the hand’s blood vessels, particularly the ulnar artery. This artery provides blood to the fingers by passing through the palm’s hypothenar region.
Men with an average age of 40 are usually the ones that suffer from hypothenar hammer syndrome. Auto mechanics, metalworkers, lathe operators, miners, machinists, bakers, carpenters, and bricklayers are among the workers who are at danger. Users of vibrating tools are also at risk. Sports like karate, baseball, mountain biking, golf, tennis, hockey, handball, volleyball, badminton, breakdancing, and weightlifting have also been linked to hypothenar hammer syndrome.
Relevant Anatomy
The ulnar artery, which passes through the hypothenar eminence (the fleshy area on the palm near the little finger), can become damaged and have less blood flow to the fingers it supplies. This condition is known as hypothenar hammer syndrome. The ring and little fingers are typically affected. The damage usually occurs as the artery passes through Guyon’s canal, where it may be compressed against the hook of the hamate bone.
- The ulnar artery is the primary blood vessel affected in hypothenar hammer syndrome.
- Guyon’s canal, a channel in the wrist where the ulnar artery runs between the pisiform bone and the hook of the hamate bone, is the most frequently damaged area of the artery.
- The syndrome is caused by repetitive trauma in this fleshy portion of the palm, which is made up of the muscles that control the movement of the little finger.
Pathology
Any blunt trauma or repeated compression to this area could be the reason. The ulnar artery is especially at risk because it passes the hook of hamate. Dissection, stenosis, occlusion, or the development of a false aneurysm can all be consequences of artery trauma. Distal thromboembolism could make this more difficult.
Causes
In essence, hypothenar hammer syndrome(HHS) is a condition that arises from occupational activities that involve forceful striking with the heel of the hand. It is caused by repetitive trauma to the hypothenar eminence of the hand, most commonly when someone repeatedly strikes objects with the palm of their hand as a hammer. This causes damage to the ulnar artery and subsequent digital ischemia due to blood clots or aneurysms in that area.
- Repetitive trauma: The hypothenar region, or the fleshy area at the base of the little finger, is the main target of repetitive blunt trauma.
- Ulnar artery damage: The ulnar artery, which passes through the hypothenar area, is the main target of this trauma.
- Factors related to the workplace: Carpentry, construction, mechanics, and any other occupation where people often use their palm as a striking tool are among the occupations that frequently cause hypothenar hammer syndrome.
- Possible underlying conditions: Some people may be more susceptible to injury from recurrent trauma because of pre-existing anomalies in their ulnar arteries.
Signs and symptoms
Hypothenar hammer syndrome is characterized by pain over the ring finger and hypothenar eminence, paresthesia (pins and needles), loss of feeling, a decrease in hand muscle strength, and difficulty holding on to a heavy thing in the affected hand. The fingers change color (typically turning blue or white) and become sensitive to cold.
- Cold sensation and pain in the palm
- raynaud’s phenomenon
- Tender hypothenar eminence
- Ischemia of (usually) the fourth and fifth fingers
- Tinel sign positive (caused by compression of the ulnar nerve)
- Allen test Positive
- Pain and tenderness in the hypothenar eminence, which is the area at the base of the little finger
- Pins and needles (paresthesia) in the ring and little fingers
- Loss of feeling in the little and ring fingers
- Decreased hand muscle strength
- Difficulty while holding heavy objects
- Cold intolerance and sensitivity in the fingers
- Bluish or white discoloration of the fingers
- Ulceration and ischemia of the ring and little fingers
Diagnosis
Angiography (DSA)
- The distal ulnar artery has a “corkscrew” or beaded uneven appearance.
- Aneurysm formation
- Blockage of the section of the ulnar artery that is above the hamate hook.
- Distal digital arteries that are blocked or inadequately filled in an ulnar arterial distribution.
Duplex sonography
When used properly, duplex sonography can be a great way to check for aneurysm formation and patency in the ulnar artery. Duplex sonography is non-invasive and reasonably priced. The method depends on the operator and calls for experience. It is challenging to utilize for surgical mapping, because its range of view is restricted. For HHS, the exam is best viewed as a screening tool.
HHS physical examination results include a positive Allen’s test in the affected hand, soreness at the hypothenar eminence, and no ulnar pulse. Duplex ultrasound is an appropriate first test, and the gold standard for diagnosis is angiography.
Allen’s test

The radial artery can be felt at the wrist’s proximal skin crease and then compressed with three fingers. Similarly, the ulnar artery is found and then compressed using three fingers. The individual is instructed to crush and relax the hand ten times while both arteries are compressed. After that, the hand is kept open to prevent the fingers and wrist from becoming overly stretched and spread out. It is seen that the palm is stained. After the ulnar artery is released, it is observed how long it takes for the palm, particularly the thumb and thenar eminence, to flush. The test is considered a success. if the capillary refill time is less than six seconds.
The radial artery is subsequently examined similarly to finish the examination. It is necessary to examine both hands for comparison.
Wide finger separation and excessive hand extension during the Allen test can produce a false-negative result. After the ulnar artery is released, portions of the fingers and palm will still be cleaned because of the obstruction of the trans palmar arch. As stated in Allen’s original paper, the test should be conducted with the hand slightly open to avoid this.
Treatment
The management strategy as a whole is challenged. Particularly when there is vasospasm and sufficient collateral circulation, non-surgical therapy is seen to be adequate.
Medical treatment
- Local care of fingers with necrosis
- Pentoxifylline: for viscosity reduction
- Calcium channel blockers (e.g. nifedipine, diltiazem)
- Antiplatelet agents or anticoagulation
Physical therapy treatment
Ice application to reduce pain and swelling.

- The main mechanism underlying hypothenar hammer syndrome is inflammation caused by injury or recurrent stress, which can be managed by applying ice to the affected part of the hand (hypothenar eminence). This is a common first-aid technique.
- By narrowing blood vessels and decreasing blood flow to the area, using ice helps reduce pain and swelling.
Application: Apply ice to the affected area for 20 minutes at a time, multiple times a day, wrapping it in a small towel to prevent direct skin contact.
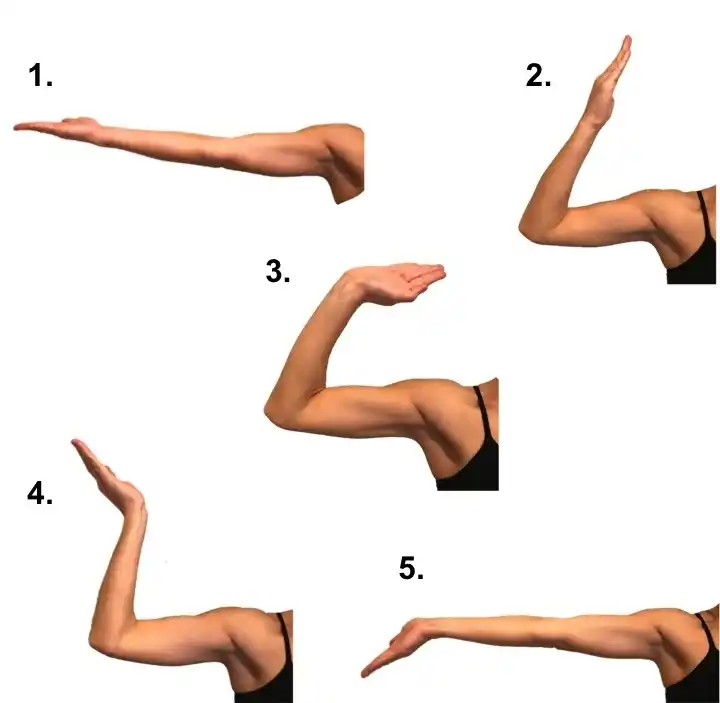
Gentle range of motion exercise
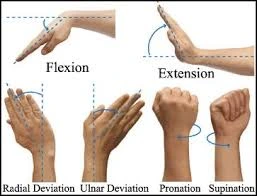
- Wrist flexion and extension
- Finger flexion and extension
- Radial and ulnar deviation movements
- Thumb movements
Massage

A healthcare professional should be consulted for a proper diagnosis and management of Hypothenar Hammer Syndrome (HHS), which typically involves addressing the damaged blood vessel through medical or surgical interventions depending on the severity. Although a gentle massage may offer some temporary relief for pain in the hypothenar area affected by HHS, it is not advised as a primary treatment method as it may worsen the underlying vascular damage caused by the condition.
Aggressive massage may aggravate the already damaged blood vessel, leading to additional clots or worsened ischemia (lower blood supply) to the fingers. HHS involves injury to the ulnar artery in the hypothenar region.
The correct diagnosis and treatment of HHS may be delayed if the pain is only related to muscle strain and is managed with massage therapy without addressing the underlying vascular problem.
Stretching
To potentially relieve symptoms of hypothenar hammer syndrome, try these gentle stretches that target the muscles of the hypothenar eminence, which is the fleshy area on the palm side of your hand near the pinky finger. These stretches include the flexor digiti minimi brevis, opponens digiti minimi, and abductor digiti minimi.
Spread your fingers wide apart, keeping your thumb extended away from the other fingers, and hold for a few seconds. Repeat several times.
Wrist flexion stretch:
- Bend your wrist downwards, gently pulling your fingers towards your forearm with the other hand, and hold for a few seconds. Repeat on the other side.
Wrist extension stretch:
- Bend your wrist upwards, gently pulling your fingers back towards your forearm with the other hand, and hold for a few seconds. Repeat on the other side.
Thumb extension stretch:
- Extend your thumb outward, gently pulling it with the other hand towards your body, and hold for a few seconds. Repeat on the other side.
Thumb opposition stretch:
- Touch your thumb to the base of each finger, one at a time, and hold for a few seconds. Repeat several times.
Cold avoidance
“Cold avoidance” is a crucial conservative treatment approach for hypothenar hammer syndrome, which means that individuals with the condition should actively avoid cold environments as this can worsen their symptoms of pain, numbness, and skin that remains white or pale in their fingers. This is because the underlying vascular damage in the hand causes reduced blood flow, which makes things worse, these symptoms.
Mechanism:
Hypothenar hammer syndrome involves damage to the ulnar artery in the hand, which can lead to reduced blood supply to the fingers, especially when exposed to cold temperatures that cause blood vessels to constrict.
Symptoms with cold exposure:
- Fingertips turning pale or white
- Numbness or tingling sensation in the fingers
- Pain in the hand, particularly in the affected fingers
- Limit activities that expose the hands to cold, such as handling cold objects or working in cold environments.
- Warm hand care: Regularly warm up the hands with warm water or hand warmers.
Surgical treatment
Aneurysm ligation, aneurysm resection with primary arterial end-to-end anastomosis, or interposition graft reconstruction with vein or artery and sympathectomy are the surgical therapy options.
To relieve symptoms such as pain and digital ischemia caused by the damaged artery in the hand’s hypothenar eminence, surgery for hypothenar hammer syndrome usually involves removing the affected ulnar artery aneurysm.
Depending on the severity of the aneurysm and the condition of the artery, there may be decisions to either directly repair the artery with an end-to-end connection or recreate it using a vein graft if required.
- Ulnar artery excision: Surgical removal of the affected segment of the ulnar artery where the aneurysm is located.
- Arterial reconstruction: Using a vein graft or other vascular grafts to re-establish blood flow after removing the damaged artery segment.
- Ligation of the ulnar artery: In some cases, ligation (tying off) of the ulnar artery may be necessary.
The ulnar artery in the hypothenar eminence—the fleshy region on the palm side of the hand close to the pinky finger—is the target of the surgery.
Procedure:
- To reveal the aneurysm, a little incision is made over the affected area.
- Carefully, the aneurysm is separated from the surrounding tissues.
- To stop the bleeding, the artery is constricted both proximally and distally.
- The artery’s aneurysmal section is removed.
- Depending on the circumstances, either a vein graft taken from the leg or an end-to-end anastomosis may be used to directly heal the artery.
Indication for surgery
- Surgery is indicated for severe symptoms such as numbness, pain, or color changes in the fingers caused by impaired blood flow.
- Failure of medication-based or activity-based conservative treatment.
- Presence of a large or sick ulnar artery aneurysm.
Lifestyle modification
Using padded gloves, switching tasks frequently to reduce strain, and using the right tools to minimize direct impact on the hypothenar region of the hand are all ways to prevent further trauma with Hypothenar Hammer Syndrome (HHS), which is primarily caused by repetitive forceful banging or slapping actions with the palm.
- Padded protective gloves: Wear padded gloves to minimize trauma to the hand.
- Activity modification: Stop activities that trigger symptoms, like repetitive hand movements or heavy gripping.
- Use proper tools: Utilize tools designed to shock absorb and reduce impact on the hand, such as rubber mallets instead of metal hammers.
- Rotate tasks: Switch between different hand movements to avoid prolonged pressure on the hypothenar area.
- Take breaks: Regularly rest your hands to prevent fatigue and overuse.
- Ergonomic adjustments: Modify workstations to optimize hand posture and reduce repetitive strain.
- Avoid activities that aggravate symptoms: Limit activities that involve repetitive hand pounding, such as heavy manual labor, certain sports (e.g., handball, baseball), or hobbies that put stress on the hands.
- Smoking cessation: Quitting smoking can improve blood circulation and reduce the risk of complications.
Prevention
Understand the signs and causes of this illness. The main goals of prevention should be to enhance work procedures and not beat up, banging, pressing, crushing, pushing, or twisting hard objects with the palm acting as a hammer. Tools that vibrate the palm, such as pliers, brush cutters, trimmers, milling machines, grinders, jackhammers, saws, wrenches, and so on, can also be dangerous. Grasping tools tightly in the palm is associated with some cases.
Using well-kept equipment to lessen vibration. Change tasks or take a break. To prevent severe injury to the hand’s heel, wear padded gloves when working. Never strike an object or instrument with your hands. Never grasp anything with too much force.
Conclusion
Due to its low prevalence, hypothenar hammer syndrome may go untreated for radial artery flow compensation and is probably underdiagnosed in hand laborers, resulting in a delayed diagnosis. In non-symptomatic situations, risk factor control and observation are the therapeutic modalities. In our case, the pain was surgically relieved due to a nerve blockage. Surgery is not justified at the time of the new thrombosis in a patient who is asymptomatic and receiving good medication management.
FAQs
How is hypothenar hammer syndrome tested for?
Tenderness at the hypothenar eminence, lack of ulnar pulse, and positive Allen’s test in the affected hand are among the physical examination findings of HHS. Duplex ultrasound is a suitable initial test, while angiography is the gold standard for diagnosis.
Why does hypothenar hammer syndrome occur?
Vibrating tool users are likewise susceptible. Sports like karate, baseball, mountain biking, golf, tennis, hockey, handball, volleyball, badminton, breakdancing, and weightlifting have also been linked to hypothenar hammer syndrome.
What kinds of damage may a hammer cause?
A hammer hit can cause damage that often results in cracked fingers, but if you’re lucky, you might leave with just mild bruising. When utilizing this tool, employees should aim to keep their focus on the task at hand and prevent distractions.
Why does hypothenar atrophy occur?
Ulnar neuropathy at the elbow or wrist is frequently the cause of atrophy of the interossei and hypothenar muscles while the thenar muscles remain intact. An ulnar neuropathy at the wrist (distal Guyon canal or piso-hamate hiatus) is typically the source of interossei atrophy with sparing of the thenar and hypothenar muscles.
Hypothenar hammer syndrome affects which of the following arteries?
Damage to the ulnar artery from sports or work-related activities results in hypothenar hammer syndrome (HHS). When a younger male exhibits pain, a palpable lump, and ischemia in the dominant hand, the diagnosis should be suspected.
Which treatments are currently available for hypothenar hammer syndrome?
The degree of vascular damage greatly influences the course of treatment. Avoiding additional trauma, calcium channel blockers (such as nifedipine or diltiazem), antiplatelet or anticoagulant medications, and pentoxifylline to lower blood viscosity are all examples of non-surgical treatment.
What danger does a hammer pose?
Even if using a hammer is easy, there are still risks involved. If you swing the hammer back too far, the claw could strike your eye. Alternatively, you can get struck in the face or eye by a hammer or material debris. Wear safety eyewear and make sure they are fastened securely.
A hammer injury: what is it?
The force required to use a hammer is considerable, and improper gripping technique can cause hand injuries. Broken bones, compressed fingers, and bruises are a few examples of these injuries.
Hypothenar Hammer Syndrome: What causes it?
Digital ischemia is a hallmark of Hypothenar Hammer Syndrome (HHS), a disorder caused by repeated damage to the hand’s hypothenar eminence. It happens to those who frequently push, crush, or twist objects with their palms acting as hammers.
How can hand-arm vibration be decreased?
Utilize products like suspension systems and jigs to lessen the requirement for tight grips when handling heavy instruments. Reduce the amount of time your staff is subjected to vibration. Plan your work so that people aren’t exposed to vibration for extended periods; many, shorter durations are better.
Reference
- Government of Canada, Canadian Centre for Occupational Health and Safety. (2024, May 10). Hypothenar Hammer Syndrome. https://www.ccohs.ca/oshanswers/diseases/hypothen.html
- Rezaee, A., & Gaillard, F. (2008). Hypothenar hammer syndrome. Radiopaedia.org. https://doi.org/10.53347/rid-1486
- Cigna, E., Spagnoli, A. M., Tarallo, M., De Santo, L., Monacelli, G., & Scuderi, N. (2010). Therapeutic management of Hypothenar Hammer syndrome causing ulnar nerve entrapment. Plastic Surgery International, 2010, 1–5. https://doi.org/10.1155/2010/343820
- Wikipedia contributors. (2025, February 21). Hypothenar hammer syndrome. Wikipedia. https://en.wikipedia.org/wiki/Hypothenar_hammer_syndrome