Shoulder Hand Syndrome
What is Shoulder-hand syndrome?
Shoulder-Hand Syndrome, also known as Complex Regional Pain Syndrome (CRPS) Type I, is a chronic pain condition that typically affects one of the upper limbs, such as the shoulder, arm, or hand. It usually follows an injury or surgery and is characterized by severe pain, swelling, and changes in skin color and temperature in the affected area.
The exact cause of Shoulder-Hand Syndrome is not fully understood, but it is believed to involve an abnormal response of the nervous system to injury.
- A disorder that affects people over 50 who have had an acute MI, a cerebrovascular accident, or a head trauma. It is characterized by shoulder discomfort, swelling, stiffness, vasomotor signs in the arm and hand, and skin edema/in duration.
- Reflex sympathetic stimulation has been linked to shoulder-hand syndrome; some patients go on to develop sclerodactyly, adhesive capsulitis, and reduced range of motion as a result of regional demineralization.
- The hand may get hot, sweaty, and bloated due to a loss of muscular mass. Recovery that occurs on its own is typical, but it can take up to two years.
- Steinbrocker syndrome, commonly referred to as reflex sympathetic dystrophy syndrome, is a term used to describe a complex of integrated finger contracture symptoms as well as ipsilateral hand discomfort and edema that are related to shoulder pain and shoulder mobility disorders.
- 90% of patients had a 50-year-old age at onset, with a slightly higher proportion of women than men.
In most cases, the shoulder-hand syndrome begins as a reflex dystrophy accompanied by causalgia, which is a sore shoulder. - Additionally, this is linked to pain and edema on the affected side of the hand.
- A stiff shoulder becomes more and more uncomfortable as a result of underusing the affected muscles.
- The hand starts to enlarge uniformly and slowly loses its range of motion in the finger joints.
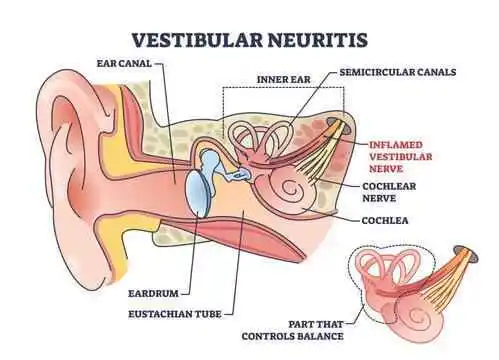
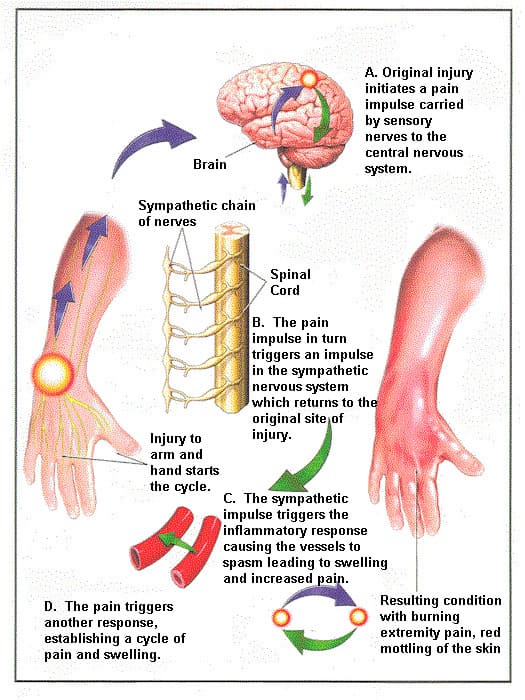
- In response to pain that is felt remotely, the sympathetic nervous system in the affected area initiates a reflexive efferent reactive vasomotor action.
- (1) The patient reports that they have a burning sensation in their hand that is concurrently chilly and clammy or cold, red, wet, stiff, and touch or pressure-sensitive on the surface.
- (2) The skin has grown, the hand looks white and creaseless, and it is getting colder and stiffer.
- (3) Osteoporosis may become visible on an x-ray, and the hand appears pale and thin with muscle atrophy (guttering) and joint contractures. The hand and arm are usually non-functional and unusable at the end of this process.
Pathology:
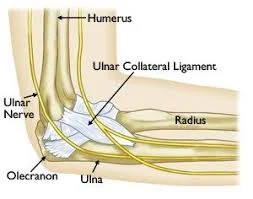
- The distal degeneration of small-diameter peripheral axons may be the cause of shoulder hand syndrome, which manifests as discomfort, edema, osteopenia, and vasomotor instability.
- Cortical alterations point to a potential pathophysiological role.
- Damage to Nerves: It’s believed that a nerve insult at first may set off an inflammatory reaction that becomes dysregulated.
- Immune Response Alterations and Inflammation: CRPS is linked to both of these conditions. Pain and additional symptoms may be exacerbated by this ongoing inflammation.
- Autonomic Nervous System Dysfunction: The illness may also result in issues with the autonomic nervous system, which controls involuntary body processes like blood flow and perspiration.
Causes of Shoulder Hand Syndrome
- trauma (usually mild).
- cardiac infarction and ischemic heart disease.
- spinal cord injury.
- brain damage.
- infections following a stroke.
- surgery.
This “short circuit” causes the sympathetic (unconscious) nervous system to become overactive, which in turn affects the local blood flow and sweat glands. It seems that certain people are more genetically predisposed to this illness than others.
Signs and Symptoms of Shoulder Hand Syndrome:
as a result of many causes and clinical presentations. following the commencement of the disease by longer than 2 to 16 weeks, with the longest period being up to 14 months, secondary to myocardial infarction.
Left shoulder and hand stiffness, tiredness, and discomfort were slightly more common than right shoulder and hand stiffness, or bilateral shoulder and hand onset. On the other hand, the hands can suddenly become painful, stiff, swollen, hypersensitive, sweaty, or change color.
Three stages:
- Stage 1: includes discomfort in the hands and shoulders, movement abnormalities that cause swelling to spread later, a progressive stiffness that appears, and a broader range of shoulder pain that does not involve the elbow.
- Stage 2: Shoulder joint dysfunction, finger flexion contracture and stiffness, and muscular atrophy may gradually decrease and disappear.
Significant osteoporosis was seen on the X-ray film; this phase will last three to six months. - Stage 3: There was reduced residual pain in the frozen shoulder, major obstacles to finger tonic deformation activities, and contraction of the palm and subcutaneous tissue. The length of the symptoms varies; some last for several years, and some end as the body develops or heals.
Clinical Features of Shoulder Hand Syndrome:
Pain:
- Severe, continuous, scorching, and/or deeply painful pain that affects one or more extremities.
- All tactile stimulation of the skin, such as clothes or a slight breeze, can cause pain perception, known as allodynia.
- Flaccid dysaesthesias and sharp pains.
- Skin changes: The skin can look scaly, dry, or glossy (dystrophy-atrophy).
- pustules, rashes, and ulcers.
- Skin that feels either warm or chilly to the touch may be a sign of abnormal sympathetic (vasomotor) activity.
- elevated goose-flesh-induced perspiration (sudomotor changes) or elevated skin temperature (pilomotor changes).
Swelling:
- localized; pitting at first, then Brawnyb.On the skin’s surface, edema can be distinguished clearly along a line.
Movement disorder:
- might become dystonic.
- Natural history begins with disuse atrophy.
- Symptom spread: A “continuity type” of spread occurs when the symptoms move up from the original location, for as from the hand to the shoulder.
- an “independent type” in which the illness extends to a different, remote area of the body. This kind of spread could be brought on by a second trauma or it could be spontaneous.
- entire body RSD.
Differential Diagnosis
- Undiagnosed local pathology (sprain, fracture).
- acute vasospasm.
- cellulitis.
- lymphatic swelling.
- Raynaud’s syndrome.
- obliterans thromboangiitis.
- erythromelalgia.
- DVT.
- Additionally, diabetic neuropathy, occupational overuse syndromes, and nerve entrapment syndromes.
Treatment of Shoulder Hand Syndrome:
Undoubtedly, the secret to a successful course of treatment is a highly qualified multidisciplinary team that is driven, well-coordinated, and employs tailored therapy to address the illness.
There is no known scientifically proven remedy.
The goal of therapy is to control the disease’s symptoms and indicators.
It is best to take a comprehensive strategy that includes physical therapy, psychological counseling, and medication.
Physiotherapy Treatment:
- In order to prevent the injured limb from contracting and atrophying, early physical therapy is crucial.
- demands that the patient participate actively in their treatment.

- physical therapy intervention.
- TENS.
- Aquatic therapy.
- Mirror therapy
- Desensitization.
- Gradual weight bearing.
- Stretching.
- Fine motor control.
In acute phase:
Treatment for the acute phase should consist of immobilization and contralateral therapy. In the acute period, worsening may result from intensive aggressive therapy.
In the chronic stage:
The edema can be helped to recede by lymphatic drainage. more proximal or more medial tender points are addressed before more distally and laterally located points; more severe tender points as determined by tenderness.
Therapeutic exercise consists of sensory desensitization programs combined with isometric strengthening therapy and active isotonic training.
Exercises for the torso and all four extremities are part of the strengthening program. Theraband can be used for workouts.
Programs for desensitization involve exposing patients to stimuli such as various textiles, light or deep pressures, vibration, tapping, heat, or cold. Exercises such as stress-loading (e.g., walking, carrying weights, cleaning), functional training, endurance training, and textual instructions can all be included. Providing a home fitness routine for the patient is also beneficial.
Mirror therapy
Mirror therapy, also known as mirror visual feedback, is putting both hands into a box with a mirror between the two compartments and moving both hands to observe the unaffected hand’s reflection in the mirror.
Increase performance.
Graded motor learning and imagery:
Graded motor imagery includes both imagined hand movement and the awareness of hand laterality.
relaxation.
Cognitive-behavioral therapy:
Deep breathing techniques, biofeedback, and relaxation training are all part of cognitive-behavioral therapy.
Neuromodulation or invasive stimulation techniques:
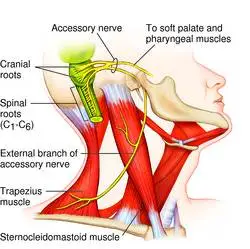
Techniques for invasive stimulation, also known as neuromodulation, include deep brain stimulation, electrotherapy, epidural spinal cord stimulation, and peripheral nerve stimulation using implanted electrodes.
Electrotherapy includes non-invasive brain stimulation (repetitive transcranial magnetic stimulation), spinal cord stimulation, and transcutaneous electric nerve stimulation (TENS).
Additional therapies:
Whirlpool and contrast bathrooms.
Rehabilitation for both hobbies and occupations.
Psychological interventions include counseling, pain education, cognitive-behavioral therapy (CBT), operant conditioning (OC), and relaxation methods.
Electroacupuncture and acupuncture.
training in tactile sensory discernment.
bearing weight.
therapy using ultrasound.
Applying Kinesiotape.
Psychological therapy:
A crucial component of the interdisciplinary treatment strategy is psychological therapy. Significant psychological dysfunction is seen in many individuals with shoulder hand syndrome; however, this is a reflection of the disease process rather than its cause.
Pain management techniques.
biofeedback.
training for relaxation.
Cognitive behavioral intervention.
mirroring oneself.
Invasive/intervention therapy:
Sympathetic nerve blocks are an invasive/interventional therapeutic option.
stimulation of the spinal cord.
Chemical and/or surgical sympathectomy.
auxiliary nerve stimulant.
intrathecal pump for baclofen.
Surgical Treatment
Surgical procedures could be a more successful way to treat the illness if non-surgical options don’t work.
An apparatus for stimulating the spinal cord
Small electrodes that deliver mild electric shocks to the injured nerves are inserted in your spine.
Installing a pain pump:
Important supplementary therapies for shoulder-hand dysfunction include counseling and psychological testing.
Conclusion:
Often affecting one of the extremities (arms, legs, hands, or feet), shoulder-hand syndrome is often referred to as complex regional pain syndrome (CRPS) or reflex sympathetic dystrophy (RSD). Excruciating pain, edema, and skin changes are its hallmarks.
Several important elements are included in the conclusion regarding shoulder-hand syndrome (CRPS):
- Early Diagnosis and Intervention: In order to minimize symptoms and stop the illness from getting worse, early treatment options may include physical therapy, pain management, and, in certain situations, medication.
- Multidisciplinary Approach: Because the syndrome is complicated, a thorough, multidisciplinary approach is frequently required to manage it. Physical therapy, occupational therapy, pain management, psychological support, and even surgical procedures might all fall under this category.
- Effective symptom management aims to minimize discomfort, enhance function, and stop or restrict the progression of symptoms. Treatment regimens are frequently customized for each patient and may include nerve blocks, pharmaceuticals, physical therapy, and behavioral therapy.
- Prognosis: Depending on the severity and timing of treatment, there are different outcomes for shoulder-hand syndrome. While some individuals would totally heal, others might struggle with ongoing pain and impairment.
- Patient Support and Education: It is crucial that patients and their families receive information about the illness, how it progresses, and available treatments. Patients can manage the emotional and psychological effects of having chronic pain with the aid of support groups and counseling.
To control symptoms and enhance the quality of life for those impacted, shoulder-hand syndrome is an intricate disorder that calls for a coordinated, individualized approach to care.
FAQs
How can shoulder-hand syndrome be avoided?
It works well for stroke patients to reduce discomfort and swelling in their upper limbs and to improve their sensory-motor function. In stroke survivors, a functioning shoulder orthosis lowers the chance of shoulder subluxation and shoulder-hand syndrome.
What three CRPS symptoms exist?
cold or tactile sensitivity.
swelling where the discomfort is.
Variations in skin temperature, with patches of sweat and cold patches.
skin color variations, from blotchy and white to red or blue.
Which score corresponds to shoulder-hand syndrome?
The effectiveness of subluxation treatment in avoiding or lowering SHS may be monitored using this method.
Are CRPS and shoulder-hand syndrome the same thing?
CRPS can also affect the arms, legs, and feet. Reflex sympathetic dystrophy, Sudeck’s atrophy, shoulder-hand syndrome, and causalgia were some of the earlier names for this illness.
Shoulder-hand syndrome: what causes it?
Shoulder-hand syndrome: what causes it?
Causes: This syndrome may result from falls, fractured wrist bones, heart attacks, strokes, and possibly the use of certain medicines (such as barbiturates).
What is shoulder-hand syndrome’s third stage?
Shoulder Hand Syndrome stages include:
Stage 1: Acute
Stage 2–dystrophic
Atrophic stage three.
What other term would you give the shoulder-hand syndrome?
Shoulder-hand syndrome is also known as:
Dystrophia reflex sympathetic
Sudeck’s atrophy Syndrome of the shoulders
The Steinbrocker condition
causative pain.
What is the best way to relieve shoulder and hand pain?
To relieve pain:
Gradually get back to your regular activities.
Ibuprofen or acetaminophen (found in Tylenol) can help reduce pain and inflammation.
Why does shoulder-arm syndrome occur?
Occasionally, a sprain, cut, or small fracture might result in shoulder-arm syndrome, a painful disability. Even though the initial reason may not have been severe, the patient nonetheless has a full, discolored, sore, unpleasant, and non-functional arm and hand.
Shoulder-hand syndrome: what is it?
The term “shoulder hand syndrome” describes excruciating impairments of the upper extremities brought on by sympathetic nervous system disturbances. The observed trophic and vasomotor symptoms are assumed to be the result of reflexive stimulation of the sympathetic nervous system.
References
- Physiotherapist, N. P. (2023, December 13). Shoulder Hand Syndrome Cause, Symptoms, Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/shoulder-hand-syndrome-physiotherapy-management/