Wrist and Hand Examination
A wrist and hand examination involves a detailed assessment of the anatomical structures, function, and range of motion of the wrist, hand, and fingers. It includes inspection, palpation, evaluation of joint movements, strength testing, and special tests to identify conditions such as fractures, tendon injuries, carpal tunnel syndrome, arthritis, and other musculoskeletal or neurological disorders. This examination is vital for accurate diagnosis and effective treatment planning.
Anatomy of wrist and hand joints
- The joint at the end of your forearm is called your wrist. The hinge that joins your arm and hand allows you to move the fingers around.
- Your hand, which is made up of your thumb, fingers, and palm, begins where your wrist ends.
Bones of the hands:
- You have nineteen bones on each hand. They are divided into groups based on their location and function:
- Metacarpals are the bones that give your palm its shape.
- Phalanges are the individual bones that make up the segments on your thumb and fingers.
- Sesamoids, which are small bones, help your tendons move smoothly.
The bones of the wrist:
Your wrist is a complicated joint made up of eight bones arranged in two rows.
The following are included in the proximal row, which is located closest to your forearm on the back of your hand:
- Scaphoid.
- Lunate.
- Triquetrum.
- Pisiform.
The following are included in the distal row, which is the area closest to the palm of your hand on the lower portion of your wrist:
- Trapezium.
- Trapezoid.
- Capitate.
- Hamate.
The portion of your wrist that allows movement and rotation is formed by the junction of the scaphoid and lunate bones with radius, the larger of the two forearm bones.
- The rounded area between your pisiform, hamate, scaphoid, and trapezium is known as the carpal tunnel. Nine tendons, four ligaments, and one nerve go through this area.
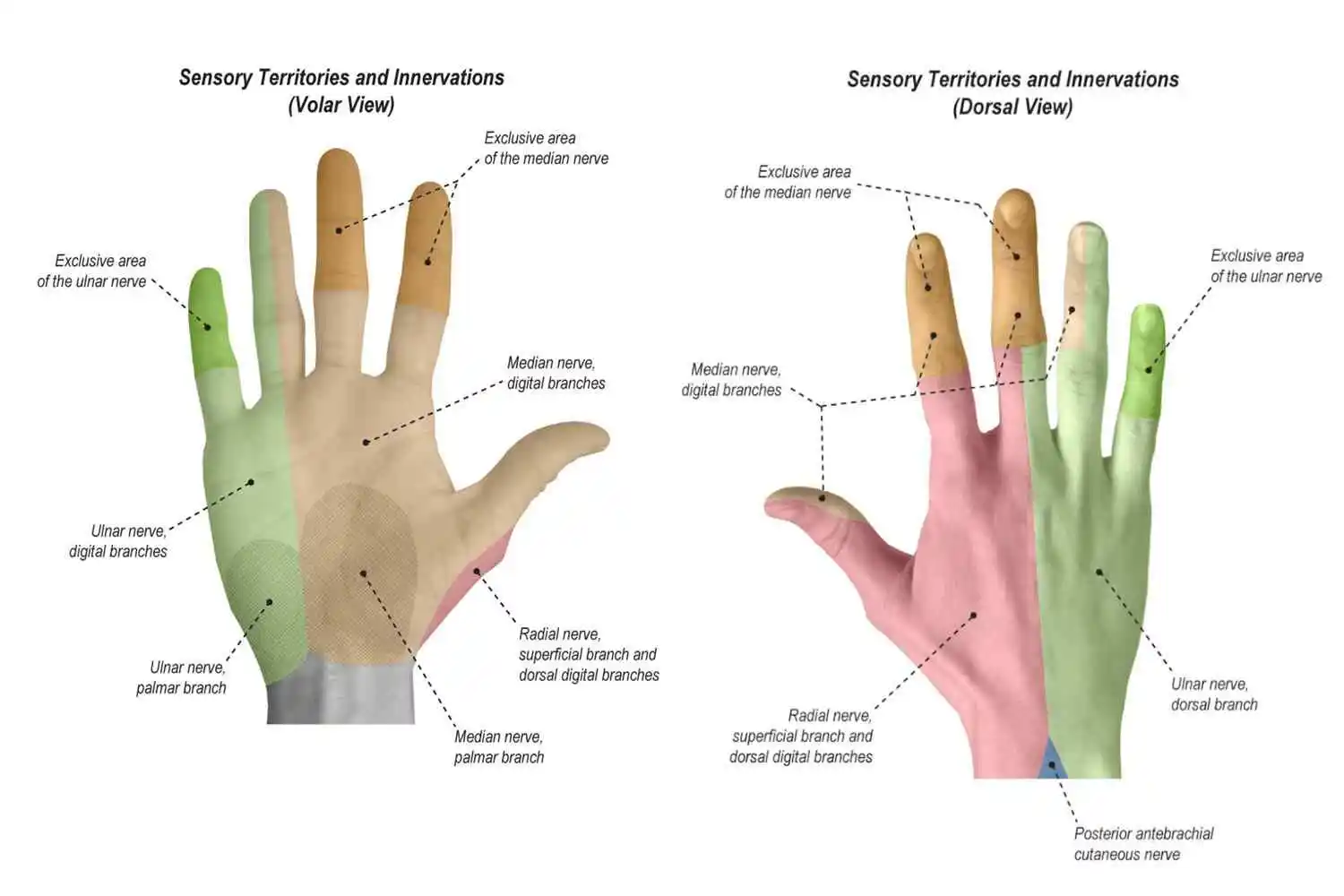
The sensations in the hand and wrist are primarily controlled by three major nerves:
- Radial nerve.
- Median nerve.
- Ulnar nerve.
All three nerves are connected to many branches of lesser nerves that run into your hand and wrist.
- 34 muscles in each hands.
- Thenar muscles
- The hypothenar region’s muscles
- Interossei muscles
- Lumbrical muscles
The following are a few of the most prevalent conditions that impact your hand and wrist:
- Carpal tunnel syndrome.
- Arthritis involves the hand or wrist, including osteoarthritis, and rheumatoid arthritis.
- Tendinitis.
- Trigger thumb or trigger finger.
- Dupuytren’s contracture
Characteristics of Swan neck deformity:
- A finger deformity known as Swan-Neck Deformity (SND) is primarily characterized by flexion of the distal interphalangeal joint (DIP) and hyperextension of the proximal interphalangeal joint (PIP).
- A metacarpal phalangeal joint (MCP) can show reciprocal flexion. The most frequent cause of a Swan-Neck deformity is an imbalance in a digit’s extensor mechanism.
- The deformity arises when the proximal phalanx’s intrinsic and extrinsic extensor mechanisms tighten at the proximal interphalangeal joint, or when the distal phalanx loses its extension.
Overview of Hand Rheumatoid Arthritis:
- Rheumatoid arthritis (RA) is a long-term inflammatory condition that impairs hand function and damages hand joints.
- Polyarthritis of the minor hand joints, including the wrist, second metacarpophalangeal (MCP), and first proximal interphalangeal (PIP) joints, is the most typical clinical manifestation of rheumatoid arthritis.
- Due to abnormalities that occur in about 90% of individuals with rheumatoid arthritis (RA), the hand is one of the primary components of therapy.
- There is a significant problem from a psychological and functional standpoint, linked to declines in muscle strength, restricted range of motion, and disapproval of limb form alterations.
- Specialized physical treatment may be available to adults with rheumatoid arthritis, with frequent evaluation.
Hand and Wrist Osteoarthritis:
- A frequent chronic illness that affects one or more thumb and finger joints is hand osteoarthritis (OA). This is associated to joint stiffness, discomfort, diminished grip strength, and loss of range of motion (ROM), which impairs hand function and makes daily tasks more challenging.
- The average incidence of symptomatic hand osteoarthritis is estimated to be between 13% to 26%, with a higher frequency in women.
The following is supported by evidence:
- For patients with osteoarthritis, prolonged usage of the night splint can significantly improve range of motion, discomfort, hand function, and strength.
- Hand function and grip strength can be improved with home workouts, joint protection programs, and coaching.
- The range of motion can be effectively increased with low-level laser therapy.
- There was no evidence that any rehabilitation techniques increased stiffness.
History:
Taking a complete medical history is a crucial first step in patient care. Although every physical therapist will have their unique style and approach, a successful interview will contain the fundamental components covered below:
- The injury’s mechanism What caused the damage, such as a fall onto an outstretched hand, and how it happened
- harm that is sudden or subtle.
- Handedness, occupation, history of fractures, and prior injuries
- Where the suffering is
- The existence and location of pins and needles, tingling, and/or numbness.
- Aggravating and alleviating elements.
- Functional restrictions.
- Did any imaging or diagnostic tests get done, and if so, what were the findings?
Examination:
Observation
Pain, redness (inflammation), swelling, elevated body temperature, deformity, neurological symptoms, and loss of function are the hallmarks of any joint disease. First, the damaged area will be visually observed by the doctor and compared with the opposite, unaffected side. Scars, irritation, lesions, asymmetry, deformities, and atrophy will all be detected by this. The doctor will look for any morphological changes in the hand and wrist anatomy during the initial examination, including:
- Rashes, scars, or other abnormalities
- Asymmetry
- Atrophy or deformity
- Anatomical variations about a healthy wrist
- Pain from extensor tendonitis in the dorsal region (back of the hand)
- Pain from flexor tendonitis in the volar region (palm)
- The condition of arthritis
Palpation
Examining every joint and group of muscles and locating any painful spots or deformities are all part of the touch of the compromised area. Palpation is used to detect anomalies, forms, and structures, as well as variations in tissue tension, texture, and thickness. Along with observing anomalous sensations like dysesthesia, reduced sensation, and heightened sensation, the examiner will also look for changes in temperature, tremors, and pulses. Anatomical markers such as the radial/ulnar styloid, scaphoid, lunate, TFCC, triquetrum, and other carpal bones up to the hand’s metacarpal bones will be identified with a mild wrist examination. The examiner will:
- Feel every major muscle group and joint.
- Determine any sensitive spots.
- Look for any abnormalities.
- Always make comparisons with the other viewpoint.
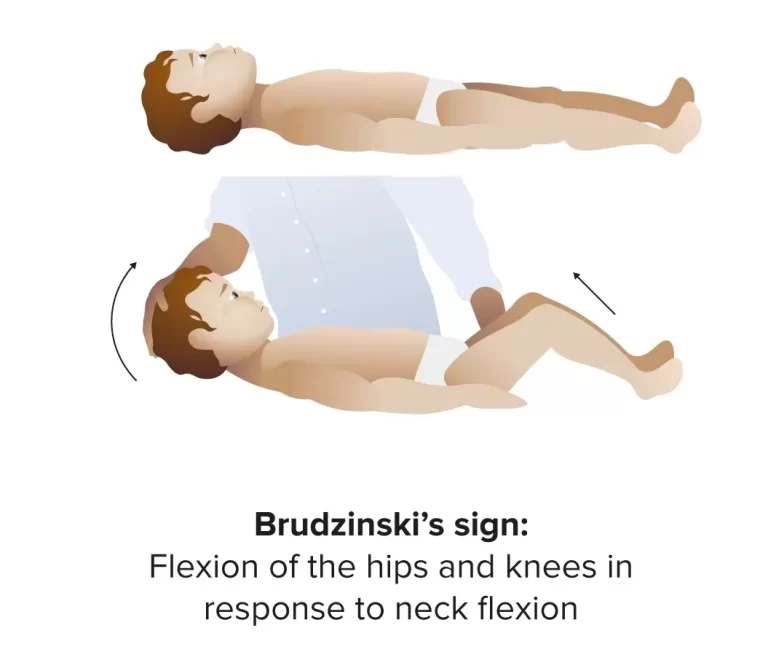
Evaluation of Neurology
- Upper Extremes Nerve Palpation: If the peripheral nerve entrapment condition is suspected, the objective is to replicate symptoms.
- To feel the three main nerves in the upper limbs
- Median: Place the patient in a supine position with their elbows extended and their shoulders abducted 90 degrees. Apply pressure medially to the mid-humeral bicep. Feel the wrist distally.
- Radial: distal radius, snuffbox, and upper arm (0 degrees in abduction, or feel proximal towards the lateral epicondyle).
- Mid-humeral upper arm: cubital tunnel, shoulder 90 degrees in abduction, elbow 120 degrees in flexion, and medial mid-humeral region
C5-C7 Reflexes - C5-T1 myotomes
- C5-T1 Dermatome
Motion range:
To assess any variations in function, instability, and pain level, the patient is encouraged to actively move each joint.
- Extension and Flexion
- Ulnar/radial abduction
- supination/Pronation
- Thumb flexion/extension
- Thumb abduction/adduction
- MCP joint
- PIP Joint
- DIP Joint
Examination of the Hand closely:
The dorsal side of the palm
Examine each hand’s dorsum with the patient’s palms facing down for any indications of underlying pathology: Take note of any irregularities in hand posture that can point to underlying disease, such as Dupuytren’s contracture or ulnar deviation caused by rheumatoid arthritis.
- Scars: look for signs of scarring, which could be a sign of prior trauma or surgery.
- Swelling: compare the hands and wrists to identify any regions of swelling.
- Skin color: soft tissue erythema could be a sign of joint infections or cellulitis.
The proximal interphalangeal joint (PIPJ) is home to Bouchard’s nodes, which are linked to osteoarthritis. - Heberden’s nodes are linked to osteoarthritis and are located at the distal interphalangeal joints (DIPJ).
- The distal interphalangeal joint (DIPJ) is the site of the Swan neck deformity, which manifests clinically as DIP flexion with PIP hyperextension. Rheumatoid arthritis is usually linked to Swan neck deformity.
- Z-thumb: fixed flexion and subluxation of the metacarpophalangeal joint (MCPJ) along with hyperextension of the interphalangeal joint. Rheumatoid arthritis is connected to Z-thumb.
- Boutonnières deformity: rheumatoid arthritis-related PIP flexion and DIP hyperextension.
- Long-term steroid use may be connected to skin thinning or bruising, which is prevalent in people with active inflammatory arthritis.
- Salmon-colored plaques that have a silvery scale are indicative of psoriatic plaques. Psoriatic arthritis is far more likely to occur in patients with psoriasis.
- Muscle atrophy may result from lower motor neuron lesions (e.g., median nerve loss due to carpal tunnel syndrome) or persistent joint pathology.
- Splinter hemorrhages are reddish-brown, longitudinal hemorrhages beneath nails that resemble wood splinters. Local trauma, sepsis, vasculitis, infective endocarditis, and psoriatic nail disease are among the causes.
- Onycholysis and nail pitting are linked to psoriasis and psoriatic arthritis.
The hand’s palmar aspect
Examine each hand for indications of underlying pathology with the patient’s palms facing up:
- Take note of any indications of abnormal hand posture, such as a clawed hand caused by Dupuytren’s contracture.
- Scars: look for signs of scarring, which could be a sign of prior trauma or surgery (e.g. carpal tunnel surgery).
- Swelling: compare the hands and wrists to identify any regions of swelling.
- A thickening of the palm fascia in Dupuytren’s contracture leads to the formation of cords of the palmar fascia, which ultimately results in contracture abnormalities of the thumb and fingers.
- Isolated atrophy of the thenar eminence, such as that seen in carpal tunnel syndrome, is indicative of injury to the median nerve.
- Examine the elbows for signs of rheumatoid nodules or psoriatic plaques.
- Janeway lesions are hemorrhagic, non-tender lesions that develop on the palms’ (and soles’) thenar and hypothenar eminences. Infectious endocarditis is usually linked to Janeway lesions. Osler’s nodes: usually found around the fingers or toes, this reddish-purple, slightly elevated, painful lumps frequently have a pale center. Infectious endocarditis is usually linked to them.
The purpose of functional tests:
- To measure and acquire the results for evaluation and reevaluation following an intervention, such as turning the doorknob, holding a key, initiating a pain-free grasp or even a key grip, opening a jar, or lifting a pot.
- Grip strength, which is expensively available online, might be a useful and dependable instrument to use.
Neurodynamic tests
Overview:
- A neurodynamic evaluation measures the length and movement of different nervous system components.
- These tests, separated into upper and lower limb tests, are carried out by the therapist applying increasing tension to a nervous system component under examination.
- The Elvey Test and Brachial Plexus Tension Test are other names for the Upper Limb Tension Test (ULTTs).
- The purpose of these tests is to stress the upper limb’s neurological structures.
- The wrist, fingers, forearm, elbow, and shoulder are held in various positions to create neural bias, or stress on a particular nerve. The position of every joint is also modified as a “sensitizer.”
- A ULTT is the counterpart of a straight leg lift designed for the lumbar region.
To check for median nerve impingement, do the Upper Limb Tension Test (ULTT1):
Signs:
- The upper limb that radiates, the sensation of tingling in the thumb, index finger, and middle finger, the initial three fingers.
Action taken:
- Shoulder depression.
- Shoulder rotates outward with elbow 90 degrees of flexion, abduction of the shoulder 110 degrees,
- Supination of the forearms
- Both wrist and finger extension
- Extension of the elbow.
- Differentiation in structure:
- Reduce pain in wrist and finger extension movement.
- Provocation includes: flexion of the neck in the opposite direction.
To check for median nerve impingement, do the Upper Limb Tension Test 2A (ULTT2A):
Signs of the examination:
- Upper limb pain that radiates,
- Instability, shoulder dislocation, and recent shoulder arthroplasty surgery.
Action taken:
- Shoulder girdle depression
- Shoulder abduction 100-degree
- External rotation at a 90-degree angle with the elbow
- Supination of the forearms
- Extension of the wrist, fingers, and elbows.
- Differentiation in structure:
- Proximal symptoms include relief from wrist and finger extension.
- Neck flexion in the opposite direction is one of the distal symptoms (provocation).
Test of Upper Limb Tension 2B (ULTT2B, screening for radial nerve compression):
Indications include Cervical Radiculopathy, De Quervain’s disease, Supinator tunnel syndrome, and radiating discomfort in the upper limb.
Action taken:
- Shoulder internal rotation, shoulder girdle depression, shoulder abduction of 20 to 30 degrees, forearm pronation,
- Flexion of the wrist, fingers, and thumb; extension of the elbow.
- Differentiation in structure:
- Proximal symptoms: Reduce flexion of the fingers and wrist.
- Neck flexion in the opposite direction is one of the distal symptoms (provocation).
Ulnar nerve compression is checked with the Upper Limb Tension Test 3 (ULTT3):
Signs include carpal tunnel syndrome, thoracic outlet syndrome, and pain that radiates to the fourth and fifth fingers.
- The following actions were performed: forearm pronation, wrist and finger extension, elbow flexion, shoulder girdle depression, abduction of the shoulder 110 degrees, and shoulder external rotation.
- Differentiation in Structure:
- Relieve wrist and finger extension as proximal symptoms.
- Neck flexion in the opposite direction is one of the distal symptoms (provocation).
Testing for Strengths:
- Bending and extending the wrists
- Supination and pronation of the forearms
- Grips strength
- Strength of key and pinch grips
Special tests:
Phalen’s carpal tunnel syndrome maneuver:
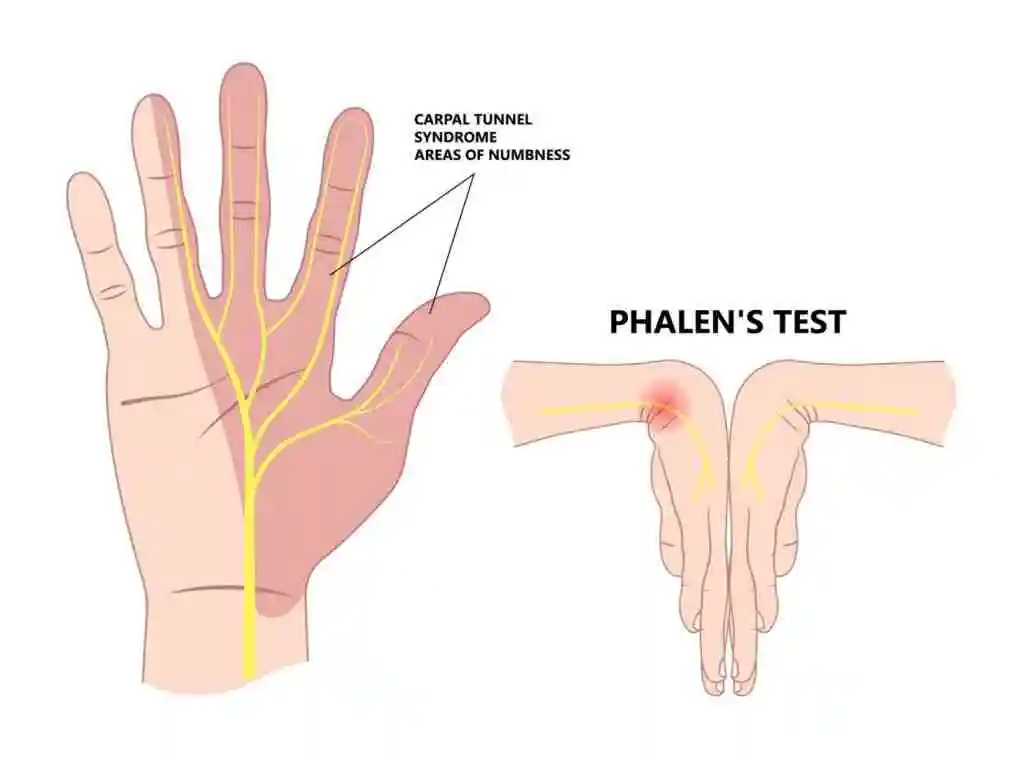
- Carpal tunnel syndrome is indicated if having the wrist flexed causes symptoms unique to the median nerve, such as tingling, pain, burning, and numbness in the thumb, index, and inner portion of the ring finger.
Tinel’s sign:

- It is used to demonstrate radial, ulnar, and median nerve dysfunction. The tester applies pressure to the wrist nerve by tapping or compressing it. A tingling sensation in the areas innervated by the particular nerve indicates a positive test.
- The thumb, index and middle fingers are the innervated regions of the median nerve.
Medial nerve compression test
- The test validates the identification of carpal tunnel syndrome if pins and needles are produced by squeezing the median nerve that is located at the posterior palm where the carpal tunnel start.
Ulnar nerve compression test
- Ulnar nerve injury is confirmed by pain or discomfort in the wrist, which encloses the ulnar nerve and artery is compressed.
Flick test
This test is mainly used for the carpal tunnel syndrome
- During this examination, the examiner forcefully shakes the patient’s hand. The test is positive if wrist shaking exacerbates symptoms of carpal tunnel syndrome.
Other tests:
Finkelstein’s test for De Quervain disease
- The examiner deviates the wrist to the ulnar side while the patient is holding the hand clenched in a fist. If the test is positive, there is a pain in the extensor pollicis brevis tendon.
Tests for instability:
Lunate-Triquetrum ligament (LT) shear test
- The examiner provides a force on the pisiform bone and the lateral wrist on the triquetrum bone while holding the wrist firmly with the thumb on the palmar side. When manipulation results in pain or increased translation relative to the healthy side, the diagnosis of a Lunate-Triquetrum (LT) ligament injury is confirmed.
TFCC Stress Test:
- The TFCC Compression Test is another name for this. Moving the affected wrist into ulnar deviation and applying a shear or stress force to replicate the discomfort is part of the TFCC (Triangular Fibrocartilage Complex) stress test.
Sharpey Test:
- The examiner securely grasps the proximal carpal row and distal radioulnar joint. Next, exert a compressive force on the distal radio-ulnar joint using the carpus. Then, in both pronation and supination, provide a rotating force. At the TFCC, discomfort or clicking indicates a positive test.
Sign of a scaphoid fracture:

- Several clinical indicators associated with a scaphoid fracture are evaluated by the instability test, including pain and edema around the scaphoid region, soreness in the anatomical snuffbox, discomfort upon axial compression, and pain when the hand is pronated and pinched.
Murphy’s Sign:
- The examiner’s evaluation of the dorsal aspect of the hand indicates that the lunate has dislocated if the middle finger’s knuckle, the third metacarpal bone, matches the knuckles on the second or fourth metacarpals.
Watson test or Scaphoid shift test for wrist injuries fracture of the scaphoid tubercle:
- Scapholunate instability is detected using the Watson test. The examiner applies pressure while placing the thumb over the patient’s scaphoid tubercle. After that, the wrist is moved from its ulnar to radial position. When the patient feels pain or hears a clunk, the test is considered successful.
Distal radio-ulnar joint instability test :
- The examiner rotates the ulna with a lateral plane while holding the wrist over the radial side. The diagnosis of DRUJ instability is confirmed by clicking, popping, or discomfort.
Froment sign

- Testing for motor weakness of the ulnar nerve
- The patient was instructed to place a piece of paper between their thumb and index finger’s radial side.
- The patient tries to hang onto the paper while the examiner pulls it away by bending their IP joint.
Wartenberg sign:
- Ulnar nerve motor weakness tests
- The patient was instructed to maintain fully adducted fingers with fully extended MCP, PIP, and DIP joints.
- It is preferable if the little finger shifts and moves into abduction.
Durkan’s Test:
- Durkan’s test is probably superior, even though Phalen’s and Tinel’s are frequently taught. The carpal tunnel examination or medial nerve compression exam are other names for this screening method.
- To blanch the skin, direct pressure must be applied on the median nerve of the carpal tunnel for an extended period. Usually, this takes around 30 seconds. A repeat of the symptoms indicates a positive test.
Red Flags:
In this segment, the patient is screened for potential significant disorders that may be causing pain in the hand or wrist. These conditions might call for a consultation or referral.
- Redness, Pain, Swelling, and Heat
- The inflammation
- Breakage or displacement:
The top five examination results that are most helpful in wrist fracture screening. Discomfort with active movement, discomfort with passive movement, pain on grasp, pain on supination, and localized soreness
Other possibly dangerous circumstances
- Instability of scapholunate
- Arthritis
- Rheumatoid Arthritis
- Lyme illness
- The tuberculosis
- Peripheral Vascular Disease
- peripheral neuropathy
- Trauma history, fall on the outstretched hand (FOOSH). Older than 65. Both men and women are at the same risk.
- Nerve damage to the upper extremities involving the median, radial, and ulnar nerve.
FAQs
Which tests are specific to wrists?
Watson test or Scaphoid shift test for wrist injuries fracture of the scaphoid tubercle. Scapholunate instability is detected using the Watson test. The examiner applies pressure while placing the thumb above the patient’s scaphoid tubercle. After that, the wrist is moved from its ulnar to radial position.
What is a wrist?
The joint at the extremity of the forearm is called your wrist. You can move your hand around thanks to the hinge that connects your arm and hand. Where your wrist finishes is where your hand starts. It consists of your thumb, fingers, and palm.
How many wrist bones are there?
Your wrist comprises eight little bones (carpal bones) and two long bones (ulna and radius) in your forearm.
Which eight carpal bones are there?
Between a metacarpal base distally and the distal radius and ulna (with the intervening TFCC) proximally, the eight carpal bones—scaphoid, lunate, triquetrum, pisiform, hamate, capitate, trapezoid, and trapezium—are organized in two rows.
How many joints does a hand have?
27 bones, 27 joints, 34 muscles, more than 100 ligaments, and tendons, as well as a large number of nerves, blood vessels, and soft tissue, make up the complex anatomy of the hand. If we are to learn about illnesses and problems that can affect the hands, it is crucial to comprehend the typical structure of the hand.
Finkelstein: What is it?
It is a straightforward test that may be carried out at the patient’s bedside or in an office to diagnose De Quervain’s disease. If a thumb is flexed into the palm and the wrist is ulnarly deviated, Finkelstein’s test results in extreme soreness and typically pain at the radial side of the wrist.
Reference:
- Professional, C. C. M. (2024, August 6). Anatomy of the hand and wrist. Cleveland Clinic. https://my.clevelandclinic.org/health/body/25060-anatomy-of-the-hand-and-wrist
- Wrist hand examination. (n.d.). https://examination.lexmedicus.com.au/collection/wrist-hand
- Wrist hand examination. (n.d.-b). https://examination.lexmedicus.com.au/collection/wrist-hand#:~:text=Watson%20test%20is%20used%20to,a%20clunk%20noise%20is%20heard.
- Kiel, J. (2023, September 25). Special tests for the wrist exam. Sports Medicine Review. https://www.sportsmedreview.com/blog/special-tests-for-the-wrist-exam/
- Sheth, U., MD. (n.d.). Physical exam of the hand – hand – orthobullets. https://www.orthobullets.com/hand/6008/physical-exam-of-the-hand
- Wilhelmi, B. J., MD. (n.d.). Hand Anatomy: Overview, Bones, skin. https://emedicine.medscape.com/article/1285060-overview?form=fpf