Tarsal Tunnel Syndrome
Introduction
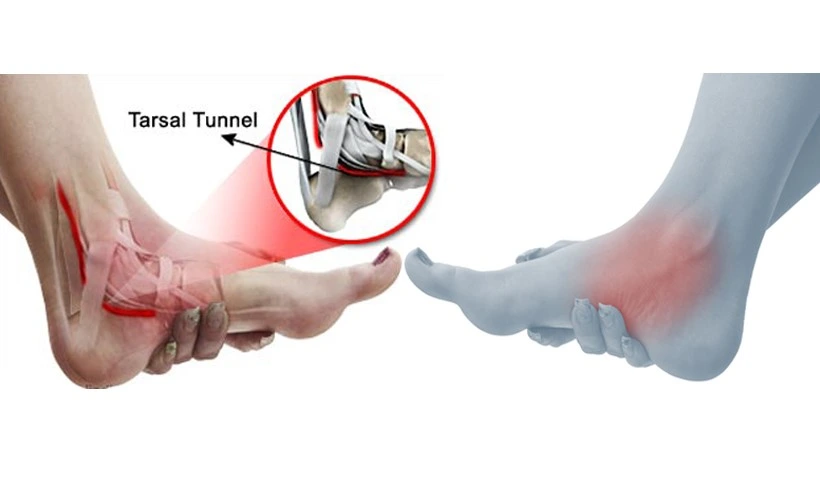
Tarsal Tunnel Syndrome is a condition caused by compression of the posterior tibial nerve as it passes through the tarsal tunnel, located along the inner ankle. This can lead to symptoms like pain, tingling, numbness, or burning sensations in the foot and ankle. Early diagnosis and treatment are essential to prevent long-term nerve damage.
The band of ligaments that runs across the foot and the ankle bones combine to create the tarsal tunnel, which is situated inside the ankle. Numerous blood arteries, nerves, and tendons traverse the tarsal tunnel, which gives the foot its mobility and flexibility.
Tarsal tunnel syndrome: What is it?
The disorder known as tarsal tunnel syndrome (TTS) is caused by a damaged or compressed tibial nerve. The nerve in your ankle is called the tibial nerve. It passes via your ankle’s tarsal tunnel, a passageway composed of ligaments and bones.
TTS patients may experience foot pain, tingling, numbness, or weakness. TTS may occur as a result of excessive foot and ankle use. Excessive or regular activity increases your risk of developing TTS, particularly if you have a very flat foot.
The tunnel is located beneath the flexor retinaculum, posterior to the ankle’s medial malleolus. Walking (or other weight-bearing activities) typically worsens the pain that radiates into the foot. An examination may indicate atrophy and weakness of the small foot muscles, loss of sensation in the foot, or Tinel’s sign over the tibial nerve near the ankle.
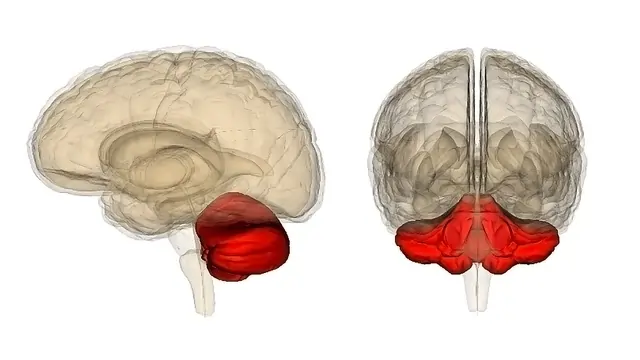
Relevant Anatomy
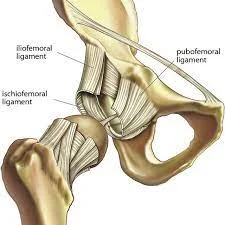
The flexor retinaculum, a fibrous sheet that extends from the medial malleolus to the calcaneus, is a tarsal tunnel that connects the talus, calcaneus, medial malleolus, and calcaneus.
The tunnel contains:
- Tibialis posterior tendon
- Flexor digitorum longus tendon
- Posterior tibial artery & vein
- Tibial nerve (yellow in the image)
- Flexor hallucis longus tendon
As the tibial nerve travels through the tarsal tunnel, it splits into two terminal branches, the medial and lateral plantar nerves. At or above the flexor retinaculum, the tibial nerve gives rise to the medial calcaneal nerve.
A uncommon compressive neuropathy of the tibial nerve or one of its branches as they pass beneath the flexor retinaculum is known as Tarsal Tunnel Syndrome (TTS).
TTS is also known as Posterior Tibial Nerve Neuralgia, and the tibial nerve is also called the posterior tibial nerve in the literature on TTS. “Anterior tarsal tunnel syndrome” is the term used by certain authors to describe compression of the deep fibular nerve. Only the topic of tarsal tunnel syndrome—the entrapment of the posterior tibial nerve or its branches—is covered on this page.
Epidemiology
Any type of compression or entrapment of the tibial nerve or its plantar branches results in Tarsal Tunnel Syndrome. The reason is frequently posttraumatic or idiopathic. 20–40% of cases were thought to be idiopathic. The following conditions account for up to 10% of all cases: rheumatoid arthritis, tenosynovitis, and arthrosis. Convoluted vessels are present in about twice as many cases as the origin.
Other uncommon causes include mucopolysaccharidoses, gout, diabetes mellitus, hypothyroidism, and (very infrequently) hyperlipidemia.
- Due to their assisting nature or hypertrophy, certain muscles or tendons located medially to the talus bone may trap the tibial nerve. Along with blood vessels, the tibial nerve, and other muscles, the tendon of the flexor hallucis longus muscle passes via the tarsal tunnel, as was indicated in the “anatomy” section. The pressure inside the tarsal tunnel rises when one of these muscles experiences sufficient hypertrophy. This can occasionally, although it comes before the flexor hallucis longus muscle belly’s entrance into the tarsal tunnel. Over stimulation of the tibial nerve or its branches may result from this. The patient may have a variety of unpleasant feelings in their foot, depending on which nerve is being impinged.
- These deviations from the routine may be more harmful than helpful. Even though such muscles aren’t always useful, they take up space in the foot. This can compress the tibial nerve, which may lead to chronic pain, much to the over growth of the muscles in the medial ankle region.
- Localized swelling and inflammation caused by surgery or an overload on the ankle region can put pressure on the tibial nerve once more. It has been demonstrated that sports involving a lot of running and jumping are stimulating for TTS. The syndrome is more likely to develop in those who have flat feet, union talocalcaneal, or bone fragments surrounding the tarsal tunnel.
- Given that tarsal tunnel syndrome is a rather uncommon clinical condition, it may be worth noting that clinicians frequently misdiagnose it in both adults and children because of their low index of suspicion. Mostly in adults, the prevalence would be higher in females than in males. Additionally, athletes and those who endure extended weight-bearing activities, such as standing, walking, or vigorous physical activity, are more likely to experience TTS. The anatomical components within the tarsal tunnel may be compromised by pes planus deformity or hyper pronation, which could result in a physical reduction of space and an increase in nerve strain. It would rank among the most frequent external factors contributing to TTS.
Wearing loose-fitting shoes and resting or neutrally immobilizing the foot and ankle could help reduce pain and complaints. The most common cause is thought to be external compression from tight plaster casts or shoes.
Causes
Tarsal tunnel syndrome occurs when your tibial nerve is damaged. Damage to the tibial nerve may result from the following:
- Flat feet.
- High arches.
- Injuries such as a broken or fractured ankle.
- Swelling from an ankle sprain or fracture
- Bone spurs
- Inflammation from a disease like arthritis
- Varicose veins
- Overuse injury
- Diabetic neuropathy, a complication of diabetes
- Tumors near your tibial nerve
Conditions like diabetes or arthritis that can lead to swelling and nerve compression
- Abnormal growths, like ganglion cysts, bone spurs, or varicose veins.
- Abnormal growths like lipomas or tumors located in proximity to your tibial nerve.
- Systemic conditions affecting the entire body, like hypothyroidism, diabetes, or arthritis.
In many cases, tarsal tunnel syndrome is a result of an overuse injury. Ankle sprains are among the injuries that more than two out of five individuals with tarsal tunnel syndrome have experienced. An injury to the ligaments in your ankle is referred to as a sprained ankle.
Symptoms of tarsal tunnel syndrome
The posterior tibial, lateral plantar, and/or medial plantar nerve distributions may experience paresthesia (burning, numbness, or tingling) as a common symptom of TTS (see picture). There may be localized pain behind the medial malleolus, as well as burning, tingling, or pain in the medial part of the ankle and/or plantar aspect of the foot.
When the foot is forced to evert and dorsiflex, the symptoms typically get worse. Patients may experience a stabbing sensation in the medial sole when walking if the medial plantar nerve is injured alone. This is typically observed in middle-aged runners. Muscle weakening of the toe flexors and abductors may be evident in a chronic or advanced disease. Muscle atrophy may be observed in more severe cases. Additionally, patients may complain of pain at night that keeps them awake and pain when they move for extended periods.
Nerve pain is a symptom of tarsal tunnel syndrome. The inside of your ankle or the bottom of your feet are typically where TTS produces pain.
Besides, you may come across:
- Burning sensations.
- Numbness.
- Tingling or “pins and needles” sensations.
- Weakness in your foot muscles.
Symptoms frequently get worse during or after exercise. You can have constant symptoms if your TTS is severe or persistent.
Diagnosis
TTS is mostly diagnosed clinically with a thorough medical history and clinical examination. Most of the clinical tests that physiotherapists conduct are thought-provoking. These will be covered in more detail under the “Examination” topic. Electrophysiological investigations and adjunctive medical imaging may help with diagnosis and offer more data that can be used to manage the condition. Computed tomography, radiography, ultrasonography, MRI, and electrodiagnostic investigations are a few examples of this.
For instance, in some long-term conditions, the digital abductor and flexor muscles of the affected foot may weaken, atrophy, or even paralyze. Since it is frequently challenging to identify clinically, further referrals for medical imaging or nerve conduction investigations may be necessary.
Although these tests can be very helpful in verifying or dispelling a doctor’s concern, we must remember that they cannot replace a clinical examination.
X-Ray
As was previously indicated, it can be difficult for clinicians to determine the etiology of TTS and many other medical ankle and heel pains based just on physical examination. This is because it is challenging to pinpoint symptoms to a particular component because of the intricate architecture of the medial portion of the ankle and hindfoot. Ankle plain X-rays, for instance, can be used to show structural anomalies such as hindfoot varus/valgus. When examining space-occupying lesions, magnetic resonance imaging (MRI) provides additional detail and has an 83 percent accuracy rate.
MRI
When it comes to detecting probable tarsal tunnel compression caused by the presence of obstructive foreign bodies, lesions, or tumors, magnetic resonance imaging (MRI) is the gold standard. This kind of imaging not only verifies the existence of a suspected lesion but also accurately characterizes it by defining its depth, extent, and edges. According to Frey’s study, 88% of tarsal tunnel candidates with symptoms had substantial MRI results, which helped with etiological reasoning and, if necessary, surgical planning. The thickness of the flexor retinaculum, the overall depth of the tarsal tunnel, and its contents, including the posterior tibial nerve cross-sectional area and its terminal branch derivatives, can all be detected and demonstrated by MRI and high-resolution ultrasonography.
Ultrasound
For the evaluation of medial ankle and heel pain, ultrasound is a convenient, portable, and reasonably priced imaging method (less expensive than MRI). It also has the benefit of being comparable to the contralateral side. Ultrasound is useful in diagnosing pathologic disorders affecting the medial ankle and heel and correlates well with MRI, even though MRI (above) is still the gold standard. The full path of the tibial nerve and its branches at the medial ankle, as well as the intricate structure of the tarsal tunnel, may be seen on ultrasound. Additionally, it works well for identifying lesions that take up a lot of space. In patients with symptoms, ultrasonography can identify even minute alterations in the nerve’s cross-sectional area.
Electrodiagnostic testing
Tarsal tunnel syndrome can also be diagnosed with the help of electrodiagnostic testing. These tests include nerve conduction studies that measure the amplitude and duration of motor-evoked potentials, as well as the sensory conduction velocities of the tibial nerve or one of its branches.
The great sensitivity and specificity of the electrophysiological approaches in TTS are demonstrated by a small number of high-quality, evidence-based studies. The more sensitive markers of disease are a motor response with a reduced amplitude and a longer duration. These tests, which regrettably frequently provide an intolerable number of false-negative results, ought to be used as a supplementary evaluation to support the results of physical exams.
A diagnostic assessment of Tarsal tunnel syndrome might include:
Tinel’s test:
- Percussion of the tarsal tunnel results in distal radiation of paresthesia
- Elicited in over 50% of those affected
Your doctor taps your tibial nerve lightly. TTS may be indicated if you have pain or tingling that mimics your symptoms.
Dorsiflexion – Eversion Test:
- Put the patient’s foot into complete dorsiflexion and eversion, maintaining this position for 5 to 10 seconds.
- The outcome is that it provokes the symptoms the patient has.
Differential Diagnosis
Since these patients also have plantar heel pain, plantar fasciitis is the most common differential diagnosis for TTS, which can appear similarly to other lower extremity illnesses. Apart from Plantar fasciitis (where TTS is believed to be frequently misdiagnosed), other conditions that need to be differentiated from tarsal tunnel syndrome include polyneuropathy, L5 and S1 nerve root syndromes, Morton metatarsalgia, and compartment syndrome of the deep flexor compartment. Posterior Tibialis Tendon Dysfunction is the most frequent cause.
- Neuropathy: Most people have experienced paresthesia, sometimes known as the “sleeping limbs” sensation. A pathological condition like polyneuropathy may also cause this sensation to increase. At that point, the patient is unable to control the numb, tingling sensation. This condition frequently affects the hands or feet. Given that one has foot paraesthesia, the symptoms closely resemble those of TTS.
- Ischemia: Ischemia is a lack of oxygen reaching the tissue. Long-term suspension of this supply may result in irreversible harm. Nerve function gradually deteriorates when oxygen levels drop. Extended ischemia can have disastrous consequences. Damage may be minimal, though, if the cause—a lack of blood flow—is remedied over time. Permanent ischemic paresthesia can occur in certain nerve-related situations. The neurons fire randomly as a result, producing the same sensation as TTS symptoms.
- Compartment Syndrome: This condition primarily affects the lower leg and upper arm. It may manifest with a build-up of pressure on or within a muscle compartment; fluid accumulation or an overabundance of specific muscle groups may be the cause of this syndrome. The deep calf muscles contain a compartment where the tibial nerve runs. This nerve may fire wildly if there is too much pressure applied. If the majority of the nerve compression occurs close to the medial malleolus, the TTS may be mistaken for this compartment syndrome. It has also been demonstrated that the former can result in a lesion of the distal tibial nerve. Any damage or unusual alteration to tissue is called a lesion. A nerve’s ability to function can be compromised by a lesion in or close to it. Therefore, when a nerve close to the medial malleolus is affected, it can mimic the same symptoms as the TTS.
- A tumor: It can be benign, precancerous, or malignant, and it is defined as a collection of cells that grow out of control. The fact that they occupy unnecessary space unites them notwithstanding these three differences. Tumor pressure rarely causes problems for the tissues around the tumor. However, if it overexcites a nerve in the medial malleolus, it may be a differential diagnosis for TTS.
Other differential diagnosis
- Polyneuropathy
- L5 and S1 nerve root syndromes
- Morton’s Metatarsalgia
- Compartment Syndrome of the deep flexor compartment
- Calcaneal spurs, arthrosis, and inflammation of the fasciae and ligaments
- Ischemia
- Infection
- Lesion
- Tumor
- Plantar fasciitis
Treatment
Medical Treatment
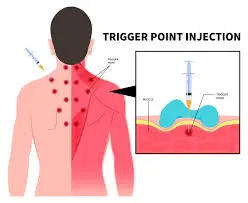
To enhance recovery and reduce functional disability, pharmacological treatments are frequently combined with physical therapy management.
- NSAIDs
- Corticosteroid Injections
- Pain Medications
Anti-inflammatory drugs or steroid injections into the tarsal tunnel to reduce swelling and pressure are examples of nonsurgical treatments for TTS. Splints, braces, and other orthotic devices can assist in limiting movement that could compress the nerve and relieve pressure on the foot.
Physical therapy treatment
Finding practical rehabilitation exercises or alternative treatments for people with tarsal tunnel syndrome would be aided. Patients are referred to a clinician for a surgical technique (such as tarsal tunnel decompression) if they do not improve with physical therapy or other conservative measures.
Orthotics and taping
- UCBL orthosis: This type of orthosis, developed by a laboratory at the University of California Berkeley, serves to enhance alignment of the hindfoot.
- CAM walker: Controlled ankle motion walker, the ROM of the patients’ ankle can be altered with this boot.
- Patient education regarding footwear: it is the therapist’s responsibility to inform the patient about wearing suitable footwear. It is best to avoid shoes that fit tightly. With athletes, it is important to consider their running mechanics and/or technique motions (specific to the sport) that could be responsible for the symptoms.
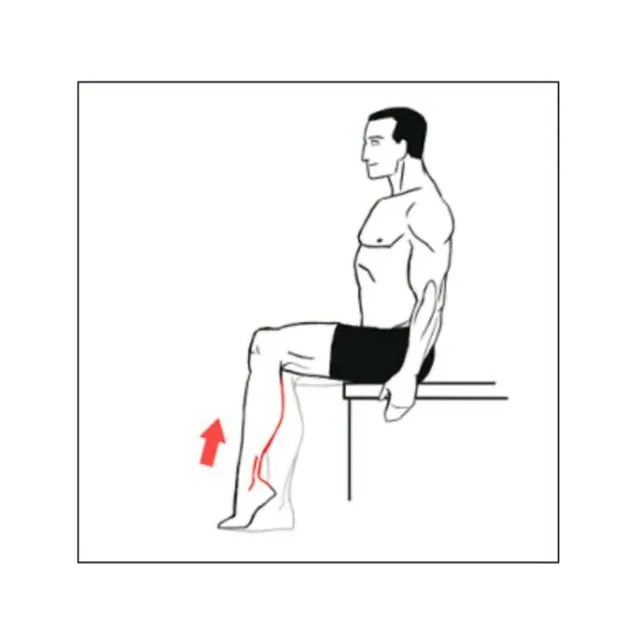
Ankle Resistance Exercises
Exercises that provide resistance to the ankle are crucial for fortifying the structures of the ankle. Movements should be voluntary and progressive. Pain should range from mild to moderate. Pain indicates that you should take a break and rest.
Ankle Inversion

- Start on the floor in a seated position, with your right leg extended in front of you.
- Secure one end of a closed elastic resistance band to a stationary object, positioning it toward the outer side of your foot.
- Wrap the other end around the top of your bent foot. Now, rotate your foot inwards against the resistance of the band and go back to the initial position.
- Make 1–2 sets of 10 reps with each foot.
Ankle Dorsiflexion

- Next, position the resistance band on your foot at the level of your toes, but a little lower down.
- Connect the other end to a stationary object that is directly in front of you.
- A leg from a chair or table works well. Gently draw your foot back towards your head, then let it relax forward and downward.
- Make 1–2 sets of 10 reps with each foot.
Ankle Plantarflexion
- Go back to sitting. Grip one end of the resistance band and loop the other around the bottom of your right foot.
- Press your foot down as if you were pushing a gas pedal, then gradually bring your foot back to the neutral position.
- Make 1–2 sets of 10 reps with each foot.
- This action also elongates the plantar fascia, which extends from the heels to the toes on the foot’s underside and is often a source of foot pain and inflammation.
Ankle Rotation
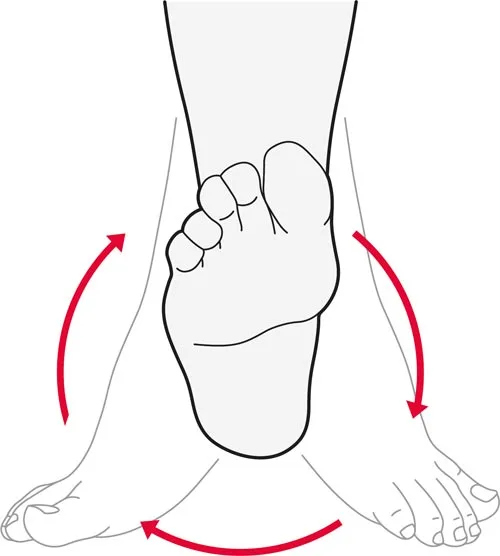
- By enhancing the ankle joint’s range of motion, ankle rotations help prevent injuries that may lead to nerve compression or damage.
- Begin while sitting on a chair. Raise your right leg a few inches above the ground and rotate your ankle 5 times in a clockwise direction, followed by another 5 rotations in the same direction.
- Put the right foot down. Make 1–2 sets of 10 reps with each foot.
Pencil Pick-Up
- This exercise serves as an alternative means of fortifying the muscles that support the tendons in the tarsal tunnel.
- Begin in either a seated or standing position. Put a pencil on the floor before you. Additionally, a marble or small hand towel can be used.
- With your toes, grab the item and keep it for 10 seconds before returning it to the floor.
- Perform this action 3–5 times for each foot.
Tibialis posterior strengthening

The tibialis posterior muscle serves to support the ankle and is also involved in ankle inversion. Weight-bearing and non-weight-bearing exercises are the two types of exercises.
Calf muscle Stretching

- The calf muscle can be stretched in a variety of ways, but the wall stretch is one of the most popular methods. The gastrocnemius muscle is stretched in the first image, and the soleus muscle is stretched in the second.
Soleus Stretch

Located at the back of the lower leg is the soleus muscle. Muscle weakness and/or tightness in this area, as well as in other muscles of the lower leg and foot, can play a role in the development of TTS. To perform a soleus stretch, position your right foot approximately 5 inches away from the wall in a staggered stance (with your left foot behind).
While maintaining contact with the floor with your right heel, attempt to bring your knee to the wall or until you experience a slight stretch in the back of your right lower calf. Maintain the stretch for 45 seconds, doing it 3-4 times on each side.
Achilles tendon Stretching
Runner’s stretch:

The Achilles tendon may become tight and uncomfortable when it is inflamed. By relaxing the tendon, the runner’s stretch, also known as the calf stretch, will offer relief. You’ll need a wall or some support, such as a chair, to perform this exercise.
- Put your hands on a chair or the wall. Place your hands at eye level if you’re using a wall.
- The leg you wish to extend behind you should be stepped. Keep your back heel on the ground and point your toes straight ahead.
- With your back leg straight, bend your other knee toward the wall.
- Until your calf begins to gently stretch, lean in the direction of the wall. Make sure that you don’t lean to the extent of causing pain.
- Wait 30 seconds. Finish three repetitions.
Try a runner’s stretch with your knees bent if you have trouble straightening your leg. Bend your back knee until you feel a stretch, starting closer to the wall. Repeat three times while holding for thirty seconds.
Toe-to-wall stretch:

If the runner’s stretch causes pain in your shoulders, the toe-to-wall stretch is the best option. The upper body is under less pressure. Similar to the runner’s stretch, this exercise improves mobility by lessening Achilles tendon stress. Use the leg that is hurting to perform these steps.
- Place your toes up against the wall while standing with your back to it. The more intense the stretch, the higher your toes should be positioned.
- Maintaining your heel on the ground, bend forward. (The second leg is behind you, heel down, toes forward.)
- Wait 30 seconds. Finish three repetitions.
Heel drop:
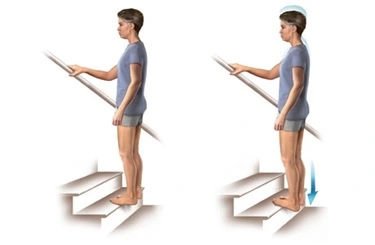
The heel drop is an additional Achilles tendon stretch. You can perform it on a stepladder or a staircase. Make sure the stepladder is fastened in place before using it. Use the leg with the Achilles tendon problem to perform this stretch.
- Cling to the stairway or ladder railings.
- Place your foot’s ball on the bottom step’s edge.
- Allow your other foot to relax by letting your heel drop.
- Wait 30 seconds. Finish three repetitions.
- Do this exercise under a provider’s supervision if you struggle with balance.
Tendo Achilles Stretching advice
The most effective way to relieve your Achilles tendon is by stretching it regularly. Even if you don’t feel stiff or sore, you should still stretch.
Keep these pointers in mind to maximize the benefits of every stretch:
- Go slowly. Whether you’re shifting positions or delving into a stretch, proceed slowly. This will reduce the possibility of pain and harm.
- Don’t bounce. Achilles tendon problems can only increase if you move quickly and abruptly. Throughout each stretch, maintain your composure.
- Don’t lift your heel. Plant your heel on the floor while performing a calf stretch. The Achilles tendon won’t stretch correctly if you elevate your heel.
- If you experience pain, stop. Relax after stretching until you experience very slight pain.
Plantar fascia Stretching

- Cross your affected leg over your other leg to test your plantar fascia.
- Grab your affected foot with the hand on your affected side, then draw your toes back toward your shin. The plantar fascia and foot arch are strained or stretched as a result.
- Gently brush the thumb of your unaffected side across the arch of the affected foot from left to right to determine the proper stretch position. Like a guitar string, the plantar fascia should feel firm.
- For ten counts, hold the stretch. Ten repetitions make up a set.
Calf strengthening exercises
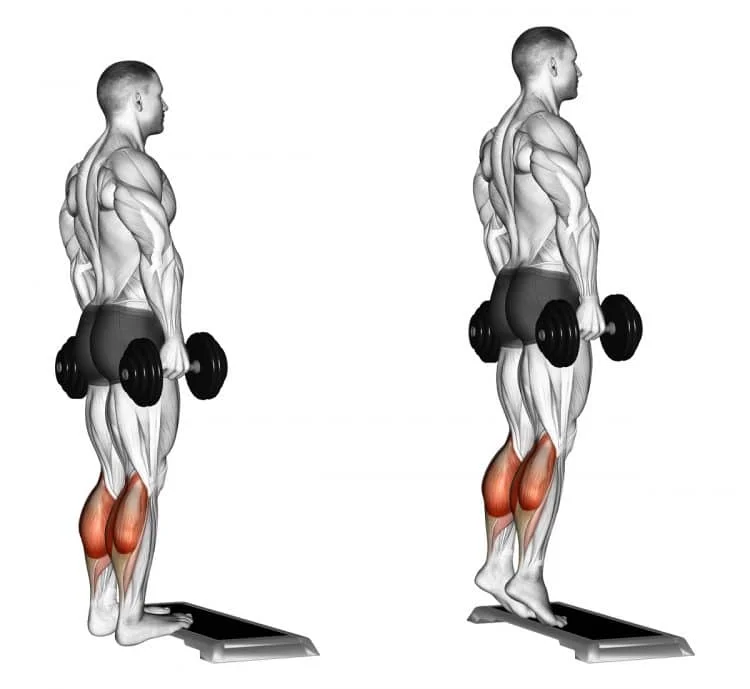
Additionally, you might work on strengthening your heel and calf muscles. Maintaining the strength of these muscles is crucial since they are connected to your Achilles tendon. It will lessen the tendon’s stress and stop further issues.
You can improve your Achilles tendon by performing muscle-strengthening workouts.
Seated heel raises
Your calf muscles cooperate to raise your heel when performing seated heel raises. This strengthens the Achilles tendon and gives it support.
- Take a seat at the edge of a bed or in a chair. Your feet should be shoulder-width apart.
- Raise your heels as high as you can, then take a moment to drop them gradually.
- Perform 20 to 25 repetitions in a single set. Repeat it five to six times daily.
Standing heel raises

You can perform heel lifts while standing up if it is comfortable. Additionally, this variant works the muscles that are connected to your Achilles tendon.
- Place your feet shoulder-width apart as you stand. For stability, cling to a chair or counter top. Raise yourself onto the balls of your feet by lifting your heels. After pausing, gradually drop your heels.
- Perform 20 to 25 repetitions in a single set. Carry this out five to six times daily.
Resistance band calf exercise

A resistance band is another tool you may use to strengthen your heel and calf muscles. By making these muscles work against resistance, this exercise helps to strengthen them.
Begin by using a band with minimal resistance. You can use a thicker, more resistant band as your tendon strengthens.
- Take a seat on a bed or the floor.
- Bend your knee a little and wrap a resistance band around the ball of the foot you wish to stretch. Use your hands to hold the ends.
- Point your foot away from you, pause, then let go.
- Perform three sets of 10–15 repetitions.
Nerve gliding
Carpal tunnel syndrome, or nerve entrapment in the wrist, has been treated using nerve mobilization exercises, although the outcomes have been mixed. There are very few case studies in the current literature that describe the use of nerve mobilization exercises to treat plantar heel pain that has a neurological basis.
An essential component of tarsal tunnel syndrome treatment is a nerve gliding exercise. Recent study indicates that these activities can help persons with tarsal tunnel syndrome with their pain and function, but more research is required. They lessen tarsal tunnel edema and pressure, promote circulation, and avoid nerve adhesions.
- Pull one knee into your chest while lying on your back to make your hips 90 degrees. The opposite leg should remain upright on the ground.
- Lift your leg and extend it as straight as you can. A small bend in your knee is acceptable.
- Now point your foot after flexing it and holding it for a few seconds.
- Return to the beginning position by bending your knee.
- Do this five to ten times.
- Repeat with the opposite leg.
Towel scrunches
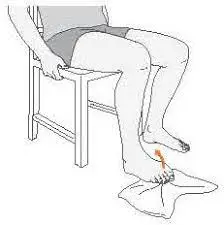
By strengthening your foot and ankle muscles, the towel scrunch exercise aids in maintaining stability and good alignment.
- Place a towel under your foot on a hard floor while seated in a chair.
- Scrunch the cloth toward you with your toes while maintaining a steady heel.
- Push the towel back out with your toes.
- On each side, repeat three to five times.
Single leg balance
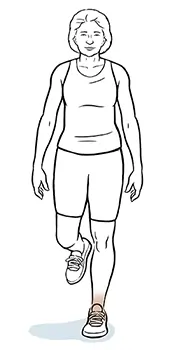
Ankle stability can be improved with balancing exercises like the single leg balance. Proprioception, or the awareness of the location of your body parts in space, is aided by them. Your body regulates your ankle’s position in this way, reducing the risk of further injuries.
- Stand close to a chair or other sturdy object so you may grab onto it if necessary.
- Elevate your foot on the other side to gain balance on the impacted side.
- Take ten to fifteen seconds to stand on one foot. Increase to 30 seconds gradually.
- Continue on the opposite side.
- Do this two or three times on each side.
- To make balancing more difficult, you might turn your head or close your eyes.
Other treatment
- Rest
- NSAID’s
- Corticosteroid injections
- Extracorporeal shockwave therapy
- Laser
- Local anesthetic injections
- Heel pads and heel cups
- Night splints
- Medial longitudinal arch supports
- Strapping
- Soft-soled shoes
- Casting
Before undergoing surgery, patients should get conservative treatment. Patients should be referred to a clinician if the conservative treatment is ineffective or if there are indications of atrophy or motor involvement.
Surgical treatment
Patients who have problems that substantially interfere with their everyday lives and who have not responded well to conservative therapies like physical therapy should consider surgery. Surgery is frequently necessary for people with space-occupying lesions because they rarely respond to conservative treatment.
A favorable reaction to surgery has been linked to several traits that Gorges and Kingman have discovered. Younger age, a brief history of symptoms, no prior history of ankle pathology, early diagnosis, and a known etiology are some of the criteria.
Prevention
There is no surefire method of avoiding tarsal tunnel syndrome. You can reduce your chance of getting TTS if you:
- To prevent overuse injuries, take breaks in between workouts.
- Regularly stretch your ankles and feet.
- Warm up, before working out.
- Put on supportive, well-fitting shoes.
Complication
If left untreated, tarsal tunnel syndrome can result in the following:
- Foot deformity (mild to severe)
- Loss of movement in the toes (either partial or complete)
- Repeated or unnoticed injury to the leg
- Partial or complete loss of sensation in the toes or foot
Prognosis
When the underlying cause of TTS is treated, symptoms may occasionally disappear. For instance, symptoms of a lipoma or bone spur may go away with treatment. People frequently manage their TTS symptoms over time. If you have a chronic illness like arthritis, your chances of TTS are reduced.
Does tarsal tunnel syndrome have any lasting effects?
TTS can cause nerve injury if left untreated. Damage to your nerves may be irreversible and permanent. You could find it difficult to walk, work out, or carry out your everyday tasks.
Fortunately, you may control your TTS symptoms with treatment. It’s critical to begin treatment as soon as symptoms appear for the best outcomes. Treatment for TTS may potentially result in its cure, depending on its underlying cause.
Conclusion
- Rare and frequently misdiagnosed is tarsal tunnel syndrome. There could be a wide range of symptoms, including hyperesthesia, sensory impairment, and tingling or burning pain (paresthesia). The plantar face of the foot and ankle is where they are felt.
- MRI, ultrasound, the Hoffman-Tinel’s test, the dorsiflexion-eversion test, the Trepan test, and the Triple Compression Stress Test are some of the techniques used to diagnose tarsal tunnel syndrome or rule out other causes.
- The first line of treatment for tarsal tunnel syndrome should be cautious. Surgery may be used if conservative therapy is ineffective.
- High-quality studies on the efficient treatment of tarsal tunnel syndrome are scarce. Based on the patient’s edema, pain, length of symptoms, and/or time since surgery, the physical therapist should stage them. To address a patient’s unique strength, flexibility, gait, and functional limitations, management should be focused on their impairment.
FAQs
What kind of pain does tarsal tunnel syndrome cause?
Paresthesia (tingling or pins and needles), hyperesthesia (increased sensitivity), and pain that radiates from the posterior medial malleolar region to the sole, heel, and toes are the main clinical characteristics of TTS.
What is a tarsal tunnel treatment that is natural?
Tarsal tunnel syndrome can be alleviated by stretching the plantar fascia, Achilles tendon, and calf muscles. Stretching the tendons and muscles surrounding the tarsal tunnel is best done slowly and softly. A slight stretch should occur, but no pain. Repeat three times, holding each stretch for 30 seconds.
Is Tarsal Tunnel going to disappear?
If the etiology of tarsal tunnel syndrome is identified and effectively treated, a full recovery is achievable. A partial or total loss of movement or feeling may occur in certain individuals. unbearable and chronic nerve pain is possible.
How can someone who has tarsal tunnel syndrome sleep?
Your doctor might also suggest physical therapy or the use of an ankle brace or wrap to limit foot mobility and relieve pressure on the tibial nerve, which will also help you sleep better at night.
Is the Tarsal Tunnel more difficult at night?
At night, symptoms could be more severe. Long periods of standing or walking tend to worsen the pain, which typically gets worse during the day and is typically alleviated by rest, elevation, or massage. Sometimes the pain travels up into the calf and along the sole.
What is the Tarsal Tunnel’s success rate?
The range of surgical success rates is 44% to 96%. The flexor retinaculum is surgically released from its proximal attachment close to the medial malleolus and extended down to the sustentaculum tali. It is possible to release the tarsal tunnel under ultrasound guidance.
Stage 1 neuropathy: what is it?
Periods of pain or numbness in your hands or feet are possible. Keep in mind that at this point, managing these symptoms is simple. At this point, neuropathy usually results from consuming too much sugar. If any of these symptoms appear, make a quick dietary change.
What is the most effective tarsal tunnel syndrome home remedy?
Changing to low-impact activities or reducing your physical activity are two options your doctor can suggest. For 10 to 20 minutes, apply ice to your foot to help with pain and swelling. Elevating and resting your foot to lessen swelling and aid in the healing process.
How may numbness in the feet be eliminated?
Start with natural treatments for foot numbness, such as rest, foot elevation, warm or cold compresses, and mild exercise. If numbness continues or gets worse, see a doctor. They can assist in determining the underlying problem and suggest the best course of action.
Is recovery possible after tarsal tunnel syndrome?
If the etiology of tarsal tunnel syndrome is identified and effectively treated, a full recovery is achievable. A partial or total loss of movement or feeling may occur in certain individuals. Nerve pain can be unbearable and persistent.
Reference
- Tarsal Tunnel Syndrome. (2025, January 6). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22200-tarsal-tunnel-syndrome
- Oh, S. J., Sarala, P. K., Kuba, T., & Elmore, R. S. (1979). Tarsal tunnel syndrome: Electrophysiological study. Annals of Neurology, 5(4), 327–330. https://doi.org/10.1002/ana.410050404
- Tarsal Tunnel Syndrome symptoms & Treatment | Aurora Health Care. (n.d.). https://www.aurorahealthcare.org/services/orthopedics/conditions/tarsal-tunnel-syndrome
- Tarsal tunnel syndrome – UF Health. (n.d.). https://ufhealth.org/conditions-and-treatments/tarsal-tunnel-syndrome
- Nunez, K. (2023, April 3). Achilles tendon stretches and strength exercises. Healthline. https://www.healthline.com/health/achilles-tendon-stretch#takeaway