Reactive Arthritis
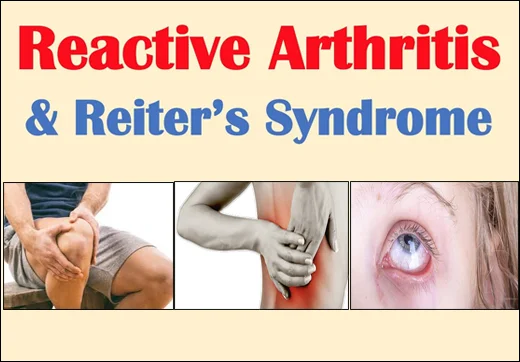
Reactive Arthritis (Reiter’s syndrome): What is it?
Reactive Arthritis is an inflammatory joint condition that develops in response to an infection, usually in the urinary tract, intestines, or genitals. It commonly affects the knees, ankles, and feet, causing pain, swelling, and stiffness.
Other symptoms may include eye inflammation (conjunctivitis), urinary problems, and skin issues. The condition is often triggered by bacterial infections such as Chlamydia, Salmonella, or Shigella. While symptoms typically resolve within a few months, treatment focuses on managing pain and inflammation with NSAIDs, physical therapy, and, in some cases, antibiotics if an underlying infection is present.
Reactive arthritis occurs when your immune system reacts abnormally to an infection in your esophagus, digestive tract, genitalia, or urinary tract. To combat infections, your immune system typically produces inflammation. However, with Reiter’s syndrome, your immune system causes inflammation in areas of your body that were never infected. It doesn’t seem to believe that the fight is done.
What causes Reactive Arthritis?
A bacterial infection is the initial cause of reactive arthritis. Typically, it is a:
- Urinary tract infection (UTI).
- Sexually transmitted infection (STI).
- Gastrointestinal infection (such as food poisoning).
- Throat infection (sore throat).
Among the particular microorganisms that might cause it are:
- Chlamydia.
- Gonorrhea.
- Salmonella.
- Shigella.
- Campylobacter.
- Yersinia.
- Mycoplasma.
- C. difficile.
- Streptococcus.
Only a small number of people get Reiter’s syndrome, which usually appears days to weeks after the initial infection is over. An autoimmune reaction seems to be triggered by the infection. This indicates that your immune system overreacts and starts to cause inflammation in healthy areas of your body. Thankfully, reactive arthritis is typically a transient symptom, in contrast to the majority of autoimmune diseases.
Spondyloarthritis is a group of inflammatory arthritis disorders that includes reactive arthritis. These are mostly autoimmune disorders. Why some people develop autoimmune disorders while others do not is a mystery to scientists. Reactive arthritis can develop without a serious infection. A gene known as HLA-B27 is one potential contributing factor. Many persons with Reiter’s syndrome also have spondyloarthritis.
Signs and symptoms of Reactive Arthritis:
Reactive arthritis symptoms often appear one to four weeks following exposure to a triggering illness. They could consist of:
- Stiffness and pain. The knees, ankles, and feet are where reactive arthritis-related joint discomfort most frequently manifests. In addition, there may be pain in the buttocks, low back, or heels.
- Eye inflammation. Conjunctivitis, or inflammation of the eyes, is common in persons with reactive arthritis.
- Urinary problems. Urination may become more frequent and uncomfortable, and there may be cervical or prostate gland inflammation.
- Inflammation (enthesitis) of the ligaments and tendons where they connect to the bone. The soles of the feet and heels are where this occurs most frequently.
- Swollen toes or fingers. In certain instances, fingers or toes may swell to the point of resembling sausages.
- Skin problems. Mouth sores and a rash on the palms of the hands and soles of the feet are just two ways that reactive arthritis can impact the skin.
- Low back pain. Usually, the discomfort is greatest in the morning or at night.
Who is susceptible to Reactive Arthritis?
Reactive arthritis can strike anyone, but it’s more likely to strike you if:
- You’re a man under 40 years old.
- You are HIV positive.
- Another autoimmune condition affects you.
- The HLA-B27 gene is present in you.
How is Reactive Arthritis diagnosed?
Your doctor will want to see them and hear about any new arthritic symptoms you may have developed. Reactive arthritis will be suggested by specific symptom combinations. If you have just recovered from an infection that may have caused Reiter’s syndrome, they will especially want to know.
Several tests may be performed to aid in the diagnosis, such as:
- X-rays.
- Computed tomography (CT) scan.
- Magnetic resonance imaging (MRI).
- Joint aspiration (arthrocentesis).
- Throat culture.
- Urinalysis.
- Blood tests.
Blood examinations:
Your physician may suggest that a blood sample be examined for:
- Evidence of an infection, either current or past
- Inflammatory symptoms
- Antibodies linked to different forms of arthritis
- Reactive arthritis and a genetic marker
Tests for joint fluid:
Your physician may take a fluid sample from inside an affected joint using a needle. We’ll test this fluid for:
- Count of white blood cells. An infection or inflammation may be indicated by an increase in white blood cells.
- Infections. The presence of bacteria in your joint fluid may be a sign of septic arthritis, which can cause serious damage to your joints.
- Crystals. Crystals of uric acid in your joint fluid could be a sign of gout. The big toe is frequently affected by this excruciating kind of arthritis.
Treatment of Reactive Arthritis:
The goal of treatment is to manage any residual sickness and regulate your symptoms.
Drugs
If there is evidence of a chronic infection, your doctor may prescribe an antibiotic if a bacterial infection causes your reactive arthritis. The bacteria present determines the antibiotic you should take.
Reactive arthritis symptoms and Signs can be reduced by:
- NSAIDs, or nonsteroidal anti-inflammatory medications. Reactive arthritis pain and inflammation can be reduced using prescription nonsteroidal anti-inflammatory medications (NSAIDs), such as indomethacin (Indocin).
- Steroids. A steroid injection into the affected joints will lessen inflammation, allowing you to resume your regular activity level. Steroid creams can be used for skin rashes, and steroid eye drops can be used for eye complaints.
- Medications for rheumatoid arthritis. There is little proof that drugs like methotrexate (Trexall), etanercept (Enbrel), or sulfasalazine (Azulfidine) can help some patients with reactive arthritis with their pain and stiffness.
Physical Therapy
You can get specific joint and muscle workouts from a physical therapist. By strengthening the muscles surrounding the affected joints, strengthening activities improve joint support. Exercises involving range of motion might help your joints become more flexible and less stiff.
Risk factors of Reactive Arthritis:
Reactive arthritis is more likely to occur if you have certain factors:
- Age. The majority of people with reactive arthritis are between the ages of 20 and 40.
- Sex. Reactive arthritis in reaction to foodborne illnesses is equally common in men and women. However, reactive arthritis caused by sexually transmitted germs is more common in men than in women.
- Hereditary factors. Reactive arthritis has been associated with a particular genetic signature. However, the syndrome never manifests in the majority of those with this marker.
Prevention of Reactive Arthritis:
The likelihood of developing reactive arthritis seems to be influenced by genetic factors. You can lessen your exposure to the microorganisms that can cause reactive arthritis, even though you cannot alter your genetic composition.
Cook your food correctly and store it at the right temperatures. By taking these precautions, you can steer clear of several foodborne bacteria, such as salmonella, shigella, yersinia, and campylobacter, that can cause reactive arthritis. Reactive arthritis can be triggered by certain sexually transmitted diseases. To reduce your risk, use condoms.
Is it possible to cure Reactive Arthritis?
Reiter’s syndrome often resolves on its own in three to twelve months, as it is self-limited. Meanwhile, therapy frequently suppresses symptoms and may hasten their resolution. However, no autoimmune disease is truly treatable, and reactive arthritis is one of them. This implies that symptoms could always recur, for instance, if you contract another illness.
Reiter’s syndrome appears to precipitate a more severe and chronic form of spondyloarthritis in a small proportion of individuals. They experience chronic joint inflammation, which over time might cause serious harm. It is uncertain if you have a distinct condition or if this is chronic reactive arthritis. Many people have many autoimmune diseases, and one might provoke another.
How should I care for myself if I have Reactive Arthritis?
While reactive arthritis is likely to be short-term, it might significantly affect your daily life during its duration. While many people experience intermittent, minor symptoms, others suffer from extreme exhaustion and discomfort. Your everyday routine or method of working may need to change during this period.
Your physician may suggest:
- Physical therapy. The muscles and tendons that support your aching joints can be gently exercised in methods that a physical therapist might recommend. Your joints may become less strained and stiff as a result.
- Orthotics. You can change how you utilize your joints or get advice from an occupational therapist on how to support them. Wearing a brace, splint, or shoe insert may help you.
- Hot/cold therapy. Soreness can be relieved in different ways by ice packs and heat packs. For instance, your healthcare practitioner may advise applying heat to your tense muscles and ice to your aching joints.
- Take power naps. While prolonged bed rest won’t assist your stiff muscles or hurting joints, chronic exhaustion might wear you down. Try taking quick sleep and getting up and moving about in between instead.
Advice on how to lower your risk of infection:
- If you know someone has an infection, try to keep your distance from them.
- Keep a tiny bottle of antibacterial hand gel on hand and wash your hands frequently.
- Regularly cleaning your teeth will help you maintain a clean mouth.
- If you are a smoker, quit.
- Ensure that your food is prepared and kept correctly.
- Make an effort to keep your home tidy and sanitary, paying particular attention to the restrooms, kitchen, and toilets.
FAQs
Does blood testing reveal reactive arthritis?
HLA-B27, a hereditary risk factor for reactive arthritis, is detected by this blood test. Although having this marker is suggestive of reactive arthritis, it is not conclusive; not all individuals who test positive have reactive arthritis, and those who test negative can nevertheless have the disorder.
Which three conditions make up reactive arthritis?
The classic trifecta of conjunctivitis, urethritis, and arthritis that follows an infection—especially one in the gastrointestinal or urogenital tracts—is called Reiter’s syndrome, or reactive arthritis.
Is there a speedy recovery from reactive arthritis?
Reactive arthritis is a condition in which an infection causes your joints to swell and hurt. Although it can last longer, it usually disappears around six months.
Which medication works best for reactive arthritis?
Reactive arthritis pain and inflammation can be reduced using prescription nonsteroidal anti-inflammatory medications (NSAIDs), such as indomethacin (Indocin). Steroids. You can resume your regular activity level after receiving a steroid injection into the affected joints, which will lessen inflammation.
What was reactive arthritis’s previous name?
In young males, reactive arthritis, often known as Reiter’s syndrome, is the most prevalent form of inflammatory polyarthritis. It can occasionally be the initial sign of an infection with the human immunodeficiency virus. More than two-thirds of reactive arthritis patients have an HLA-B27 genotype as a risk factor.
What is the impact of nutrition on arthritis?
Omega-3 fats, which are present in oily seafood like salmon and sardines, may help persons with inflammatory diseases like rheumatoid arthritis. Drinking lots of water and avoiding foods strong in purines, such as beer, seafood, and offal, may help persons with gout, a form of arthritis.
References
- Reactive arthritis – Symptoms & causes – Mayo Clinic. (2022, January 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/reactive-arthritis/symptoms-causes/syc-20354838
- Reactive Arthritis (Reiter’s Syndrome). (2025, February 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/reactive-arthritis-reiters-syndrome
- Reactive arthritis. (n.d.). Versus Arthritis. https://versusarthritis.org/about-arthritis/conditions/reactive-arthritis/