Pulmonary Hypertension
Introduction
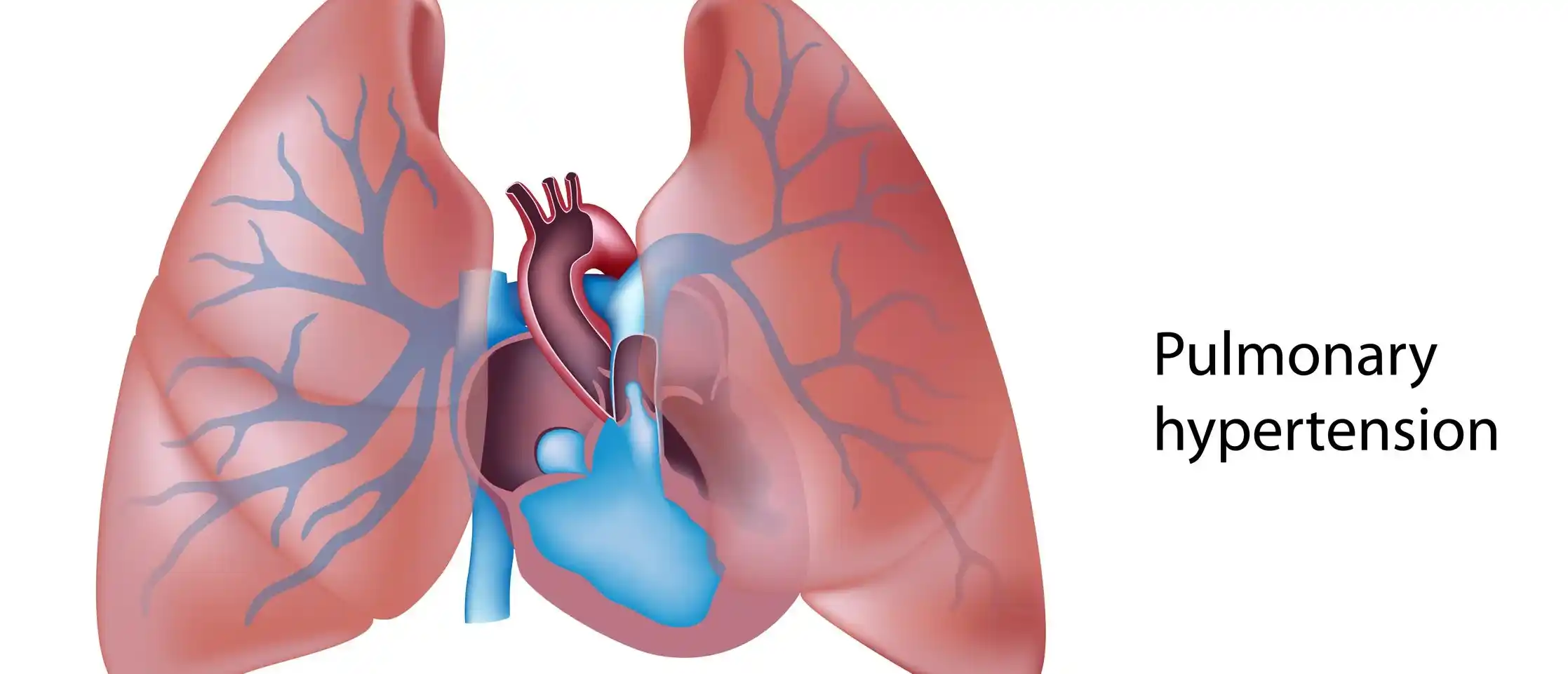
Pulmonary hypertension (PH) is a condition characterized by high blood pressure in the arteries of the lungs, leading to increased strain on the heart. It can be caused by various factors, including heart disease, lung disease, chronic blood clots, or genetic mutations.
There are two upper chambers and two lower chambers in a normal heart. The lower right chamber of the heart pumps blood to the lungs each time blood passes through it. The pulmonary artery is a large blood vessel that the blood travels through.
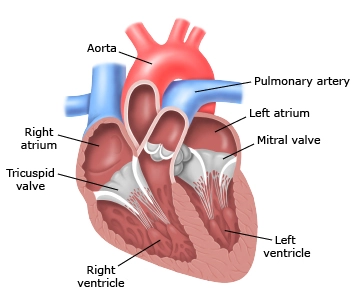
Normally, blood travels to the left side of the heart with ease via blood arteries in the lungs. The pulmonary arteries, capillaries, and veins are examples of these blood vessels.
However, alterations in the cells lining the arteries in the lungs might result in thick, bloated, thin, and rigid arterial walls. Pulmonary hypertension can result from these alterations, which slow or stop blood flow through the lungs.
Pulmonary Hypertension: What is it?
High blood pressure in the pulmonary arteries, which transport blood with low oxygen content from your heart to your lungs, is known as pulmonary hypertension. Breathlessness during daily activities is the first sign. Heart disease, lung disease, and hypoxia are the most frequent causes. A higher quality of life can be yours with early diagnosis and treatment.
A typical diagnosis of pulmonary hypertension (PH) indicates that your pulmonary arteries are experiencing elevated blood pressure. These blood arteries transport blood with low oxygen content from your heart to your lungs.
There are numerous causes of pulmonary hypertension. Usually, it is a side effect of lung or cardiac problems. However, your risk for PH might be increased by a number of other illnesses and environmental factors.
Because it restricts the flow of blood via the heart and lungs, pulmonary hypertension is harmful.
The pulmonary arteries narrow as a result of elevated blood pressure. Your heart has to work harder to pump blood that is low in oxygen to your lungs as a result.
PH harms your heart over time and leads to issues all over your body. If left untreated, it can be dangerous.
What are the effects of pulmonary hypertension on my body?
Serious health issues caused by pulmonary hypertension include:
- Anemia.
- Arrhythmias.
- Blood clots in pulmonary arteries.
- Pericardial effusion.
- Pregnant women should avoid PH. Both the mother and the fetus may experience difficulties as a result.
Pulmonary hypertension can overwork your heart and ultimately cause death if left untreated. Your heart must work harder to pump blood with low oxygen content to your lungs when your pulmonary arteries are under high blood pressure.
This blood must be pumped to your lungs by your right ventricle, also known as the lower right chamber. Because of the additional effort, PH eventually causes your right ventricle to enlarge.
Right-sided heart failure may result from this disorder, which is known as right ventricular hypertrophy.
The effects of right-sided heart failure are felt throughout the body. Numerous organs and systems may have disruptions in their regular functions.
Early diagnosis and treatment are crucial since pulmonary hypertension can impact every part of your body. The cause of your PH will determine the course of treatment your doctor recommends. Untreated PH can be fatal, regardless of the etiology.
Pathogenesis
The constriction of blood arteries that are attached to and inside the lungs is a pathophysiological feature of pulmonary arterial hypertension (WHO Group I). Since it is considerably more difficult to force water through a narrow pipe than a wide one, this makes it more difficult for the heart to pump blood through the lungs.
Fibrosis is the process by which those with damaged blood vessels thicken and stiffen over time. Vasoconstriction, thrombosis, vascular remodeling, excessive cellular proliferation, fibrosis, and decreased apoptosis/programmed cell death in the vessel walls are the mechanisms underlying this narrowing process.
These processes are caused by inflammation, abnormal metabolism, and dysregulation of specific growth factors.
This worsens the lungs’ blood flow and raises blood pressure even further. These alterations cause the right side of the heart to work harder, as is the case with other forms of pulmonary hypertension.
With systolic ventricular pressures that are lower than those the left ventricle typically experiences, the right ventricle is typically a component of a low-pressure system. Because of this, the right ventricle is unable to handle increased pressures as well.
While right ventricular adaptations, such as hypertrophy and increased heart muscle contractility, initially help in maintaining stroke volume, they eventually prove insufficient; as a result, the right ventricular muscle is unable to receive enough oxygen to meet its demands, which leads to right heart failure.
The left side of the heart receives less blood when the amount of blood passing via the lungs declines. Additionally, this blood may contain less oxygen than usual. As a result, especially during physical activity, the left side of the heart finds it increasingly difficult to pump enough oxygen to the rest of the body.
The Gaussian curvature and mean curvature of the right ventricular endocardial wall of PH patients were found to be significantly different from controls during the end-systolic volume phase of the cardiac cycle.
Although the exact molecular cause of pulmonary arterial hypertension (PAH) is unknown, it is thought that endothelial dysfunction leads to a reduction in the production of endothelium-derived vasodilators like prostacyclin and nitric oxide.
Additionally, the production of vasoconstrictors such thromboxane and vascular endothelial growth factor (VEGF) is stimulated. Patients with PAH are characterized by adventitial hypertrophy, vascular smooth muscle, and significant vasoconstriction as a consequence.
Pathway of nitric oxide-soluble guanylate cyclase
Under normal circumstances, L-arginine and oxygen are converted into nitric oxide by the vascular endothelial nitric oxide synthase.
Diffusing into nearby cells, such as platelets and vascular smooth muscle cells, this nitric oxide raises the activity of the soluble guanylate cyclase enzyme, which in turn promotes the production of guanosine triphosphate (GTP) to cyclic guanosine monophosphate (cGMP).
PKG (protein kinase G) or cGMP-dependent kinase are subsequently activated by cGMP. Activated PKG suppresses platelet activation, changes the expression of genes involved in smooth muscle cell contraction, migration, and differentiation, and promotes vasorelaxation (by lowering intracellular calcium levels).
Additionally, nitric oxide-soluble guanylate cyclase signaling has anti-inflammatory properties.
Endothelin
Endothelial cells produce the peptide endothelin-1, which is made up of 21 amino acids. It causes vasoconstriction, hypertrophy, proliferation, inflammation, and fibrosis by acting on the endothelin receptors ETA and ETB in a variety of cell types, including fibroblasts and vascular smooth muscle cells.
Additionally, it acts on endothelial cells’ ETB receptors, which causes those cells to release vasoconstrictors and vasodilators and removes endothelin-1 from the body.
Thromboxane and prostacyclin
In endothelial cells, prostacyclin is produced from arachidonic acid. Prostacyclin primarily interacts with the prostaglandin I receptor in vascular smooth muscle cells.
This causes adenylate cyclase activity to rise, which in turn causes cyclic adenosine monophosphate (cAMP) synthesis to rise. Increased cAMP-dependent protein kinase or PKA (protein kinase A) activity follows, which eventually encourages vasodilation and suppresses cell division.
Additionally, prostacyclin signaling has anti-inflammatory, anti-fibrotic, and antithrombotic properties. Phosphodiesterases 3 and 4 lower levels of cAMP, which mediates the majority of prostacyclin’s biological actions.
Arachidonic acid is also used to make the vasoconstrictor thromboxane. The production of thromboxane takes priority over the synthesis of prostacyclin in PAH.
Types and Causes of pulmonary hypertension
According to its cause, pulmonary hypertension is classified into five classes by the World Health Organization (WHO).
- Group 1 due to Pulmonary Arterial Hypertension
- Group 2 due to left sided heart diseases
- Group 3 due to Hypoxia or lung diseases
- Group 4 due to lung obstructions
- Group 5 due to other conditions
Group 1 PH due to Pulmonary Arterial Hypertension: There are numerous causes of PAH, from underlying illnesses to specific medications. Your pulmonary arteries become stiff, thick, or narrowed as a result of PAH. Your pulmonary arteries’ pressure rises as less blood can pass through.
Cause include:
- Idiopathic pulmonary arterial hypertension is a condition with unknown cause.
- Heritable pulmonary arterial hypertension is a condition caused by alterations in a gene that runs in families.
- Use of illegal drugs, such as methamphetamine, or certain medications.
- Congenital heart defects are cardiac issues that manifest from birth.
- Additional medical disorders include lupus, cirrhosis, scleroderma, and chronic liver disease.
Group 2 PH due to left sided heart diseases: Your heart’s left side circulates blood throughout your body. Your entire pulmonary circuit and the right side of your heart are impacted if there is an issue with this side of your heart. Your heart backs up with blood, which causes your pulmonary arteries to become more pressurized.
Cause include:
- left heart failure.
- Aortic or mitral valve disease are examples of left-sided cardiac valve disorders.
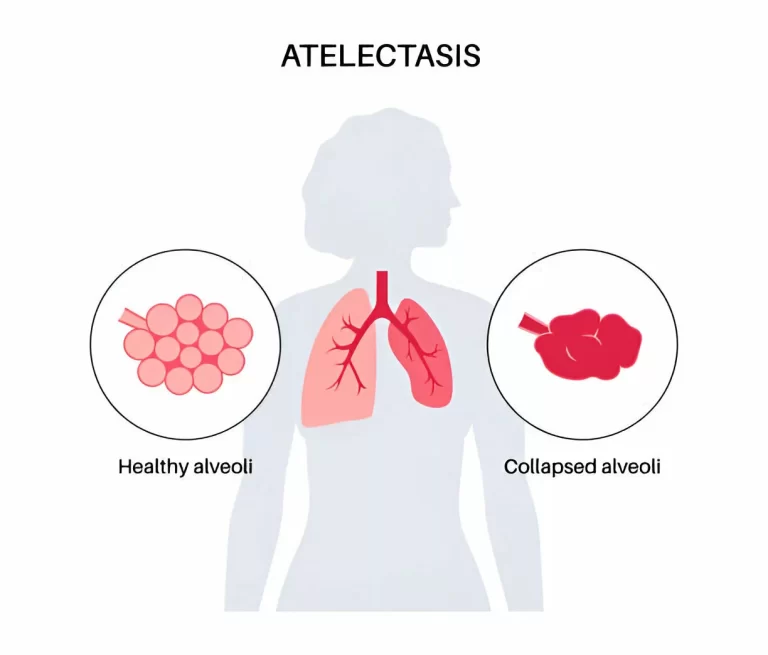
Group 3 PH as a result of hypoxia or lung diseases: Your lungs’ arteries constrict when you have certain lung conditions. Your pulmonary arteries’ pressure will rise as less blood can pass through your lungs.
Cause include:
- Pulmonary fibrosis, or lung scarring.
- Chronic obstructive pulmonary disease.
- Sleep apnea.
- Prolonged exposure to high elevation in those who might be more susceptible to pulmonary hypertension.
Group 4 PH as a result of lung obstructions: Your blood cannot pass through your lungs normally if you have a blood clot or scar from one. This increases pulmonary blood pressure and strains the right side of the heart more.
Cause include:
- Pulmonary emboli are long-term blood clots in the lungs.
- Tumors that block the pulmonary artery
Group 5 PH because of additional conditions: Blood problems and metabolic abnormalities are among the illnesses that coexist with PH. There is sometimes uncertainty regarding the exact processes by which the disease causes PH.
Cause include:
- Blood disorders, including polycythemia and essential thrombocythemia.
- Inflammatory disorders such as sarcoidosis.
- Metabolic disorders, including glycogen storage disease.
- Kidney disease.
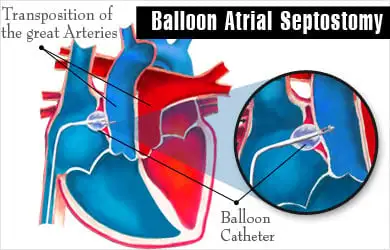
One form of congenital cardiac disease that results in pulmonary hypertension is Eisenmenger syndrome. Unresolved gaps between the heart’s chambers may cause it. Ventricular septal defects, which are big holes in the heart between the two lower heart chambers, are one example.
Blood flows in the heart incorrectly as a result of the hole. Blood with and without oxygen combines. After that, the blood goes back to the lungs rather than the rest of the body. Pulmonary hypertension results from this increase in blood flow and pulmonary artery pressure.
Pulmonary hypertension: Who is affected?
Any age of adult might be affected by pulmonary hypertension. It frequently affects those with lung or cardiac disorders. Additionally, those who have other medical disorders are more likely to have it. PH influences:
- Almost all patients have significant mitral valve disease.
- Aortic valve disease affects roughly 65% of persons.
- up to 30% of scleroderma patients.
- 20% to 40% of sickle cell disease patients.
- HIV affects about 1 in 200 persons.
Adults are typically affected by PH. Rarely, though, it may have an impact on babies. Persistent Pulmonary Hypertension of the newborn (PPHN) , is the term for this condition. Treatment in the critical care unit may be necessary for infants with this illness.
What is the prevalence of pulmonary hypertension?
Pulmonary arterial hypertension (PAH) and PH caused by blood clots are two uncommon forms of PH. However, other forms, particularly PH caused by heart or lung issues, are far more prevalent.
The precise number of people with PH worldwide is unknown. However, according to some estimates, 1 in 100 persons may have PH. This indicates that between 50 million and 70 million people have PH.
The prevalence of PH in older persons is significantly higher. Approximately 10% of persons over 65 worldwide suffer from PH.
Signs and symptoms
Pulmonary hypertension symptoms appear gradually. For months or even years, you might not see them. As the illness worsens, the symptoms worsen.
Symptoms of pulmonary hypertension include:
- Breathlessness, initially during physical activity and thereafter during rest
- Low oxygen levels can cause the skin to turn blue or gray. These changes may be more or less noticeable depending on the color of your skin
- Chest pain
- Lightheadedness or episodes of fainting
- A hammering heartbeat or rapid pulse
- Exhaustion
- Swelling in the legs, ankles, and abdomen.
Risk factors
People between the ages of 30 and 60 are typically diagnosed with pulmonary hypertension. The risk of Group 1 pulmonary hypertension, also known as pulmonary arterial hypertension (PAH), might rise with age. Younger persons are more likely to have PAH from an unidentified etiology.
The following additional factors may increase the risk of pulmonary hypertension:
- A history of the illness in the family.
- Being overweight.
- Smoking.
- Blood-clotting conditions or a family history of lung blood clots.
- Asbestos exposure.
- A congenital heart defect is a heart condition that you are born with.
- Residing at a high elevation.
- Use of specific substances, such as illegal narcotics like cocaine or methamphetamine, and some weight-loss medications.
Complications
The following are possible side effects of pulmonary hypertension:
- Heart failure and hypertrophy of the right side: This disorder, also known as cor pulmonale, results in an enlargement of the right lower chamber of the heart. In order to pump blood through constricted or blocked lung arteries, the chamber must work harder than usual.The heart walls thicken as a result. To expand its capacity to hold more blood, the lower right chamber of the heart contracts. The right lower heart chamber eventually fails as a result of these alterations, which put additional strain on the heart.
- Thrombi: Blood clots in the lungs’ tiny arteries are more likely to occur in people with pulmonary hypertension.
- Irregular pulses: Arrhythmias are potentially fatal cardiac abnormalities caused by pulmonary hypertension.
- Bleeding in the lungs: Coughing up blood and potentially fatal lung hemorrhage are two symptoms of pulmonary hypertension.
- Complications throughout pregnancy: Both the mother and the developing child may be at risk for death from pulmonary hypertension.
Stages of Pulmonary Hypertension
Pulmonary hypertension occurs in four major stages. These are referred to as “functional classes” by the World Health Organization (WHO). They relate to your ability to perform daily tasks and are based on the symptoms you experience. The symptoms of PH grow increasingly obvious and interfere with day-to-day functioning as the condition worsens.
- Class 1: You are symptom-free.
- Class 2: When you’re sleeping, you don’t experience any symptoms. However, while performing certain everyday tasks, you experience some discomfort or dyspnea. These include climbing stairs and doing housework.
- Class 3: When you’re sleeping, you might still feel good. However, because you feel exhausted or out of breath, it is now much more difficult to perform everyday tasks.
- Class 4: Even while you’re at rest, you get symptoms. Attempting to perform any routine task exacerbates the symptoms.
Testing and Diagnosis
How is the diagnosis of pulmonary hypertension made?
To diagnose pulmonary hypertension, your doctor will do a physical examination and provide tests.
You will first undergo a physical examination to look for any indications of pulmonary hypertension or other lung or heart conditions. In this examination, your healthcare provider will:
- Inquire about your health and medical background.
- Inquire about your symptoms.
- Examine the veins in your neck for size. Jugular venous distention, or bulging neck veins, may indicate right-sided heart failure.
- Feel the upper right section of your abdomen to determine the size of your liver.
- Listen to your heart and lungs with a stethoscope.
- Check for edema in your legs, ankles, and abdomen.
- Check your blood pressure.
- Use a pulse oximeter to find out how much oxygen is in your blood.
- Since many of the symptoms of pulmonary hypertension (PH) can be confused with those of other disorders, diagnosing PH can be challenging.
Your provider may use various tests for various objectives.
Your pulmonary artery blood pressure is measured by these tests:
Another name for this test is pulmonary artery catheterization, or right heart catheterization: It tests the amount of blood your heart can pump in a minute and measures the pressure inside your pulmonary arteries.
Doppler echocardiogram: A Doppler echo shows the function of your right ventricle by using sound waves. Additionally, it gauges the flow of blood via your heart valves. It enables the computation of your systolic pulmonary artery pressure by your healthcare professional.
These examinations seek to identify the underlying cause of pulmonary hypertension:
Blood tests: Examine for a variety of conditions pertaining to infections, hormone levels, and organ function. A full blood count and a complete metabolic panel are examples of specific blood tests.
A chest CT scan checks for blood clots and other lung disorders that could be contributing to or exacerbating your pulmonary hypertension.
An X-ray of your chest can reveal whether your pulmonary arteries or right ventricle are larger than they should be.
An nightly sleep test called a polysomnogram (PSG) can determine whether you have sleep apnea.
A pulmonary ventilation/perfusion (VQ) scan checks your lungs for blood clots.
A six-minute walk test may also be conducted by your provider. This test measures the amount of oxygen in your blood during exercise and the amount of activity you can tolerate. The findings show whether your pulmonary hypertension is severe or mild.
Treatment
Your underlying medical issues and the type of pulmonary hypertension you have will determine how you are treated. Your medical team will customize care to meet your specific needs.
Only two forms of PH are currently directly treatable:
- Pulmonary artery hypertension (PAH).
- Chronic thromboembolic pulmonary hypertension (CTEPH)
Pulmonary arterial hypertension (PAH) is treated with the following:
Blockers of calcium channels: These drugs can assist in lowering blood pressure throughout your body, including in your pulmonary arteries.
Diuretics: These water pills help your body to eliminate extra fluid.
Oxygen treatment: If your blood oxygen level is low, you may require this treatment.
Pulmonary dilatation agents: These drugs facilitate the relaxation and improved opening of your pulmonary arteries. This lessens the strain on your heart and increases blood flow.
CTEPH treatment consists of:
Anticoagulants: These medications help in the prevention of blood clots.
Atrial balloon septostomy (BAS): Babies with serious cardiac abnormalities are usually the ones that undergo this treatment. However, adults with PH can also utilize it. It serves as a stabilizing bridge while you await a lung transplant.
Balloon pulmonary angioplasty (BPA): Your pulmonary artery is widened with a balloon during this catheter-based surgery. It is typically performed when open surgery is not an option.
Medicine: The progression of the disease may be slowed down with the use of a soluble guanylate cyclase stimulator (SGCS).
Pulmonary endarterectomy (PEA): Blood clots in your lungs are removed during this procedure. It is the only treatment for pulmonary hypertension that is currently available, and it is solely for those who have CTEPH.
Managing the underlying disorders is the main goal of treatment for PH caused by heart or lung issues. Treatment regimens might vary greatly from person to person because PH is caused by so many distinct heart and lung problems. Discuss what’s best for you with your provider. Generally speaking, your provider might suggest:
- Dietary adjustments
- Lifestyle changes
- Medication to treat conditions like heart failure or hypertension.
- Oxygen treatment.
- Surgery, such as replacing a heart valve.
- A lung transplant is the last option for some patients with severe pulmonary hypertension.
Drugs called pulmonary vasodilators are used to treat CTEPH and PAH. Other forms of PH, such as those caused by underlying heart or lung conditions, cannot be treated with them.
Your pulmonary arteries relax with the help of pulmonary vasodilators. This lessens the strain on your heart’s right side and decreases blood pressure.
Depending on their underlying medical issues, people with PH may take several different drugs.
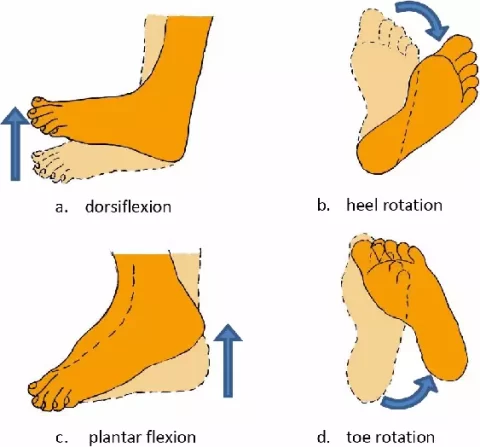
Physical therapy
Physical therapists may have used a variety of typical therapies to help in the acute patient’s recovery and discharge, such as:
- Treadmill walking
- Programs for progressive walking
- Customized exercise regimens based in chairs or beds
- Chest treatments
- Breathing Exercises
- Tips for pursed-lip breathing and dyspnea
- Pacing activities
- Evaluations of oxygen
- Providing relaxation therapy
- Promoting static cycling exercises
Education for patients, their families, and caregivers: Patients frequently experience anxiety when they exercise and are unsure of the appropriate amount of exercise.
They might have preconceived ideas about the negative consequences of exercise because they were warned against overdoing it in the past, or they might have had severe dyspnea in the past and believed that exercise could be harmful.
Referrals for pulmonary rehabilitation, an accurate strategy for many respiratory disorders, are beneficial.
Provide Activity Guidelines:
Because these actions raise the pressure in your arteries and lungs, limit your lifting, pushing, and shoving to less than 10 kg.
Walking is essential for maintaining muscle strength and enhancing circulation.
Because the lungs may not be able to meet the oxygen demands placed on the body during these activities, it is not advisable to engage in strenuous aerobic activity on a regular basis.
Pacing exercises should be used in place of activities that make you feel lightheaded or short of breath.
FAQs
Can someone with pulmonary hypertension live a long life?
At one year, the average survival rate was almost 86%. 67% after three years. 54% after five years.
Is it possible to cure pulmonary hypertension?
PAH management and treatment. Although pulmonary arterial hypertension cannot be cured, there are drugs and therapies that can help you live a better life and delay the disease’s progression.
What is the latest PAH treatment?
Every three weeks, a subcutaneous injection of Winrevair is administered. Other PAH therapies are administered in conjunction with the injection. In clinical trials, Winrevair users demonstrated a markedly enhanced capacity for exercise and a reduced rate of illness progression.
Does pulmonary hypertension improve with walking?
If you have PAH, there are some exercises that are beneficial for you. Light aerobic exercise, such as swimming or walking, is a good option. Train your hands, shoulders, and other tiny muscular groups with mild resistance.
Which examination verifies pulmonary hypertension?
It can become fatal if left untreated. However, right heart catheterization, an invasive outpatient technique that uses a tiny device put through a neck vein to detect pressures inside the heart and lungs, is presently the only approach to definitively identify pulmonary hypertension or feet
Which medication works best for lung conditions?
The best long-term control medication on the market right now is inhaled steroids. They enhance lung function and relieve lung disease symptoms. Leukotriene modifiers are long-term asthma treatments that relax the smooth muscles surrounding the airways and minimize swelling inside them.
Reference
- Pulmonary hypertension – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pulmonary-hypertension/symptoms-causes/syc-20350697
- Pulmonary hypertension (PH). (2025, February 18). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/6530-pulmonary-hypertension-ph