Proximal Tibiofibular Joint
Introduction
The proximal tibiofibular joint is a synovial joint located between the lateral condyle of the tibia and the head of the fibula. It plays a key role in stabilizing the lower leg and allowing slight movement to accommodate ankle motion.
Although it contributes minimally to knee movement, it helps distribute forces during activities like walking and running. Stability is provided by ligaments, including the anterior and posterior ligaments of the head of the fibula. Dysfunction or injury in this joint can lead to pain, instability, or altered biomechanics in the lower limb.
Biomechanics
There is comparatively little literature outlining the PTFJ’s biomechanics. Ogden characterized the main function of the joint as dissipating tensile, as opposed to compressive, weight-bearing, lateral tibial bending moments and torsional stresses exerted at the ankle. The middle portion of the fibula has a higher tensile strength than the femur, according to Evans and Bands, who also claimed that the proximal fibula was involved in tensile forces rather than compressive ones.
When the ankle joint moves, a slight gliding movement may occur at the PTFJ. The distal tibiofibular syndesmosis and the interosseous membrane allow the tibia and fibula to move relative to one another at the PTFJ. The proximal fibula is known to externally rotate at the PTFJ when the ankle is dorsiflexed.
As previously mentioned by Lambert, one of the roles of PTFJ is to tolerate torsional loads placed on the ankle joint. The fibula at the PTFJ rotates more in horizontal versions than in oblique ones, according to one of the previous investigations. When the knee flexes, the proximal fibula moves anteriorly with relative relaxation of the fibular collateral ligament and the biceps femoris, whereas when the knee extends, these structures become taut and pull the fibula posteriorly. Gliding movement was seen in the anterior-posterior axis at the PTFJ. Andersen explained how the ankle joint’s dorsiflexion causes the fibula to twist laterally.
Due to the forceful transverse expansion of the malleolar mortise during maximal dorsiflexion of the ankle, the compensatory system that is comprised of all tibiofibular joints permits a modest upward movement of the fibula. In the fluoroscopic investigation, Ogden showed ankle dorsiflexion and fibular rotation. He also discovered that the horizontal kind of PTFJ seemed to have more external rotation than the oblique type.
Similar to the rotation at the radio-humeral joint, Barnett and Napier explained the rotation of the horizontal form of PTFJ. They also discussed the connection between the PTFJ’s anatomical form and the ankle’s growing dorsiflexion ranges. According to their description, Type I (horizontal) joints have wide, freely moving articulations that are linked to an ankle’s high dorsiflexion axis inclination. Conversely, Type III (oblique) joints are small, stationary joints that have a modest dorsiflexion axis inclination.
Anatomy
The articulation between the fibula’s head and the tibia’s lateral tibial plateau is known as the proximal tibiofibular joint (PTFJ). A slanted groove behind the lateral tibial ridge located the fibular head, preventing anterior fibular movement during knee flexion. With the extension of the knee, the proximal fibula moves posteromedially. This joint’s anterolateral and posteromedial sliding motion distributes the axial load while standing, prevents the tibia from bending laterally, lowers torsional forces from the ankle, and stabilizes the knee.
The popliteus, lateral collateral ligament, anterior and posterior tibiofibular ligaments, and biceps femoris tendon (BFT) stabilize the PTFJ capsule. The lateral collateral ligament, which is taut between 0° and 30° of knee flexion, compresses the fibular head on the tibia. The IT band attaches to the tibia at Gerdy’s tubercle, where a layer of the biceps femoris tendon wraps anteriorly to the anterior PTFL. Moving the fibular head anterolaterally strengthens the joint.
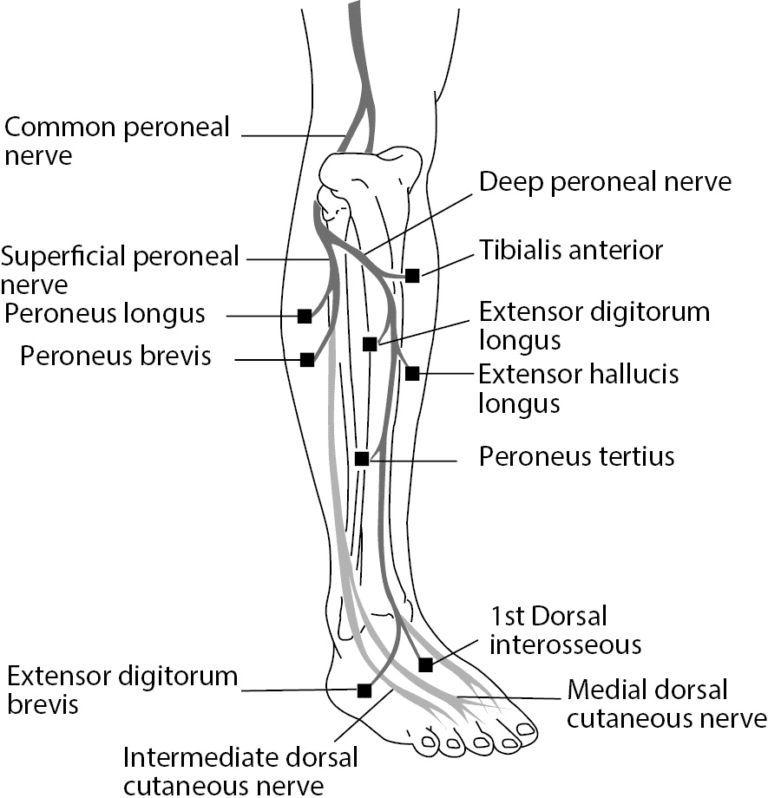
The common peroneal nerve that encircles the fibular neck is located just under the tibiofibular ligaments. To innervate the leg muscles that dorsiflex and evert the foot, this nerve splits into superficial and deep branches.
The PTFJ’s articular surface can be characterized as either oblique or horizontal. The horizontal orientation reduces the rate of injury because it has a larger surface area, a joint tilt of less than 20°, and improved rotatory motion. The oblique variety is frequently restricted, particularly when rotating, and has an inclination angle greater than 20°. The joint’s surface area can be reduced by an inclination angle of up to 76°, making it more prone to instability.
Articulating Surfaces
- The head of the fibula and the lateral condyle of the tibia articulate to produce the proximal tibiofibular joint.
- This form of synovial joint allows the bones to move by gliding over one another.
Ligaments and joint capsule
The proximal tibiofibular articulation lacks bone support since it is a planar joint. Rather, the robust fibrous capsule and two ligaments offer support.
The fibrous capsule is affixed to the articular surface edges. A synovial membrane, which occasionally runs parallel to the knee joints, lines the inside of the capsule. The popliteal bursa, a distal continuation of the knee joint cavity, connects to the tibiofibular joint in this instance via an aperture on the upper portion of its capsule.
In the anterior and posterior tibiofibular ligaments, the superior tibiofibular joint is strengthened.
- The fibular head has a short, broad, and thick anterior ligament. It passes through the joint’s front surface. The anterior aspect of the fibular head gives birth to two to three fascicles that make up the ligament. Following this, the fascicles adhere to the anterior side of the lateral tibial condyle along an oblique, superomedial path.
- The anatomy of the posterior ligament of the fibular head is likewise broad and short. A single band that originates from the posterior surface of the fibular head and travels obliquely in a superomedial direction before attaching to the posterior portion of the lateral tibial condyle makes up this structure. The tendon of the popliteus muscle crosses the posterior surface of the ligament.
Innervations
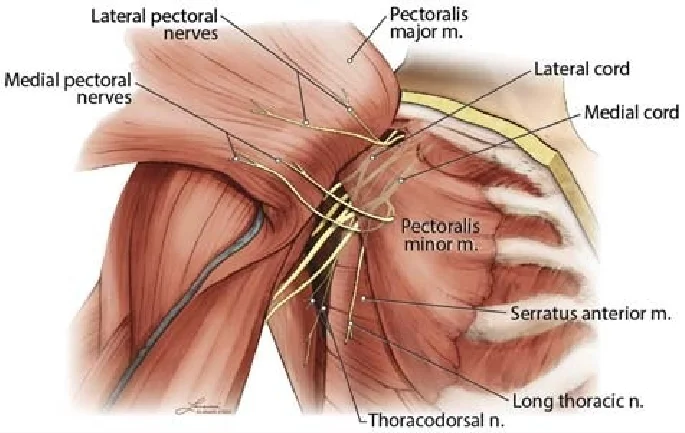
The common fibular nerve (recurrent branch) and the popliteus muscle innervate the superior tibiofibular joint.
The latter originates from the tibial nerve, whilst the former is a branch of the sciatic nerve.
Blood supply
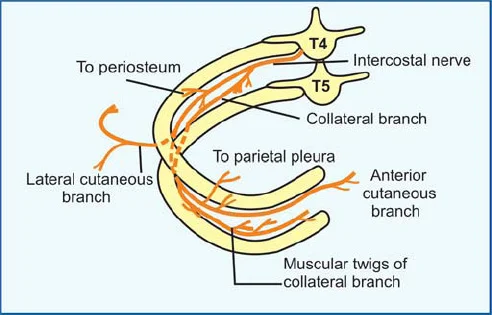
The anterior and posterior tibial recurrent arteries, two branches of the anterior tibial artery, provide blood to the superior tibiofibular joint.
Movements
The superior tibiofibular joint permits mild gliding motions since it is a plane synovial joint. More precisely, this joint permits the fibula to glide anteroposteriorly against the tibia as an auxiliary action. These motions are limited to a few degrees and take place in a superior-inferior direction. The inferior tibiofibular and ankle (talocrural) joints move them instead of any muscles actively producing them.
Clinical significances
Proximal tibiofibular joint injuries are rare and typically coexist with other lower limb injuries. The five categories of dislocations are as follows:
- Anterolateral dislocation (most common)
- Posteromedial dislocation
- Superior dislocation (rare, linked to severe ankle injuries or shortened tibia fractures)
- Rare, linked to avulsion of the foot or lengthened tibia fractures, inferior dislocation typically results in extensive soft tissue damage and a poor prognosis.
- Chronic instability (subluxation)
Anterolateral and posteromedial dislocations may go unnoticed during initial examination due to the frequent co-occurrence of fractures and ligamentous injuries (such as an ankle fracture), which could result in long-term instability.
The common peroneal nerve may sustain damage, but the prognosis is usually favorable if the dislocation is identified and appropriately treated. Since inferior dislocations typically only happen in avulsion (traumatic amputation) injuries, they are exceptional. Diseases characterized by ligamentous laxity (like Ehlers-Danlos Syndrome), muscle weakness (like muscular dystrophy), or secondary degeneration (like rheumatoid arthritis) can also cause subluxation.
FAQs
The proximal tibiofibular joint: what is it?
The tibial facet on the posterolateral aspect of the tibial condyle and the fibular facet on the medial upper surfaces of the fibula’s head make up this plane-type synovial joint.
The proximal bone is what kind?
The top part of the bone where it broadens to aid in the formation of the knee joint is called the proximal tibia. Breaks here are sometimes referred to as plateau fractures because this part of the tibia bone, which supports the joint, is sometimes called the plateau.
What joints do the proximal tibia form?
The tibial-femoral joint of the knee is formed by the proximal articulation of the tibia and femur. The talocrural joint of the ankle is formed distally by the articulation of the tibia and talus.
Why is the proximal tibiofibular joint painful?
Proximal tibiofibular joint instability is a rare and frequently overlooked cause of lateral knee pain, instability, and mechanical symptoms. Acute traumatic dislocation, chronic or recurrent dislocations, and atraumatic subluxations are the three etiologies of the condition.
How can pain in the proximal tibiofibular joint be treated?
The timing of the presentation determines how to treat proximal tibiofibular joint instability. Immobilization of the knee in extension for a few weeks to try to heal the injured posterior ligaments is reasonable if the diagnosis is made quickly after the injury (acutely).
References
- Sarma, A., Saikia, B., & Borgohain, B. (2015). A neglected articulation meets up with the proximal tibiofibular joint. 489–495 in Indian Journal of Orthopaedics, 49(5). 10.4103/0019-5413.164041 https://doi.org
- TeachMeAnatomy. (2018, October 16). Tibiofibular joints – proximal – distal – interosseous membrane – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/joints/tibiofibular-joints/
- Tibiofibular joints. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/tibiofibular-joints
- Wikipedia contributors. (2024b, May 6). Superior tibiofibular joint. Wikipedia. https://en.wikipedia.org/wiki/Superior_tibiofibular_joint