Posterior Longitudinal Ligament
Introduction
The posterior longitudinal ligament (PLL) is a strong, fibrous band that runs along the back (posterior) of the vertebral bodies inside the spinal canal. It extends from the cervical spine to the sacrum, providing support and stability to the spine while preventing excessive spinal flexion. The PLL also helps protect the spinal cord and nerves.
Whereas the fibers are thinner at the vertebral body, they are wider at the intervertebral gaps and more attached to the annulus fibrosus of the intervertebral discs. The posterior ligament shows this phenomenon more strongly than the anterior. This is important for the pathophysiology of disc herniations that occur posterolaterally because the posterior longitudinal ligament is significantly weaker than the anterior longitudinal ligament.
Structure of the Posterior Longitudinal Ligament
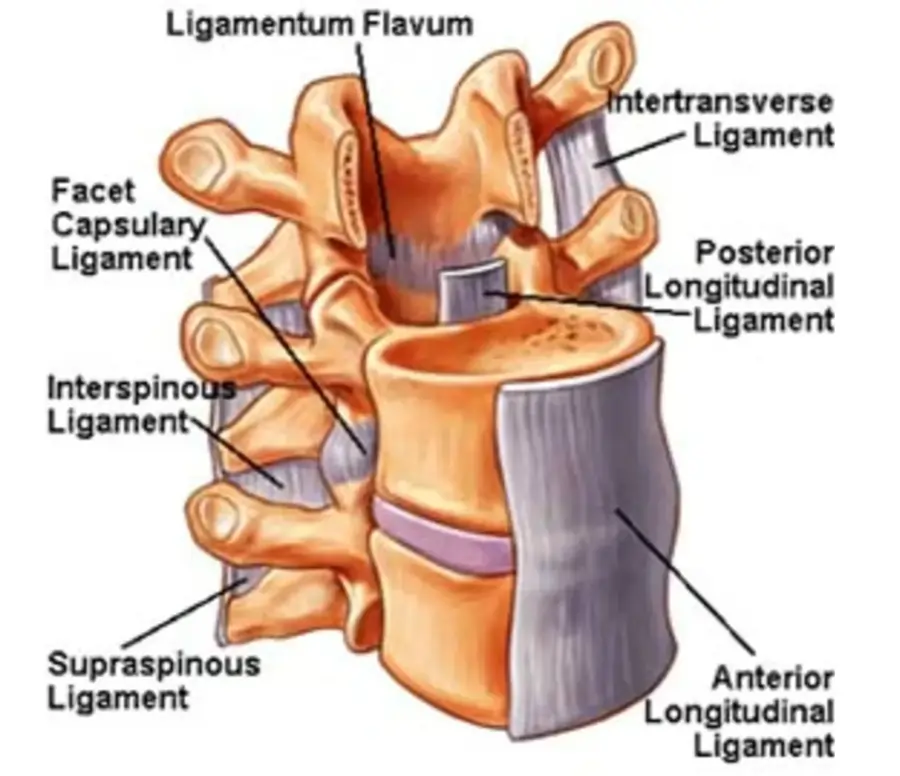
In the spinal column, the posterior longitudinal ligament (PLL) is a thick band of fibrous tissue that runs along the back or posterior aspect of the vertebral bodies. Together with the ligamentum flavum and the anterior longitudinal ligament (ALL), it is one of the main ligaments that support and stabilize the spine.
From the top of the sacrum, the triangular bone at the base of the spine, to the axis vertebra, the second cervical vertebra, the posterior longitudinal ligament stretches. It is narrower in the cervical region and wider in the lumbar region. The lower back has a thicker posterior longitudinal ligament than the neck and upper back.
The crisscrossed arrangement of collagen fibers that make up the posterior longitudinal ligament gives it strength and flexibility. Along its whole length, it is joined to the intervertebral discs and vertebral bodies.
Preventing excessive forward bending (flexion) of the spine is the primary role of the posterior longitudinal ligament. Additionally, it protects the spinal cord from harm and keeps the spine’s natural curvature.
Attachments of the Posterior Longitudinal Ligament
Along the posterior (back) side of the vertebral bodies in the spinal column runs a fibrous band known as the posterior longitudinal ligament (PLL), which is very strong and flexible. Along its whole length, it is joined to the intervertebral discs and vertebral bodies.
Each vertebral body has some tiny fibers that attach to its exterior, which is how the posterior longitudinal ligament is attached to the vertebral bodies. The ligament is attached to the bone by these fibers, which are referred to as Sharpey’s fibers.
The posterior longitudinal ligament is thicker and wider in the lumbar region than it is in the cervical region. Stretching across the intervertebral discs, the ligament is attached to the back of the vertebral bodies. The posterior longitudinal ligament is thinner and narrower in the cervical region than it is in the lumbar region. Both the intervertebral discs and the posterior surface of the vertebral bodies are where it attaches.
The posterior longitudinal ligament connects to the sacrum’s posterior surface at its top and reaches the axis vertebra (C2). The ligament attaches itself to the sacrum via a broad base. The lower portion of the spine is stabilized by this attachment.
The posterior longitudinal ligament’s attachment to the axis vertebra is unique. The ligament is attached to the posterior tubercle, a bony ridge on the back of the axis vertebra. The upper portion of the spine is stabilized by this attachment.
Generally speaking, the entire length of the posterior longitudinal ligament is connected to the intervertebral discs and vertebral bodies. The lower and upper portions of the spine are stabilized by its attachment to the sacrum and axis vertebra, respectively. The ligament is strengthened and stabilized by the attachment of Sharpey’s fibers, which also serves to fix the ligament to the bone.
Functions of the Posterior Longitudinal Ligament
The posterior longitudinal ligament (PLL) plays many important functions in the spine.
Spinal stability: By preventing excessive movement between the vertebrae, the posterior longitudinal ligament helps in spinal stability. It serves as a passive control to stop the spine from bending too much forward or backward. This is essential for avoiding injuries and maintaining the bony structure of the spine.
Spinal cord protection: The posterior longitudinal ligament contributes to spinal cord protection as well. It serves as a barrier to help keep the spinal cord from being compressed or injured, and it is situated directly behind the cord. The posterior longitudinal ligament may tear or sustain injury in spinal cord injury cases, which could result in additional spinal cord injury.
Support of the intervertebral discs: The intervertebral discs, which are situated in between each pair of vertebrae, are supported by the posterior longitudinal ligament. To keep the discs from degenerating and herniating, the ligament helps to evenly distribute pressure across them.
Preservation of appropriate spinal alignment: The proper alignment of the spine is maintained with the help of the posterior longitudinal ligament. It ensures that the spine stays in its correct position by cooperating with other muscles and ligaments. This is crucial for lowering the risk of injury and avoiding abnormal stresses on the spine.
Facilitation of spinal movement: The main purpose of the posterior longitudinal ligament is stability, however, it also allows for some spinal movement. This is essential for maintaining the flexibility and range of motion of the spine.
In conclusion, the intervertebral discs are supported, the spine is stabilized and protected, the proper alignment of the spine is maintained, and spinal movement is facilitated by the posterior longitudinal ligament. Its operations are necessary to keep the spine strong and functional.
Blood supply of the Posterior Longitudinal Ligament
The blood supply to the posterior longitudinal ligament (PLL) comes from multiple sources. The anterior spinal artery’s branch, the basivertebral artery, provides the majority of the blood supply to the posterior longitudinal ligament. The spinal cord, intervertebral discs, and vertebral bodies are all supplied with blood by the basivertebral artery, which runs along the anterior aspect of the spinal column.
The posterior spinal arteries, which run along the posterior aspect of the spinal column, provide blood to the posterior longitudinal ligament in addition to the basivertebral artery. Blood flows from these arteries to the spinal cord and the surrounding tissues.
Branches of the segmental arteries, which are tiny arteries that run along the spinal column and emerge from the aorta, also supply blood to the posterior longitudinal ligament. The muscles, ligaments, and other back structures receive blood flow from these arteries.
The posterior longitudinal ligament’s blood supply is ultimately responsible for maintaining both its bony structure and functionality. Insufficient blood flow can weaken or injure the ligament, causing the spine to become unstable or injured.
Pathology of the Posterior Longitudinal Ligament
The posterior longitudinal ligament (PLL) may become pathological for some reasons, such as inflammation, infection, trauma, or degenerative changes. Some common pathologies linked to the posterior longitudinal ligament include the following:
Osteossification of the posterior longitudinal ligament (OPLL): This condition causes the posterior longitudinal ligament to become rigid due to abnormal calcification, which results in spinal canal stenosis. Compression of the spinal cord and nerve roots may result from this condition, causing symptoms like weakness, numbness, and trouble walking. Older adults and those with a history of spinal injuries or surgeries are more likely to have posterior longitudinal ligament ossification.
Intervertebral disc herniation: The posterior longitudinal ligament supports the intervertebral discs in place between the vertebral bodies. The posterior longitudinal ligament may stretch or tear as a result of pressure from a disc herniation. Compression of the spinal cord or nerve roots, as well as spine instability, may result from this. Muscle weakness, sciatica, and back pain are some signs of a disc herniation.
Trauma: Injury to the posterior longitudinal ligament from a spinal trauma can result in instability of the spine and compression of the spinal cord or nerve roots. Trauma can be caused by falls, sports injuries, car crashes, and other accidents.
Infection: Rarely, an infection may develop in the posterior longitudinal ligament, resulting in inflammation and ligament injury. A bacterial or fungal infection that travels from another area of the body to the spine may cause this.
Inflammation: The posterior longitudinal ligament may sustain injury as a result of chronic inflammation in the spine. Rheumatoid arthritis and ankylosing spondylitis are two diseases that can inflame the spine and cause ligament erosion and weakening.
Therefore, a variety of symptoms and complications may arise from a pathology of the posterior longitudinal ligament, which can ultimately cause instability of the spine and compression of the spinal cord or nerve roots. Depending on the underlying cause and severity of the condition, treatment options may involve medication, physical therapy, surgery, or a combination of these methods.
Symptoms of the Posterior Longitudinal Ligament Injury
The spine is stabilized by the posterior longitudinal ligament (PLL), which runs along the back side of the vertebral bodies inside the spinal canal. Pain, neurological problems, and instability in the spine can result from injury to this ligament. The following are typical signs of PLL injury:
Pain
- Neck or Back Pain: The cervical, thoracic, or lumbar spines can suffer pain, depending on where the injury occurred.
- Radiating Pain: Pain may go down the arms or legs if the ligament injury affects near nerves.
Neurological Symptoms
- Tingling or numbness: in the hands, legs, feet, or arms.
- Weakness: Having problems walking (lumbar injury) or holding objects (cervical injury).
- Loss of Reflexes: In affected limbs, reflexes are either absent or slowed.
- Radiculopathy: Severe pain that travels along a nerve’s path.
Stiffness and Limited Mobility
- Reduced Range of Motion: The spine is difficult to bend or twist.
- Muscle spasms or tightness: Protective contractions of the muscles surrounding the wound.
Spinal Instability
- Feeling as though the spine is weak or “giving out.”
- Potentially worsening abnormalities like kyphosis (hunchback).
Myelopathy (If the Spinal Cord is Affected)
- Clumsiness and trouble with fine motor skills are examples of coordination issues.
- Bladder/Bowel Dysfunction: In cases of severe spinal cord compression.
Potential Reasons for Injury
- Trauma (e.g., car accidents, falls, sports injuries)
- Degeneration (e.g., aging, spondylosis)
- Herniated Discs (PLL may become stretched or torn)
- Hyperextension Injuries (e.g., whiplash)
To identify the best method of treatment and determine the level of injury, it is essential that you get a medical assessment, including imaging (MRI, CT, or X-ray), if you suspect a PLL injury.
Diagnosis
Analysis of the patient’s medical history, physical examination, and imaging tests are necessary to diagnose PLL (Posterior Longitudinal Ligament) pathology.
Medical History: The doctor will ask about any symptoms the patient may be feeling, such as stiffness, weakness, numbness, or pain in the neck or back. Additionally, they should ask about any prior accidents or diseases that could be related to the symptoms.
Physical Examination: The doctor will perform a physical examination to assess the patient’s reflexes, muscular strength, and range of motion. They may also examine for signs of inflammation or pain in the spine.
Imaging Tests: Imaging tests such as X-rays, MRIs, or CT scans are used to get a complete look at the spine and identify any abnormalities. X-rays may show changes in bone structure, but MRIs and CT scans can identify soft tissue injury or nerve compression.
Blood Tests: Blood tests may be recommended to check for signs of inflammation or infection that could be the cause of the symptoms.
Biopsy: In certain cases, a biopsy may be necessary to determine the underlying etiology of the anterior longitudinal ligament pathology. Under a microscope, a small sample of tissue is taken from the wound.
Spinal Tap: A spinal tap may be necessary to check for signs of an infection or other conditions that could be causing the symptoms.
In the end, a combination of these diagnostic methods is used to determine the root cause of the posterior longitudinal ligament disease and create a suitable treatment plan. Early diagnosis and treatment can improve a person’s quality of life and prevent further spine injuries.
Treatment of the Posterior Longitudinal Ligament Injury
Conservative treatment
Conservative management of PLL (Posterior Longitudinal Ligament) pathology involves non-surgical methods to manage symptoms and improve the patient’s quality of life. Conservative posterior longitudinal ligament therapy options include the following:
Pain management: The doctor may prescribe prescription medications or suggest over-the-counter painkillers to treat the posterior longitudinal ligament pain. Physical treatment, massage therapy, or chiropractic adjustments may also be recommended as a means of reducing pain and stiffness.
Activity and Rest Modification: The patient may need to avoid activities that worsen their symptoms and take it easy. Apart from providing braces such as a back or neck brace, the physician may suggest modifying daily routines.
Exercise and Stretching: The doctor may recommend specific exercises and stretching techniques to help build flexibility and strengthen the muscles that surround the spine.
Weight management: Maintaining a healthy weight can improve overall health and reduce spinal stress.
Anti-inflammatory Drugs: The physician may recommend corticosteroid injections or anti-inflammatory medications to reduce swelling and inflammation in the affected area.
Acupuncture: This additional therapy involves inserting tiny needles into specific body locations to lessen pain and improve healing.
Lifestyle Changes: To help control symptoms of the posterior longitudinal ligament, the doctor may suggest changing one’s lifestyle by quitting smoking, reducing the use of alcohol, and improving posture.
Depending on the extent of the injury, conservative treatment for a posterior longitudinal ligament injury usually lasts a few weeks to several months. Based on the patient’s medical history and particular needs, the doctor and patient will develop a personalized treatment plan.
Physiotherapy treatment
Compression of the spinal cord and nerve roots results from a condition known as posterior longitudinal ligament, or PLL, in which the ligament that runs along the back of the spinal column thickens and calcifies. Symptoms like pain, numbness, weakness, and trouble moving can result from this.
Exercise, education, and manual therapy are commonly used in physiotherapy treatments for the posterior longitudinal ligament. Reducing pain and enhancing function, strength, and mobility are the objectives of treatment.
Soft tissue massage, joint mobilization, and stretching are examples of manual therapy techniques that can help reduce muscle tension and increase joint mobility. These methods can also help in lowering inflammation and enhancing blood flow to the affected area.
An essential part of physiotherapy treatment for the posterior longitudinal ligament is exercise. While stretching exercises can help to increase range of motion and flexibility, strengthening exercises can help to improve muscle function and stability around the affected area. To enhance general fitness and cardiovascular health, aerobic exercise may also be advised.
A key component of physiotherapy treatment for the posterior longitudinal ligament is education. Patients will learn proper posture and body mechanics to reduce the strain on the injured area. Additionally, they might receive advice on how to carry out everyday tasks like lifting and bending without making their symptoms worse.
In addition to these methods, other modalities that can help reduce pain and inflammation include ultrasound, electrical stimulation, and heat or cold therapy.
The overall goal of physiotherapy treatment for the posterior longitudinal ligament is to help patients effectively manage their symptoms while improving the underlying causes of the condition. Many patients can see notable improvements in their mobility, function, and quality of life with a thorough treatment plan that incorporates manual therapy, exercise, education, and modalities.
Risk factors
The development of the posterior longitudinal ligament is linked to some risk factors. These consist of:
- Age: older adults, especially those over 50, are more likely to have posterior longitudinal ligaments.
- Gender: The posterior longitudinal ligament is more common in women than in men.
- Genetics: Given that the posterior longitudinal ligament tends to run in families, there may be a genetic component to its development.
- Obesity: Being overweight or obese increases the risk of developing posterior longitudinal ligament because it puts a lot of stress on the spinal column.
- Trauma: The development of a posterior longitudinal ligament may be more likely in individuals with a history of spinal trauma, such as a fall or auto accident.
- Spinal surgery: The risk of developing posterior longitudinal ligament is also increased by prior spinal surgery.
- Arthritis: Rheumatoid arthritis and osteoarthritis are two forms of arthritis that can raise the risk of posterior longitudinal ligament development.
- Diabetes: Due to potential alterations in the body’s metabolism of calcium and other minerals, people with diabetes may be more susceptible to developing posterior longitudinal ligaments.
- Smoking: The risk of developing posterior longitudinal ligament may be increased by smoking’s effects on blood flow to the spinal column.
- Bad posture: Over time, poor posture can increase the risk of developing a posterior longitudinal ligament by placing additional strain on the spinal column.
It is important to remember that developing a posterior longitudinal ligament is not always a result of having one or more of these risk factors. People who have these risk factors, however, should be conscious of their elevated risk and take precautions to avoid or treat the condition should it occur.
How to avoid posterior longitudinal ligament injuries
It can be difficult to prevent PLL (Posterior Longitudinal Ligament) injuries because some risk factors, like age and genetics, are uncontrollable.
To minimize the risk of developing a posterior longitudinal ligament or, if one has already occurred, to stop further injury, some actions can be taken. The posterior longitudinal ligament can be protected against injuries in the following ways:
- Maintain a healthy weight: Obesity and excess weight can strain the spine and raise the risk of posterior longitudinal ligament development. Thus, injuries to the posterior longitudinal ligament can be avoided by maintaining a healthy weight through a balanced diet and regular exercise.
- Maintain proper posture: Over time, poor posture can increase the risk of developing posterior longitudinal ligament by placing additional strain on the spinal column. As a result, maintaining proper posture when standing, sitting, and walking is crucial. This involves maintaining the head in line with the spine, shoulders back, and chest out.
- Engage in regular physical activity: Frequent exercise can help establish stronger bones and muscles throughout the body, including the spine. This can help prevent further injury if it has already happened or lower the risk of developing a posterior longitudinal ligament.
- Avoid smoking: Smoking can increase the risk of developing posterior longitudinal ligament by reducing blood flow to the spinal column. The posterior longitudinal ligament can therefore be protected from injury by stopping smoking or avoiding it completely.
- Wear protective gear: It’s crucial to wear the proper protective gear, such as helmets, back braces, or support belts, if you engage in activities that increase your risk of spinal injuries, such as heavy lifting or contact sports.
- Get medical help right away if you have any spinal injuries: Get help right away if you have any symptoms of a spinal injury, such as tingling in your arms or legs, numbness, or back pain. In addition to lowering the risk of developing posterior longitudinal ligament, early intervention can help stop additional spine injury.
A healthy weight, proper posture, regular exercise, avoiding smoking, wearing protective gear, and seeking immediate medical attention for any spinal injuries are all important ways to prevent injuries to the posterior longitudinal ligament.
FAQs
The posterior longitudinal ligament: what is it?
A fibrous band called the posterior longitudinal ligament runs along the back of the spine’s vertebral bodies.
What is the posterior longitudinal ligament used for?
The posterior longitudinal ligament helps in maintaining spinal stability and limiting the vertebral column’s excessive flexion, or forward bending.
What leads to an injury to the posterior longitudinal ligament?
A posterior longitudinal ligament injury may be caused by trauma to the spine, degenerative changes in the spine, or a family history of spinal disorders.
What signs of a posterior longitudinal ligament injury are present?
Back or neck pain, tingling or numbness in the arms or legs, weakness in the limbs, and trouble standing or walking are all signs of a posterior longitudinal ligament injury.
How can an injury to the posterior longitudinal ligament be identified?
Imaging tests like MRI scans or X-rays, as well as additional diagnostic tests like nerve conduction studies, can all be used to diagnose a posterior longitudinal ligament injury.
How is a posterior longitudinal ligament injury treated?
Treatment options for a posterior longitudinal ligament injury include rest, physical therapy, pain management, and, in severe cases, surgery.
Is it possible to avoid a posterior longitudinal ligament injury?
Although a posterior longitudinal ligament injury cannot always be prevented, the risk can be decreased by practicing proper posture, getting regular exercise, and avoiding activities that place undue strain on the spine.
What is the posterior longitudinal ligament’s unique characteristic?
The ligament is stronger than the anterior longitudinal ligament because it is wider at the intervertebral disc space and much shorter at the vertebral bodies. Understanding certain pathological conditions of the spine, like the usual location of a spinal disc herniation, is crucial.
References
- Patel, D. (2023g, August 22). Posterior longitudinal ligament – anatomy, structure, function. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/posterior-longitudinal-ligament/


One Comment