Posterior Cruciate Ligament (PCL)
Introduction
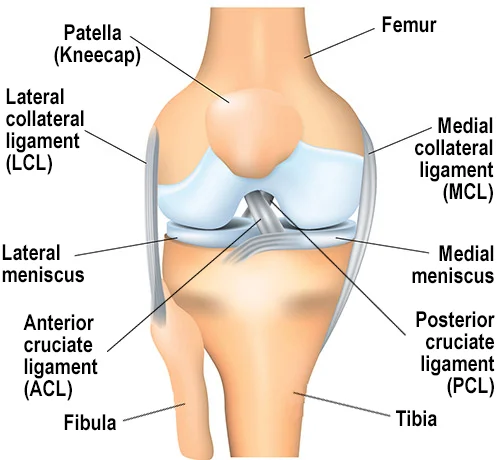
The Posterior Cruciate Ligament (PCL) is one of the four major ligaments in the knee, located at the back of the joint. It connects the femur (thigh bone) to the tibia (shin bone) and primarily functions to prevent the tibia from moving too far backward. The PCL provides stability to the knee, especially during activities involving sudden changes in direction or impact.
Posterior Cruciate Ligament (PCL) Anatomy
The posterior cruciate ligament, or PCL, is another crucial ligament in the knee joint that aids in knee stability and stops the tibia from moving backward relative to the femur. The PCL can also cause discomfort, swelling, instability, and trouble walking or bearing weight on the injured limb, just like the ACL.
ACL and PCL injuries can be diagnosed and treated similarly, depending on the location and degree of the injury. The likelihood of a PCL injury can also be decreased by taking preventative steps like using the right protective gear, maintaining perfect technique during sports or exercise, and warming up and stretching properly.
Structure of the Posterior Cruciate Ligament (PCL)
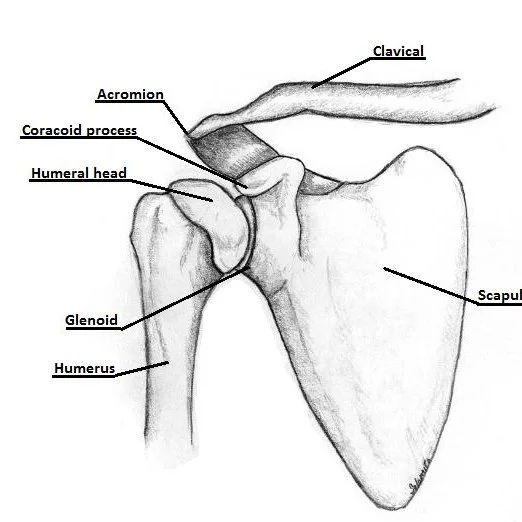
One of the most important ligaments in the knee joint is the posterior cruciate ligament (PCL). It is connected to the tibia (shin bone) and femur (thigh bone) near the rear of the knee. The PCL is the main ligament that stabilizes the knee joint and is bigger and stronger than the anterior cruciate ligament (ACL).
The posteromedial bundle (PMB) and the anterolateral bundle (ALB) are the two distinct bundles that make up the PCL. The tibia on the femur cannot posteriorly translate because of the ALB, which is stronger and tighter than the PMB. The PMB is more flexible and gives rotating forces more stability.
The medial femoral condyle, a bony protuberance on the inside of the femur, is where the PCL begins. The lateral surface of the tibia is where the ALB and the medial surface are attached, respectively. The menisci, which are cartilage formations that aid in stabilizing and cushioning the knee joint, are also attached to the PCL.
Collagen strands, the building blocks of PCL, are crisscrossed to provide it strength and stability. A proteoglycan matrix around the collagen fibers aids in shock absorption and lubricates the ligament.
Function of the Posterior Cruciate Ligament (PCL)
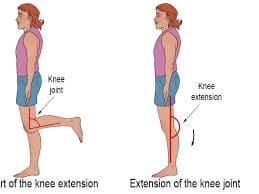
The PCL’s primary work is to keep the tibia from sliding too far backward with the femur, which could harm the knee’s joint surfaces and other internal structures. The posterior (rear) portion of the knee is supported, and it also aids in stabilizing the knee joint during rotating motions.
PCL injuries are usually caused by direct hits to the front of the knee, like in an automobile accident or when someone falls onto a bent knee, as opposed to the ACL, which is frequently hurt during abrupt stops or direction changes. PCL injuries can cause stiffness, soreness, swelling, and trouble walking or carrying weight on the injured leg.
A person’s mobility and quality of life may be greatly impacted by injuries to the PCL, which is essential for preserving the stability and functionality of the knee joint.
Blood supply of the PCL
There are multiple routes of blood flow to the posterior cruciate ligament (PCL). The middle genicular artery, a branch of the popliteal artery, provides the PCL with its primary blood supply. The popliteal artery, a large artery that delivers blood to the lower leg and foot, is situated behind the knee joint.
The inferior medial and lateral genicular arteries, which are branches of the popliteal artery, provide blood to the PCL in addition to the middle genicular artery. The PCL and other knee joint components receive extra blood flow from these arteries.
The PCL’s blood flow is necessary to keep the ligament healthy and functioning properly. Knee instability and discomfort may result from the PCL becoming weaker or injured due to inadequate blood flow.
PCL injuries can interfere with the ligament’s blood flow, which makes it even more difficult for it to heal and recover. Therefore, it is crucial to treat PCL injuries as soon as possible to restore normal function and avoid long-term consequences.
Signs and symptoms of injury to the posterior cruciate ligament (PCL)
The severity of the injury can affect the symptoms of a PCL injury. Common symptoms include the following:
- Knee Pain: One of the most typical signs of a PCL injury is pain in the rear of the knee. Activity might exacerbate the discomfort, which can range from mild to severe.
- Knee joint swelling: Another typical sign of a PCL injury is knee joint swelling. In addition to mild to severe edema, rigidity may also be present.
- Instability: A PCL injury frequently manifests as a sensation of instability or looseness in the knee joint. There may be a buckling or givingaway sensation in the knee.
- Walking difficulties: Walking can be difficult after a PCL injury, particularly if the knee joint is extremely painful or unstable.
- Restricted range of motion: It may be difficult to fully bend or straighten the knee due to a PCL injury that also limits the knee joint’s range of motion.
- Weight-bearing difficulties: It could be difficult to bear weight on the injured leg if the PCL injury is significant.
- Popping or clicking noises: In certain situations, a PCL injury may be accompanied by popping or clicking noises coming from the knee.
Activities Injuries to the ligaments are referred to as “sprains” and are graded in severity.
Grade 1 Sprains
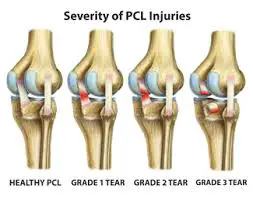
- A Grade 1 sprain causes minor injury to the ligament. Even when it has been slightly stretched, it can still support the stability of the knee joint.
Grade 2 Sprains
- The ligament is stretched to its breaking point in a Grade 2 sprain. This is frequently called a partial ligament tear.
Grade 3 Sprains
- The most common term used to describe this kind of sprain is a complete tear of the ligament. The knee joint is unstable due to a split ligament.
- Total posterior cruciate ligament rupture
A whole posterior cruciate ligament tear is seen from the rear. - Usually partial injuries, posterior cruciate ligament tears can mend themselves. Individuals who have just suffered injuries to their posterior cruciate ligaments can typically resume their athletic activities without experiencing issues with knee stability.
Injuries of the posterior cruciate ligament
There are several methods to harm the PCL, including:
Direct impact: The PCL may be torn or stretched if the tibia moves backward in response to a direct strike to the front of the bent knee.
Hyperextension: If the knee is pushed straighter than it should be, this could cause the PCL to tear or stretch.
Twisting or rotating forces: The PCL may tear if the knee experiences abrupt twisting or rotational forces, as could occur during sports.
Automobile accidents: When the knee collides with the steering wheel or dashboard, injuries to the knee may result.
Falls: The PCL may stretch or tear if you fall onto a bent knee, which can cause the tibia to slide backward.
Sports: Players who play sports like basketball, football, and soccer that require quick pauses and direction changes are more likely to get a PCL injury.
Overuse: Running and jumping put a lot of strain on the knee joint, which can weaken and potentially tear the PCL.
How to Treat Posterior Cruciate Ligament (PCL) Injury
Conservative treatment
Non-surgical techniques to control pain and encourage healing are part of conservative treatment for a PCL injury. Conservative treatment aims to enhance knee stability, lessen discomfort and inflammation, and get the knee joint back to its normal function. For PCL injuries, some typical conservative therapies include:
- Rest: The knee needs to rest to heal. Activities like jogging and jumping that make your symptoms worse might need to be avoided.
- Ice therapy: Putting ice on the injured knee can help it feel less swollen and painful. Several times a day, you can apply ice for 20 minutes at a time.
- Compression: Using a knee brace or compression bandage might assist in supporting the knee joint and reduce swelling.
- Physical therapy: A physical therapist can assist you with exercises that increase the strength, range of motion, and stability of your knees. Exercises could involve lunges, squats, and leg lifts.
- Medication: Non-steroidal anti-inflammatory medicines (NSAIDs) and acetaminophen are examples of over-the-counter pain treatments that can help lower inflammation and pain.
- Injection therapy: To lessen discomfort and inflammation, your doctor can occasionally advise injecting medicine straight into the knee joint.
Depending on how severe your injury is, conservative treatment could take weeks or months. Surgery may be required to repair or reconstruct the PCL if conservative treatment is unable to alleviate your symptoms.
Physiotherapy treatment
For PCL injuries, physiotherapy uses a mix of manual therapy, exercises, and modalities to increase knee strength, range of motion, and stability. Restoring knee joint function, promoting healing, and lowering pain and inflammation are the objectives of physical therapy.

- Manual treatment: To lessen discomfort and increase knee mobility, a physiotherapist may employ manual therapy techniques like stretching, joint manipulation, and massage.
- Exercises for range of motion: To increase flexibility and avoid stiffness, range of motion exercises involve exercising the knee joint through its entire range of motion. Leg swings, knee bends, and heel slides are a few examples of these workouts.
- Strengthening exercises: The purpose of strengthening exercises is to increase the strength of the muscles surrounding the knee joint, which will give it stability and support. Squats, lunges, and leg presses are a few examples of these workouts.
- Training for balance and proprioception: To increase knee stability, using activities that test your balance and coordination is known as balance and proprioception training. A wobble board, agility drills, and one-legged standing are a few examples of these workouts.
- Modalities: To lessen pain and inflammation and encourage healing, modalities like electrical stimulation, ultrasound, heat, and ice may be applied.
- Functional training: Functional training entails doing exercises that replicate the tasks you must complete in your everyday life or while participating in sports. You can lower your chance of re-injury and return to your regular activities with confidence with this kind of training.
For PCL injuries, the duration of physiotherapy treatment may vary depending on the severity of the injury and your specific needs. Your physiotherapist will collaborate with you to create a customized treatment plan that meets your unique requirements and goals.
Risk factors of the posterior cruciate ligament
One of the four main ligaments of the knee joint, the posterior cruciate ligament (PCL), aids in stabilizing the joint and limiting the tibia bone’s excessive backward movement. Several risk factors can result in PCL injuries, such as:
Trauma: A PCL injury may result from a direct impact on the knee, such as in a car accident or tumble. Due to the high-impact nature of contact sports like basketball and football, athletes participating in these activities are also more likely to sustain PCL injuries.
Hyperextension: PCL injuries may also result from excessive knee joint extension. This may occur during abrupt pauses and twists or after landing from a jump.
Knee dislocation: The PCL may sustain significant harm if the knee joint’s bones are pushed out of their natural position.
Muscle imbalances: The risk of PCL injuries may be raised by weakness or tension in the muscles that surround the knee joint. Overuse, bad posture, and muscular imbalances are a few possible causes.
Prior knee injuries: Due to the increased strain on the ligament, people who have previously suffered knee injuries, such as meniscus or ACL tears, may be more susceptible to PCL injuries.
Gender and age: Males are more likely than females to sustain PCL injuries, and people over 40 may be more vulnerable because of aging-related changes in the ligaments and joints.
Genetics: Due to aberrant joint anatomy or ligament laxity, certain people may be genetically prone to PCL injuries.
To lower the incidence of PCL injuries and improve general knee health, it is critical to recognize and manage these risk factors.
How to reduce the possibility of posterior cruciate ligament injury
The posterior cruciate ligament (PCL) can be strengthened in some ways:
Strengthening exercises: The PCL can be supported and protected by strengthening the muscles surrounding the knee joint. Strength training can be achieved with exercises like calf lifts, leg presses, lunges, and squats.
Stretching: Stretching can help avoid PCL injuries by increasing flexibility and reducing muscle stiffness. Make sure to stretch your hamstrings, quadriceps, and calves.
Correct technique: To prevent putting too much strain on the PCL, it’s critical to employ adequate technique when playing sports or engaging in other activities that need the knee joint. This can entail avoiding abrupt stops and twists and employing appropriate landing methods when jumping or turning.
Protective equipment: During high-impact activities, using the proper protective equipment, such as knee pads or braces, can help lower the risk of PCL injuries.
Rest and recovery: After engaging in strenuous physical activity, allowing the knee joint to rest and recuperate can assist in avoiding overuse injuries and support knee health in general.
Maintaining a healthy weight: Carrying too much weight can put more strain on the knee joint, raising the possibility of PCL injuries. This risk can be decreased by maintaining a healthy weight through exercise and food.
Seeing a doctor: It’s critical to get medical help right away if you feel any pain or discomfort in your knee joint. Injuries to the knee can be prevented and healing accelerated with early diagnosis and treatment.
FAQs
The posterior cruciate ligament (PCL): what is it?
Among the four main ligaments in the knee joint that give the knee stability and support is the PCL.
How can a PCL injury occur?
A direct hit to the front of the knee, excessive knee extension, or an abrupt change in direction while the foot is planted can all result in a PCL injury.
What features make up a PCL injury?
Pain, swelling, stiffness, trouble walking, knee instability, and a popping sound at the site of injury are all signs of a PCL injury.
How do you diagnose a PCL injury?
A physical examination, imaging tests like X-rays or MRIs, and particular testing to look for PCL injury are used to diagnose a PCL injury.
What kind of care is advised for a PCL injury?
The conditions surrounding a PCL injury determine the course of treatment. Physical therapy, elevation, compression, ice, and rest are all non-surgical therapeutic options.
What is the average recovery period following a PCL injury?
How long it takes to heal from a PCL injury depends on how severe it is and how it is treated. Severe injuries may require several months to fully recover, but mild injuries may heal in a matter of weeks.
Is it possible to avoid a PCL injury?
A PCL injury can be avoided by warming up properly before exercise or sports activities, wearing the right protective gear, performing activities with the right technique, and keeping your knees healthy overall with frequent stretching and exercise.
References
- Patel, D. (2023b, December 13). Posterior cruciate ligament (PCL) – anatomy, structure, function. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/posterior-cruciate-ligament-pcl/
- Dhameliya, N. (2023, October 21). Posterior cruciate ligament – anatomy, function, injury. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/posterior-cruciate-ligament/