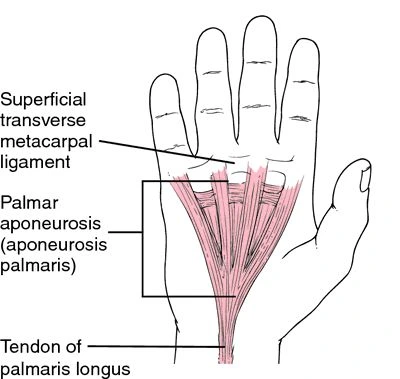
Palmar Aponeurosis
The palmar aponeurosis is a thick, triangular layer of connective tissue located in the palm of the hand. It functions to protect underlying structures, provide support to the hand, and aid in grip by connecting the palmar skin to the deeper tissues.
The aponeurosis extends from the flexor retinaculum to the bases of the fingers, contributing to the stability and strength of the hand during various movements.
Introduction
The core of the palm’s deep fascia, a highly specialized, thickened structure with limited mobility, is called the palmar aponeurosis. It is triangular and covers the tendon and neurovascular tissues underneath. It mostly encompasses the long flexor tendons, the superficial branch of the ulnar nerve, the terminal portion of the median nerve, and the superficial palmar arch. According to phylogenetic analysis, the deteriorated tendon of palmaris longus is known as palmar aponeurosis.
Beneath the palm’s skin is a fibrous tissue called palmar aponeurosis, which extends from the flexor retinaculum and splits into four slips that connect to each finger. Its involvement in disorders such as Dupuytren’s contracture, which can result in flexion deformity of the fingers, makes it clinically significant.
The inverted triangle-shaped palmar aponeurosis thins out laterally over the thenar eminence and medially over the hypothenar eminence, and fanned out over the palm.
To reach their objectives, the superficial palmar arch and the median nerve that enters the palm through the carpal tunnel must go deep into the palmar aponeurosis. On the other hand, the ulnar nerve’s palmar cutaneous branch travels above the palmar aponeurosis to the hypothenar eminence. Together with the palmar digital arteries and nerves, the tendons of the flexor digitorum superficialis and profundus travel through digital slips that are created between the palmar aponeurosis and the heads of the metacarpal bones.
While the palmaris brevis muscle originates from the palmar aponeurosis, the palmaris longus muscle tendon joins to it. According to some authors, palmar aponeurosis is even thought to be the palmaris longus deteriorated tendon.
The palmar aponeurosis enhances hand grip and shields the underlying flexor tendons, veins, and nerves because it has superficial fibers that adhere to the skin.
What is an Aponeurosis?
Your muscles and bones are connected by a thin sheath of connective tissue called an aponeurosis. Tendons and aponeuroses are comparable. They provide stability and strength to your body by supporting your muscles. When your muscles contract, aponeuroses absorb energy. Your body is covered in aponeuroses. They are crucial for posture and mobility.
Your body has a flat layer of connective tissue called an aponeurosis, which is crucial for posture and movement. Although they play a somewhat different purpose, aponeuroses (plural) are comparable to your tendons. To attach your muscles to your bones and cartilage, they serve as insertion sites for your muscle fibers.
What are the types of aponeurosis?
Your body contains a wide variety of aponeuroses. Here are a few instances:
Bicipital aponeurosis
The broad tissue layer in your biceps is called the bicipital aponeurosis. The muscles on the front of your upper arms are called biceps. The inner portion of your elbow is where your bicipital aponeurosis is situated. It fortifies this region and aids in safeguarding your upper arm’s brachial artery and median nerve.
Epicranial aponeurosis
The upper portion of your skull is covered by your epicranial aponeurosis. It resembles a thin, three-layered helmet underneath your scalp. The outermost initial layer is your skin. The second layer is composed of dense connective tissue. The third layer consists of your epicranial aponeurosis. A muscle in your skull that regulates your facial expressions is supported by the movement of all three layers.
Palmar aponeurosis
The palm of your hand contains your palmar aponeurosis. It extends from the base of your fingers to the fold of your wrist. It allows you to cup and grasp objects by adhering to the skin in the palm of your hand. It also shields your muscles and tendons. Dupuytren’s disease might develop as a result of your palmar aponeurosis becoming thicker and shorter over time.
Plantar aponeurosis
The sole of your foot contains your plantar aponeurosis, often known as the plantar fascia. It extends from the front portion of your foot to your heel bone. Your foot’s nerves and arteries are shielded by your plantar aponeurosis. It helps regulate mobility around your ankle and supports the arch of your foot. Additionally, it equally distributes force across your foot. Plantar fasciitis can result from overstretching your plantar aponeurosis.
Erector spinae aponeurosis
Your lower back contains your erector spinae aponeurosis (ESA). Your thoracolumbar fascia (TLF) meshes in with it. Another thick layer of connective tissue that envelops your back muscles is called your TLF. Your ESA and TLF work together to divide the muscles in your abdominal wall from the muscles in your spine. Breathing, posture, and load transmission all depend on them.
Aponeurosis of the external oblique
Your outer abdominal oblique muscle is where the aponeurosis of your external oblique is attached. This muscle runs down the sides of your body to your pelvis from the bottom of your ribs. Your external oblique aponeurosis facilitates the side-to-side twisting of your trunk by your oblique muscles. Additionally, it facilitates your spine’s movement.
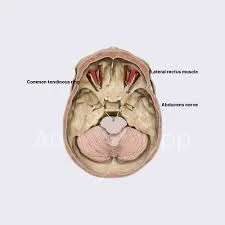
Anatomy
The palm’s central, lateral, and medial muscles are invested by the palmar aponeurosis, also known as the palmar fascia.
The middle part, which is triangular and extremely strong, takes up the middle of the palm.
Apex
- Its apex receives the palmaris longus’s enlarged tendon and is connected with the transverse carpal ligament’s lower edge.
- The apex is located proximally, blending with the flexor retinaculum and continuing with the palmaris longus tendon.
Base
- Four slips, one for each finger, split off from its base underneath. Each slip releases superficial fibers into the skin of the finger and palm, those into the fingers that flow into the skin at the transverse fold at the bases of the fingers, and those into the palm that connect the skin at the furrow that corresponds to the metacarpophalangeal articulations.
- It stretches out distally toward the bases of the fingers from the flexor retinaculum’s distal edge.
The tendons and muscles on the palmar surface of the hand are protected by the palmar aponeurosis, a robust, triangular membrane.
- The apex of the longitudinal fibers is either attached to the wrist’s flexor retinaculum or, if existent, continuous with the palmaris longus. The index, middle, ring, and little fingers are reached by the four longitudinal bundles that are created when the fibers go distally. The thumb receives a less distinct bundle. The longitudinal fibers of the palmar aponeurosis split into three layers distal to the transverse fibers.
- The initial longitudinal fibers are superficially introduced into the base of the fingers and the skin of the distal palm.
- The second, middle longitudinal fibers continue into the fingers, where they are continuous with the lateral digital sheaths, and enter deep into the superficial transverse metacarpal ligament.
- The third, deepest layer of longitudinal fibers attaches to the extensor tendon, proximal phalanx, and metacarpal bone after penetrating the deep transverse metacarpal ligament and circling the sides of the metacarpophalangeal joint.
- The deepest layer of the palmar fascia is made up of the transverse fibers of the palmar aponeurosis. They are located in a band about 2 cm wide, proximal to the distal palmar crease. The flexor tendon’s anterior fibers merge with the flexor tendon sheaths’ anterior fibers. The palmar aponeurosis is attached to the thenar and hypothenar eminences by vertical fibers.
Superficial fibers are inserted into the skin at the crease of the MCP joints.
Deep (main) fibers insert into:
- The proximal end of the flexor sheaths
- The deep transverse ligament of the palm
- The bases of the proximal phalanges
The flexor tendons travel through the narrow channels that are created on the front of the metacarpal bones as a result of this arrangement. The tendons of the lumbricals, as well as the digital vessels and nerves, are transmitted in the spaces between the four slips.
The distinct processes are joined at the points of separation into the aforementioned slips by a large number of robust, transverse fasciculi.
The palmaris brevis originates from the medial margin of the palmar aponeurosis, which is firmly attached to the integument by dense fibro areolar tissue that forms the superficial palmar fascia.
On either side, it gives off a septum that is continuous with the interosseous aponeurosis and divides the intermediate from the collateral groups of muscles. It also covers the superficial volar arch, the tendons of the flexor muscles, and the branches of the median and ulnar nerves.
Lateral and medial portions
The palmar aponeurosis’s lateral and medial portions are thin, fibrous layers that cover the thumb’s ball muscles on the radial side and the little finger’s muscles on the ulnar side. They are continuous with the central portion and the fascia on the hand’s dorsum.
Function
- Improves grip by providing a strong connection to the palm’s skin.
- Shields the nerves, vessels, and tendons underneath.
The palmar aponeurosis protects the hand’s soft tissue and lengthy flexor tendons, radiating into the fingers. To reach their objectives, the superficial palmar arch and median nerve penetrate deep into the aponeurosis, whereas the palmar cutaneous branch of the ulnar nerve travels above the palmar aponeurosis. The flexor tendons go through narrow passageways that are created between the metacarpal bone heads and the palmar aponeurosis. To reach the fingers, the palmar digital arteries and nerves travel via the four digital slips of the aponeurosis.
The palmar aponeurosis is the origin of the palmaris brevis tendon and the insertion point of the palmaris longus tendon. The webs between the fingers are supported by the transverse fibers. It strengthens the hand’s grasp and shields the tendons beneath it as it adheres to the skin.
- Your hand’s palmar aponeurosis serves several purposes, such as:
- Grip: Affixed to the skin, it enhances your capacity to grasp and cup objects.
- Protection: Preserves your hand’s tendons, muscles, blood vessels, and nerves.
- Origin and insertion: acts as the palmaris brevis tendon’s genesis and the palmaris longus tendon’s insertion site.
- The webs between your fingertips are supported.
Causes
- Genetics: It is known that there is a significant hereditary component. Usually, it runs in families.
- Age: As people age, the incidence rises.
- Gender: Men are more likely to have it.
- Ancestry: Those with Northern European ancestry are more vulnerable.
- Medical problems: A higher risk is linked to certain medical problems, including diabetes and seizure disorders.
- Lifestyle Factors: Drinking alcohol and smoking might also have an impact.
- Trauma: Although it is up for debate, some people think that hand trauma could cause or exacerbate the illness.
Sign and symptoms
Dupuytren’s contracture is the result of thickening and contraction caused by inflammation of the ulnar side of the aponeurosis. The fingers’ proximal and distal phalanxes—typically the third and fourth digits—flex as a result. The terminal phalanx is not impacted.
Nodules
- Nodules are tiny, solid lumps that form beneath the palm’s skin. These are frequently the first apparent symptoms.
- Usually, they show up around the base of the fingers.
Cords
- The nodules may become thicker and develop into tissue cords that run down the palm and into the fingers as the illness worsens.
- The fingers are drawn inward by these cables.
Contractures
- The gradual inability to straighten the fingers is the most distinctive sign.
- Although other fingers may occasionally be impacted, the ring and little fingers are most frequently impacted.
- This might lead to trouble with common tasks, such as holding objects, shaking hands, or placing hands in pockets.
Other Potential Symptoms
- The palm may occasionally feel sensitive or uncomfortable.
- There may be puckered or dimpled skin over the nodules.
Risk factor
- The risk rises with age, usually impacting people over 50.
- One important risk factor is a strong family history.
- More common in men than in women, and the symptoms are typically more severe in men.
- The disorder is more common in people of Northern European ancestry (English, Irish, Scottish, Scandinavian, etc.).
- Excessive alcohol use and smoking have been associated with increased risk.
- Repeated hand injuries or exposure to vibrations.
Elevated risk is linked to specific medical disorders, such as:
- Diabetes mellitus
- Seizure disorders
Treatment
Medical management
- Observation: In mild cases, when hand function is not significantly affected, observation might be the only necessary treatment.
- Corticosteroid injections: These injections can help nodule pain and inflammation by lowering inflammation.
They may slow the condition’s progression, but they don’t fix contractures that already exist.
- Collagenase Injections: This includes injecting an enzyme that breaks down the constricted cords, allowing the finger to be straightened. This is a minimally invasive option.
Needle aponeurotomy
- Needle aponeurotomy, also known as percutaneous needle fasciotomy, is a procedure that helps straighten fingers by breaking the tight cords with a needle. Additionally, this is a less invasive technique.
Physical therapy treatment
- Physical therapy can help improve strength and function in your fingers and hands, reduce swelling, and aid in wound care. A hand therapist will frequently create a splint for you to wear while you heal.
- The goal of physiotherapy treatment for palmar aponeurosis problems, which are mainly associated with Dupuytren’s contracture, is to restore hand function by addressing the contracted palmar aponeurosis that inserts into the base of the fingers and metacarpals. Early intervention is crucial to prevent further contracture development.
- The treatment involves manual stretching techniques, specific exercises to improve finger extension, splinting to maintain finger position, and modalities like ultrasound or heat therapy to soften the thickened fascia.
Manual treatment
- Soft tissue mobilization: Deep tissue treatments and mild massage to release tense fascia and surrounding tissues.

- Stretching methods: Targeting the affected fingers with the right placement, certain finger extension stretches gradually lengthen the constricted palmar aponeurosis.

- Cross-friction massage: May help encourage tissue remodeling and break down scar tissue.
- Active range of motion exercises: To increase joint mobility, perform mild finger flexion and extension movements.
- Isometric exercises: Strengthening the intrinsic hand muscles by contracting them against resistance.
Exercises that enhance hand coordination and finger position awareness are known as proprioceptive exercises. Exercise and stretching can support the preservation of a range of motion and flexibility.
Modalities
- Ultrasound therapy: To increase blood flow and potentially soften the thickened fascia
- Heat therapy: To improve tissue extensibility and reduce pain
Splinting

- Custom splints: Often with gradual modifications as the disease gets better, nighttime splinting is essential to preserve finger extension and stop additional contracture formation.
- Dynamic splints: These can be used later on to offer mild stretching while going about daily tasks.
Splinting is another option, albeit it isn’t proven to halt the disease’s progression. Bracing or splinting: This can help stretch the fingers.
Surgical treatment
Fasciectomy
- A fasciectomy is the surgical excision of the affected palmar fascia.
- More severe contractures that substantially limit hand function are usually taken into consideration.
Fasciotomy
- This surgical technique releases the contracture by cutting the cord, but it does not remove it.
Complication
- The severity of the contracture
- The quantity of contractures treated in a single operation
- The presence of any other medical conditions
- Pain
- Scarring
- Injury to nerves and/or blood vessels
- Wound infection
- Muscle Stiffness
- Momentary loss of feeling The stretching of long-contracture nerves can cause momentary loss of feeling.
- Finger loss or loss of viability (capacity to survive) (rare)
What functional similarities exist between a tendon and an aponeurosis?
A tendon functions similarly to an aponeurosis. Both of these serve to connect your muscles to your bones. An aponeurosis acts as a spring to withstand the strain and additional pressure when you flex or lengthen one of your muscles. When you move your muscles, it absorbs energy.
Your tendons, on the other hand, contract and stretch when your muscles move. Your tendon moves a bone when you exercise a muscle. Tendons provide you flexibility and allow your body to move. Your body’s aponeuroses provide stability and strength.
Furthermore, aponeuroses can function similarly to fascia, another kind of connective tissue. Your muscles, organs, and bones are supported by fibrous tissue called fascia.
FAQs
What is the purpose of aponeurosis?
Your muscles and bones are connected by a thin sheath of connective tissue called an aponeurosis. Tendons and aponeuroses are comparable. They provide stability and strength to your body by supporting your muscles. When your muscles contract, aponeuroses absorb energy.
What is the palmar fascia used for?
Palmar fascia: intricately woven fascia in the hand’s palm that protects the hand’s sensitive structures and is a component of the palmaris longus expansion.
What is the palmar ligament used for?
Along with the hand’s flexor retinaculum, the palmar carpal ligament—also known as the volar carpal ligament or Guyon’s Tunnel—is a thickened section of antebrachial fascia on the anterior/palmar side of the wrist that preserves the tendons of the majority of the hand’s flexor muscles.
What distinguishes the retinaculum from aponeurosis?
Similar to the aponeurotic fasciae, the retinacula are made up of two to three layers of parallel collagen fiber bundles; however, the fibrous bundles are packed more firmly and there is less free connective tissue in the retinacula.
What makes aponeurosis different from fascia?
It protects your blood vessels, muscles, bones, tendons, cartilage, and nerves. Compared to superficial fascia, this layer is thicker. This layer is divided into two subtypes: The aponeurotic fascia Thick, pearly-white aponeurotic tissue detaches from your muscles more readily.
What is the palmar nerve used for?
Among the branches of the median nerve are: Muscular branch: Which regulates action in the superficial muscles near the surface of the forearm. Deep (volar interosseous) branch: Regulates the forearm’s deeper muscles. The palmar branch transmits and receives sensory data between the thumb, palm, and a few fingers.
Are aponeuroses considered ligaments?
Fibroblasts are spindle-shaped cells that secrete collagen, and bundles of collagenous fibers are found in the dense fibrous connective tissue that makes up the aponeurosis.
Which three forms of fascia are there?
In addition to being categorized by physical location, fascia can be categorized as superficial, deep, visceral, or parietal. Directly beneath the skin and superficial adipose layers lies superficial fascia. It can display stratification at both the macro and microscales.
What’s the term for a flattened tendon?
Flatfoot deformity in adults: collapsed arches and flat…
An aponeurosis is a flattened tendon. Flat sheets of connective tissue called aponeuroses bind muscles to cartilage and bones. They provide strength and stability to the body by supporting muscles.
Reference
- Palmar aponeurosis (Longitudinal fibers; right) | Complete Anatomy. (n.d.). www.elsevier.com. https://www.elsevier.com/resources/anatomy/connective-tissue/fasciae/palmar-aponeurosis-longitudinal-fibers-right/22502
- Taylor & Francis. (n.d.). Palmar aponeurosis – Knowledge and References | Taylor & Francis. https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Anatomy/Palmar_aponeurosis/
- Professional, C. C. M. (2024a, May 1). Aponeurosis. Cleveland Clinic. https://my.clevelandclinic.org/health/body/23407-aponeurosis
- Wikipedia contributors. (2024b, May 16). Palmar aponeurosis. Wikipedia. https://en.wikipedia.org/wiki/Palmar_aponeurosis
- Palmar aponeurosis. (2024, May 6). Kenhub. https://www.kenhub.com/en/library/anatomy/palmar-aponeurosis
- Hacking, C. (2021). Palmar aponeurosis. Radiopaedia.org. https://doi.org/10.53347/rid-92470