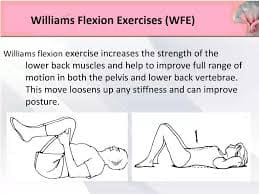
What is a Williams Flexion Exercises?
Williams back exercises, sometimes referred to as lumbar exercises or Williams flexion exercises, are a set of exercises designed to help people with low back pain. Unlike the McKenzie back exercises, which focus on lumbar extension, these exercises aim to strengthen the gluteal and abdominal muscles and enhance lumbar flexion in order to prevent the pain from growing worse.
The Williams Flexion Exercises are a well-researched approach that emphasises flexion-based exercises for the management and treatment of lower back pain. People with disorders including lumbar disc herniation, lumbar spondylosis, and general lower back discomfort can benefit most from these exercises. By lowering lumbar lordosis, the exercises hope to relieve strain on the spinal discs and nerves.
The purpose of the Williams Flexion Exercises, which were created by Dr. Paul C. Williams in the 1930s, is to strengthen the muscles that support the lumbar spine, increase flexibility, and reduce lower back pain.
For patients seeking non-surgical treatment to alleviate their low back pain, Williams’ back flexion exercises offer an option. Those who do not wish to have low back surgery can effectively address their back discomfort permanently with these workouts. Williams’s back flexion exercises have been recommended to patients over time, even in the lack of a definitive diagnosis, for a variety of ailments associated with low back pain. Physical therapists and doctors have created numerous variations of this exercise, which is primarily recommended by orthopaedics.
in contrast to the McKenzie exercise method, which uses motion to promote lumbar extension. In the 1930s, William’s Back Flexion Exercises and the McKenzie Method of Extension Exercises were established. Another name for the McKenzie exercise is mechanical diagnosis.
Historical Background and Evolution
These exercises were created in the 1930s by orthopaedic surgeon Dr. Paul C. Williams as a part of his groundbreaking work in orthopaedic medicine. Dr. Williams thought that people with lower back problems could benefit from a regimen of exercises that focus on spinal flexion, abdominal strengthening, pelvic positioning, and decompressing the spine to lessen the strain on the lumbar vertebrae and discs. Since then, back pain rehabilitation and physical therapy programmes have adopted his method as standard practice.
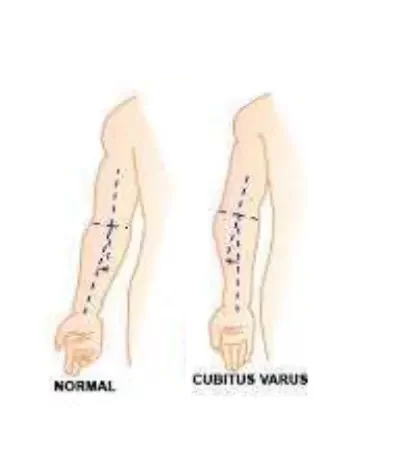
Originally designed for men under 50 and women under 40 with low-grade, persistent complaints and excessive lumbar lordosis, these workouts also indicated decreased disc space between lumbar spine segments (L1-S1).
Foundation Theory
The main idea underlying the Williams Flexion Exercises is that by decompressing the lumbar spine, specific postures and motions will lessen discomfort and enhance function. These exercises help to open up the intervertebral gaps, which can reduce strain on the discs and nerves by pushing the spine to bend forward.
Mechanisms of Williams flexion exercise
For a long time, the WFEs were the go-to method for treating low back pain without surgery.
These exercises were done on a floor or other level surface while the person was in the supine posture. Although there were several modifications, the main technique is to grab both legs, bring the knees to the chest, and hold them there for a few seconds. After a moment of relaxation, the patient lowers their legs and performs the exercise once more. The main advantages are thought to be the ligamentous structures being stretched, the apophyseal joints being distracted, and the intervertebral foramen opening.
These exercises aimed to stretch the hip flexors and lower back (sacrospinalis) muscles passively while actively increasing the “abdominal, gluteus maximus, and hamstring muscles as well as…” to alleviate discomfort and give lower trunk stability. Williams stated, “the workouts outlined will achieve an adequate equilibrium between the postural muscles’ flexor and extensor groups.” Williams proposed that the optimal position to do this was a posterior pelvic tilt.
Benefits:
There are several benefits to using Williams Flexion Exercises if you have lower back pain or want to strengthen your spine. These exercises have been extensively utilised and researched in physical therapy and rehabilitation settings with the goals of decreasing pain, increasing flexibility, strengthening muscles, adjusting posture, and improving general function. The following are Williams Flexion Exercises’ main advantages:
1. Pain Reduction:
- Reduces Back Pain: These exercises help to lessen discomfort related to disorders like disc herniation, spondylosis, and muscle strain by encouraging spinal flexion and decompression.
- Reduces Sciatic Pain: Williams Flexion Exercises help relieve sciatica symptoms brought on by nerve compression by stretching and mobilising the pelvic and lower back muscles.
2. Increased Flexibility:
- Increases Lumbar Spinal Mobility: By focusing on the lumbar spine’s muscles, ligaments, and joints, these exercises increase range of motion and flexibility.
- Improves Hip Flexibility: A lot of Williams Flexion Exercises include flexion and extension of the hips, which can aid with hip joint flexibility and mobility.
3. Muscle Strengthening:
- Strengthens Core Muscles: By using the stomach and back muscles, exercises including squats, pelvic tilts, and partial sit-ups enhance core strength and stability.
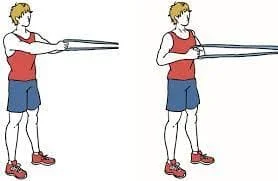
- Improves Gluteal Power: Exercises that target the gluteal muscles, which are essential for supporting the pelvis and lower back, include bridges and squats.
4. Posture Correction:
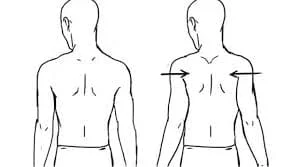
- Williams Flexion Exercises aim to correct lumbar lordosis by decreasing excessive lumbar curvature, establishing a more neutral spine alignment, and easing lower back discomfort.
- Improves Pelvic Alignment: These exercises help produce a more balanced posture and lessen the strain on the spine by treating concerns related to pelvic tilt and alignment.
5. Functional Improvement:
- Enhances Daily Function: Daily tasks like bending, lifting, and standing can be more comfortable and effective with stronger core muscles and increased flexibility.
- Reduces Disability: Williams Flexion Exercises can improve quality of life and lessen disability by addressing the underlying causes of lower back pain.
6. Preventive Maintenance:
- Reduces Risk of Injury: By enhancing posture, muscle strength, and flexibility, regular practice of these exercises can help avoid lower back issues.
- Maintains Spinal Health: Williams Flexion Exercises enhance long-term spinal health and lower the risk of degenerative disorders by increasing spine mobility and alignment.
7. Psychological Advantages:
- Decreases tension: A lot of these exercises include deliberate breathing and relaxation methods, which can lower tension and increase feelings of wellbeing.
- Empowers Individuals: Acquiring knowledge of and engaging in these exercises can enable people to actively manage their lower back pain and enhance their general health.
Williams Flexion Exercises address various facets of musculoskeletal function and mobility, providing a comprehensive approach to treating lower back pain and enhancing spine health. These exercises can be employed as preventative measures or as part of a rehabilitation programme, and they can offer substantial advantages and enhance the quality of life for those with lower back problems.
Principles of Williams flexion exercise:
The basis for Williams Flexion Exercises’ efficacy in treating lower back pain and enhancing spine health is their set of guiding principles. These guidelines direct the choice and implementation of workouts to meet certain therapeutic objectives while reducing the possibility of aggravating pre-existing diseases. The following are the main ideas behind Williams Flexion Exercises:
1. Spinal Flexion:
Core Principle: The main goal of the Williams Flexion Exercises is to encourage the lumbar spine’s flexion, or forward bending.
Justification: Spinal flexion relieves lower back pain by decompressing the spinal discs, relieving pressure on the spinal nerves, and opening up the intervertebral gaps.
Application: Exercises include postures that promote lumbar spine flexion, such as forward bends, knee-to-chest stretches, and pelvic tilts.
2. Abdominal Engagement:
Core Principle: During flexion movements, the lumbar spine needs stability and support, which is primarily provided by the abdominal muscles.
Justification: By controlling and stabilising the lumbar spine’s movement, using the abdominal muscles lowers the chance of overstretching or injury.
Application: To guarantee that the core muscles are properly engaged throughout the movement, exercises include abdominal bracing and activation strategies.
3. Gradual Advancement:
Core Principle: To encourage adaptation and prevent overexertion, exercise intensity and difficulty should be gradually increased over time.
Justification : Gradual progression lowers the chance of injury and promotes long-term improvements in strength and flexibility by enabling the muscles and connective tissues to adjust to increased demands.
Application: Resistance, repetitions, and range of motion are all adjusted as necessary to progress exercises based on personal tolerance and improvement.
4. Customized Method:
Core Principle: Individualized treatment programmes should take into account each patient’s unique needs, abilities, and limits.
Justification: Each person has distinct anatomical differences, functional limitations, and pain patterns that call for individualised evaluation and treatment.
Application: Based on the patient’s medical history, physical examination results, degree of discomfort, and functional goals, different exercises are chosen and adjusted.
5. Pain Management:
Core Principle: To prevent aggravating symptoms, exercises should be done within a pain-free range of motion and intensity.
Justification: Pain can impede progress and result in more injury, and it is frequently a limiting factor in exercise tolerance and adherence.
Application: Exercises should be performed by patients in their comfort zone, with adjustments made to lessen pain and prevent exacerbating underlying issues.
6. Conformity and Consistency:
Central Idea: To maintain development and attain the best results, exercise must be practiced consistently and on a regular basis.
Justification: Adherence to an exercise programme is essential for promoting the kinds of repetitive stimuli that are necessary for musculoskeletal adaptations over time.
Application: Patients receive techniques to include exercise in their daily routines as well as education regarding the significance of sticking to their exercise regimen.
Indication:
The majority of ailments and circumstances for which Williams Flexion Exercises are recommended are those involving lower back pain and dysfunction. These exercises aim to strengthen the muscles that support the lumbar spine, reduce pain, and increase flexibility. The main reasons to conduct Williams Flexion Exercises are listed below:
Indications:
Prolonged lower back pain:
Lower back pain that is persistent and lasts longer than three months.
Justification: By decompressing the spine and reducing lumbar lordosis, flexion exercises can help relieve chronic pain.
Herniation of the lumbar disc:
This is a disorder that causes pain, numbness, or weakness when the intervertebral disc protrudes and compresses the spinal nerves.
Justification: By releasing pressure from the herniated disc and spinal nerves, flexion exercises can ease pain.
Spondylosis in the Lumbar Region:
Osteoarthritis and disc degeneration are two examples of the degenerative processes that affect the lumbar spine.
Justification: Flexibility exercises might lessen the mechanical strain on the deteriorating components while also preserving spinal mobility.

Sciatica:
Pain that travels down the sciatic nerve, usually as a result of lumbar spinal stenosis or compression from a herniated disc.
Justification: Flexibility exercises can help relieve sciatica symptoms by relieving strain on the sciatic nerve and lower back.
Dysfunctional Posture:
Described as bad posture with an anterior pelvic tilt or severe lumbar lordosis (swayback),.
Justification: By reducing excessive lumbar curvature and adjusting pelvic alignment, flexion exercises help enhance posture overall.
Stenosis of the lumbar spine:
Description: Compression of the spinal cord or nerves due to lumbar region spinal canal narrowing.
Justification: By increasing spinal canal space, flexion exercises lessen compression and its related symptoms.
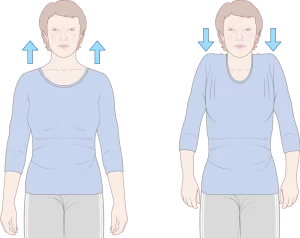
Weakness and imbalance of muscles:
Description: Tight lower back muscles are frequently accompanied by weak abdominal and gluteal muscles.
Justification: By strengthening the gluteal and abdominal muscles, these workouts enhance general balance and lumbar spine stability.
Rehabilitation following surgery:
Phase of recuperation after lumbar spine surgery, such as laminectomy or discectomy.
Justification: By gradually reintroducing movement with flexion exercises, one can promote healing, regain range of motion, and avoid complications following surgery.
Contraindications
Although many people with lower back discomfort benefit from Williams Flexion Exercises, there are some situations and conditions in which they might not be appropriate:
Acute Back Injury or Pain:
The injury or sudden onset of significant back pain.
Reason: Exercising while experiencing acute pain or injury can make it worse.
Osteoporosis Severe:
A disorder that is typified by fragile and feeble bones.
Reason: In people with severe osteoporosis, flexion motions may raise the risk of vertebral fractures.
Abrupt Spinal Instability:
Spondylolisthesis is one example of an extremely unstable spine condition.
Reason: Exercises involving flexion may exacerbate instability and raise the possibility of damage.
Certain Spinal Disorders That Need Extension
Spinal stenosis is one of the conditions that can benefit most from spinal extension exercises.
Reason: Exercises involving flexion may not be suitable and may even make symptoms worse.
Inflammatory or infectious spinal conditions:
Disorders such as spinal infections or inflammatory diseases in their active stage, such as ankylosing spondylitis.
Reason: An illness or inflammation may get worse with exercise.
The importance
Non-Invasive Approach: For people with lower back pain, Williams Flexion Exercises provide a conservative, non-invasive treatment alternative that lessens the need for invasive treatments or reliance on drugs.
Comprehensive Rehabilitation: By addressing several facets of lower back health, such as pain reduction, flexibility, strength, and posture correction, these exercises promote long-term back management and holistic rehabilitation.
Empowerment via Self-Care: Williams Flexion Exercises enable patients to actively participate in the management of their back pain and the promotion of spinal health by teaching them how to carry out specific exercises at home.
Preventive strategy: By preserving spinal health and muscular strength, regular practice of these exercises not only aids in the management of current lower back ailments but also acts as a preventive strategy against future problems.
Rationale:
According to Williams, improper posture puts stress on the intervertebral disc, which is the root cause of all pain. He postulated that the intervertebral disc’s early dysfunction was caused by the strain that the lordotic lumbar spine put on its posterior parts. He was worried about the disc injury resulting from the accumulation of extension forces caused by the lack of flexion in routine activities.
Williams flexion exercises (WFE) procedure:
These exercises were done on a floor or other level surface while the person was in a supine posture. Although there were several modifications, the main technique was to grab both legs, bring the knees to the chest, and hold them there for a few seconds. After that, the patient unwinds, lowers their legs, and performs the exercise once more. The main advantages are thought to be the ligamentous structures being stretched, the apophyseal joints being distracted, and the intervertebral foramen opening.
The following are some of Williams’ exercises:
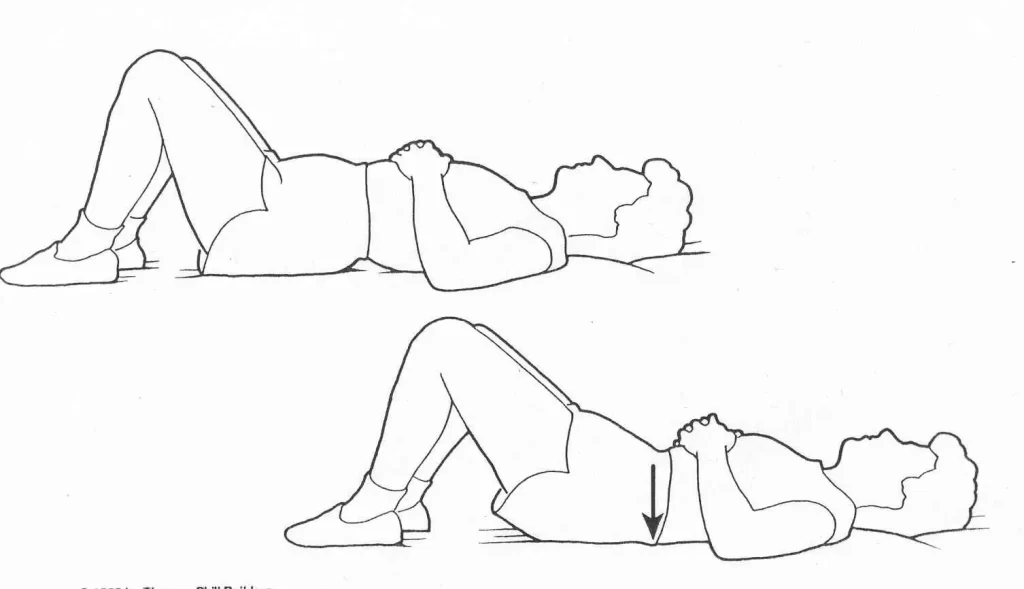
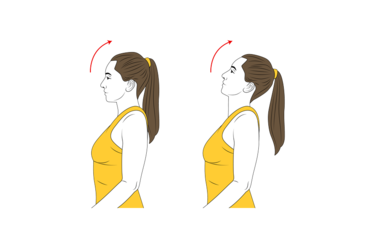
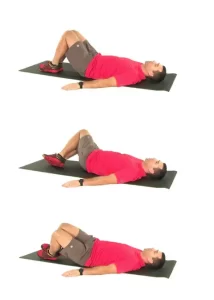
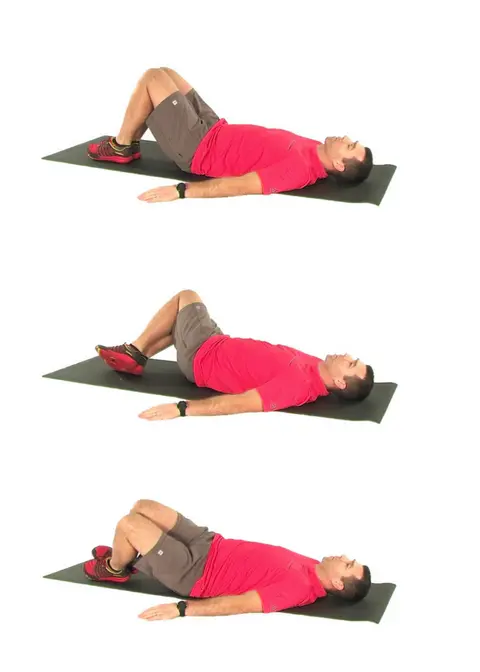
1. Pelvic Tilt Exercise
Goal:
discomfort relief: By decompressing the lumbar spine, lower back pain is lessened.
Strengthening: Works the muscles in the abdomen.
Posture correction: Enhances general posture and pelvic alignment.
Application:
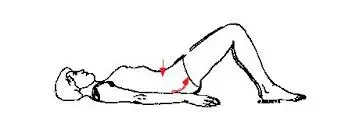
Beginning Position: arms by your sides, knees bent, feet flat on the ground, and you lying on your back.
Neutral Spine: Start with your lower back’s natural curve.
Pull your navel in the direction of your spine to engage your abs.
Pelvis Tilt: Press your lower back onto the floor by tilting your pelvis backward.
Hold: Hold the posture for ten to fifteen seconds.
Return: Unwind and take a seat again in the neutral position.
Repeats: Perform ten to fifteen repetitions, progressively increasing.
Advantages:
Improves Core: Focuses on and fortifies the muscles of the abdomen.
lessens the abnormal curvature of the lumbar spine (lordosis).
Enhances Alignment: Encourages appropriate pelvic and spinal alignment.
Improves Flexibility: Makes the pelvic and lower back muscles more flexible.
Basis: Provides support for more difficult workouts.
Advice: Move carefully and deliberately.
Continue breathing steadily.
For optimal outcomes, practice consistently.
2. Single Knee to Chest
Goal:
discomfort relief: By extending the gluteal and lower back muscles, this technique helps to reduce lower back pain.
Increases the lumbar spine’s and the hip flexors’ flexibility.
Lower back muscle tension can be reduced by practicing muscle relaxation.
Implementation:

Starting Position: Recline fully on your back, knees bent, feet straight on the floor.
Elevate One Knee: Gently raise one knee to your chest.
Hold Knee: Grasp the knee softly on the shin or below with both hands as you bring it gently up to your chest.
Hold the Position: Hold this posture for 15 to 30 seconds while bending the opposite leg so that it is flat on the floor and the foot is flat on the ground.
Return: Lower your leg gradually to its initial position.
Change Legs: Perform the same exercise using the other leg.
Repeats:
Repeat two to three times on each side, escalating the number of reps as tolerated.
Advantages:
Lower Back Stretch: This technique lengthens the muscles in the lower back, releasing tension and soreness.
Enhances Flexibility: Increases hip flexor, gluteal, and lower back flexibility.
Lessens Tension: This eases tense muscles, encouraging calmness and lessening discomfort.
Enhances Circulation: This promotes healing by increasing blood flow to the pelvis and lower back regions.
Advice:
Move lightly and slowly.
To avoid getting hurt, don’t pull too hard.
Breathe continuously for the entire exercise.
To get the most out of the stretch, keep the opposite leg loose.
3. Double Knee to Chest
Goal:
discomfort Relief: By extending the gluteal and lower back muscles, lower back pain is reduced.
Increases the lumbar spine’s and the hip flexors’ flexibility.
Muscle Relaxation: Encourages relaxation and eases tense muscles.
Implementation:
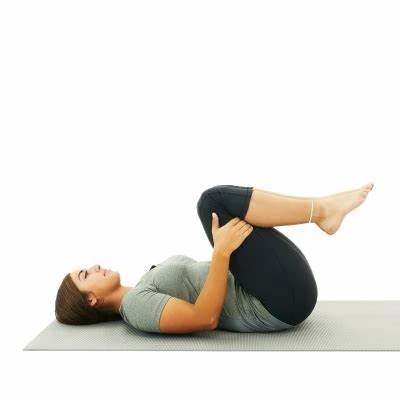
Starting Position: Recline fully on your back, knees bent, feet straight on the floor.
Raise Knees: Gradually raise both knees to your chest.
Hold Knees: Grasp your knees below the knees or on your shins with both hands as you slowly bring them closer to your chest.
Hold the Position: Keep your back flat against the floor and hold this position for 15 to 30 seconds.
Return: Return to the starting posture by lowering your legs gradually.
Repeats:
Do two to three repetitions, escalating the amount as tolerated.
Advantages:
Lower Back Stretch: By lengthening the lower back muscles, this technique relieves pain and tightness.
Enhances Flexibility: Boosts the flexibility of the hip flexors, gluteal muscles, and lower back.
Lessens Tension: Aids in lowering tenseness in the muscles, encouraging calmness, and lessening discomfort.
Enhances Circulation: Promotes healing and recuperation by increasing blood flow to the pelvic and lower back regions.
Advice: Move lightly and slowly.
Breathe continuously for the entire exercise.
For the best stretch, keep your back flat on the ground.
4. Partial Sit-Up.
Goal:
Strengthening the abdominal muscles that support the lumbar spine is known as core strengthening.
Spinal Stability: By using the core muscles, the lumbar spine becomes more stable.
Improves Posture: By fortifying the muscles that support the spine, this technique helps to improve posture.
Execution:

Recline fully on your back, knees bent, and feet straight on the floor. Cross your hands through your upper body or place them behind your head.
Engage Core: Pull your navel inside towards your spine to tighten your abdominal muscles.
Raise Shoulders: Keeping your lower back flat on the ground, carefully raise your head, neck, and shoulders off the ground. Raise just enough to lift your shoulder blades off the floor.
Hold Position: Keep your abdominal muscles engaged while holding this position for one to two seconds.
Return: Carefully and slowly reposition your shoulders, head, and neck to their initial positions.
Repeats: Do ten to fifteen repetitions, escalating the number as your strength increases.
Advantages:
Strengthens Core: Concentrates on the oblique and rectus abdominis muscles, which are crucial for sustaining the lower back.
Enhances Spinal Stability: By making the lumbar spine more stable, it lowers the chance of lower back pain and injuries.
Supports Posture: By fortifying the muscles that uphold appropriate spinal alignment, it aids in the improvement of posture.
Encourages Functional Movement: Develops the core strength required for everyday bending and lifting tasks.
Advice:
Controlled Movements: To prevent using momentum and guarantee appropriate muscle engagement, complete the exercise slowly and deliberately.
Breathing: Take a breath out as you raise your shoulders, then a breath back in as you take your initial posture.
Neck Support: Refrain from pulling with your hands on your neck. Make sure to use your abdominal muscles while lifting.
Maintaining consistency is essential to developing core strength and reaping the advantages of exercise.
5. Hamstring stretch
Goal:
Flexibility: Develops hamstring flexibility, which helps release tension in the pelvis and lower back.
Lower Back Relief: Reduces hamstring tightness, which may aggravate lumbar strain, and helps ease lower back pain.
Enhances Improves posture by addressing hamstring tightness, which can pull on the pelvis and alter the alignment of the spine.
Implementation:

Beginning Position: Extend both legs down the floor while lying on your back.
Bend Knee: Place one foot flat on the ground and bend the knee.
Raise Leg: Gently bring the other leg up to your chest while maintaining its straight posture.
Hold Position: Feel a light stretch in the back of your leg (hamstring) and hold the stretch for 15 to 30 seconds at a comfortable tension.
Return: Lower your leg gradually to where you started, then switch to the other side.
Reps: Do two to three sets on each leg, escalating the number of reps as tolerated.
Advantages:
Enhances Hamstring Flexibility: This exercise stretches the hamstrings, increasing their range of motion and easing back thigh tension.
Reduces Lower Back Tension: This technique helps to relax the hamstrings, which can lessen the strain on the pelvic and lower back.
Improves Postural Alignment: By treating tense hamstrings, which can lead to postural abnormalities, this technique improves spinal alignment.
Enhances Hip Range of Motion: This enhances hip joint range of motion, promoting general mobility and function.
Advice:
Maintain Straight Back: To properly target the hamstrings and avoid putting tension on the spine, maintain a straight back during the stretch.
Breathe Deeply: To encourage relaxation, take a deep breath before beginning the stretch, and then release it gradually as you bend forward.
Adjust as necessary: You can rest your hands on your thighs or shins and concentrate on keeping your back straight if you are unable to touch your toes.
Consistency: To sustain and gradually increase your flexibility, incorporate sitting hamstring stretches into your regimen on a regular basis.
6. Squatting exercise
Goal:
Strengthens Lower Body: This exercise focuses on building strength and stability in the muscles of the legs, hips, and buttocks.
Enhances Flexibility: This improves mobility by making the hips, knees, and ankles more flexible.
Activates the core muscles to support posture and spinal alignment, which improves core stability.
Functional Movement: Encourages functional strength by simulating commonplace actions like bending and lifting.
Implementation:

Starting Position: Place your toes slightly outward while standing with your feet shoulder-width apart.
Engage Core: To stabilize your spine, tense your abdominal muscles.
Lower Body: Lower your body towards the ground by bending your knees and hips to begin the squat.
Depth: Keep your thighs parallel to the ground or slightly lower as you drop your body as far as is comfortable.
Knees and Toes: Make sure your knees do not buckle inward and that they track over your toes.
Maintain Posture: Throughout the exercise, keep your shoulders back, spine neutral, and chest elevated.
Press Through Heels: To get back to the starting position, straighten your hips and legs by pushing through your heels.
Repetition is key. Continue squatting for the required number of times.
Repeats: As strength increases, progressively increase the number of repetitions from 10 to 15.
Advantages:
Strengthens Lower Body: Promotes general lower body strength by focusing on the quadriceps, hamstrings, glutes, and calves.
Improves Core Stability: When squatting, the lower back and abdominal muscles are used to support the spine.
Enhances Joint Health: Lowers the chance of injury by promoting hip, knee, and ankle mobility and stability.
Enhances Functional Strength: By imitating everyday movements like bending, lifting, and sitting, functional strength is improved.
Advice:
Maintain Form: Pay close attention to correct form, keeping your back straight, knees in line with your toes, and chest high.
Controlled Movements: To maximise muscle engagement and minimise the chance of injury, lower and elevate your body slowly and deliberately.
Adjust Depth: Only go as low as is comfortable without hurting yourself or your form. Increase depth gradually as your strength and flexibility grow.
Breathing: Take a breath as you go down into the squat, then release it as you stand back up.
Use Support: Until you have enough strength and balance, you can, if necessary, use a chair or wall as support.
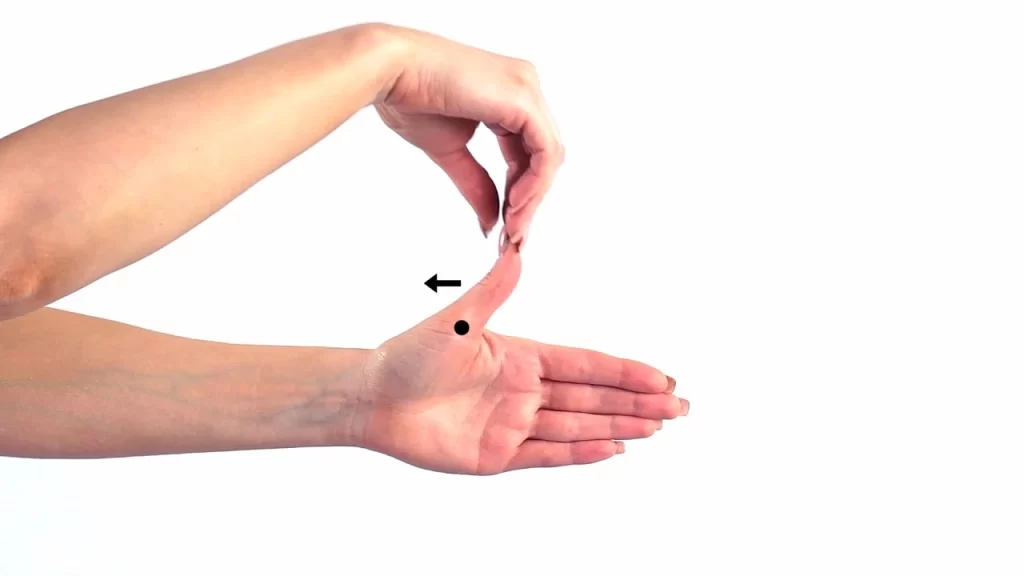
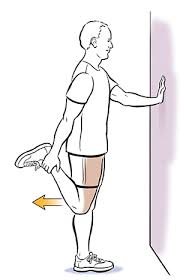
7. Hip Flexor Stretch
Goal:
Flexibility: Promotes greater range of motion in the hip flexor muscles, which might tense up after extended periods of sitting or exercise.
Diminished Reduces back strain by releasing tension in the hip flexors, which helps ease lower back pain.
Better Posture: Treats hip flexor tension, which can lead to pelvic tilt and improper spinal alignment.
Implementation:

Beginning Position: Lie on your back with your legs extended 90 degrees in front of you and 90 degrees behind you to form a triangle with your shin and thigh.
Engage Core: To stabilise your spine, contract your abdominal muscles.
Change of Weight: With your knee bent, gently move your weight forward and lean onto the leg’s hip.
Feel the Stretch: With your leg straightened, you should feel a stretch in the front of your hip and thigh.
Hold Position: Keep your posture tall and concentrate on feeling the stretch in your hip flexors for a duration of 15 to 30 seconds.
Return: Return to the starting position after releasing the stretch gradually.
Change Sides: By moving your legs to the opposite position, repeat the stretch on the opposite side.
Repeats: Do two to three sets on each side, escalating the number of reps as tolerated.
Advantages:
Boosts Hip Flexor Flexibility: This exercise stretches the hip flexor muscles, which helps to release tension and increase range of motion.
Reduces Lower Back Tension: Reduces lower back strain by relieving the tightness in the hip flexors.
Encourages Postural Alignment: Treats hip flexor tightness, which may be a factor in poor spinal posture and pelvic tilt.
Enhances Mobility: Promotes more functional movement patterns by enhancing hip joint mobility.
Advice:
Maintain Proper Posture: Throughout the stretch, try not to overly arch your lower back and maintain a tall spine.
Concentrate on Breathing: As you get ready for the stretch, take a deep breath, and as you relax into the stretch, release it slowly.
Increase Intensity Gradually: Take your time and go easy on the stretch; don’t force yourself into pain or discomfort. Increase the intensity gradually as your flexibility increases.
Remain Aware: To ensure a comfortable yet effective stretch, pay attention to how your body feels during the pose and modify the intensity as necessary.
8. Lumbar Flexion with Rotation
Goal:
Spinal Mobility: Encourages the lumbar spine to be flexible and mobile.
Stretching: Promotes relaxation and eases tension by focusing on the lower back muscles.
Activating the core muscles helps maintain posture and spinal stability.
Functional Movement: Enhances functional strength by imitating the twisting motions performed in daily activities.
Implementation:
Beginning Position: Recline fully on your back, knees bent, and feet straight on the floor.
Participate Core: To stabilise your spine, contract your abdominal muscles.
Flexion: As you slowly lift both of your knees to your chest, your lower back will flex slightly, or lumbar flexion.
Rotation: Keeping your knees together, slowly flex them to one side until your buttocks and lower back are comfortably stretched. Maintain a level shoulder-to-floor position.
Hold Position: While taking deep breaths and letting go of tension, hold the stretch for 15 to 30 seconds.
Go back to the center. Return your knees to the centre slowly.
Repeat on the Other Side: Lower your knees to the opposite side while carrying out the same motion.
Repeats:
For each side, begin with two to three repetitions, and then increase as tolerated.
Advantages:
Spinal mobility: expands the lumbar spine’s range of motion and flexibility.
Lower back tightness is released by muscle relaxation, which encourages relaxation and lessens stiffness.
Core activation involves using the muscles in the core of the body to maintain good posture and spinal stability.
Functional Strength: Enhances mobility and strength by imitating twisting motions performed in daily tasks.
Advice:
Preserve Control: To prevent putting undue tension on the lower back, move slowly and deliberately.
Pay Attention to Your Body: Don’t force the stretch; instead, only bend your knees as far as it feels comfortable.
Breathe Deeply: As you get ready for the stretch, take a deep breath, and as you bend your knees to the side, release it gradually.
Maintain Shoulders Down: To get the most out of the lower back stretch, make sure your shoulders stay level with the floor during the rotation.
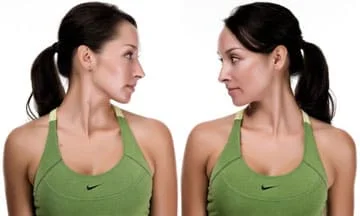
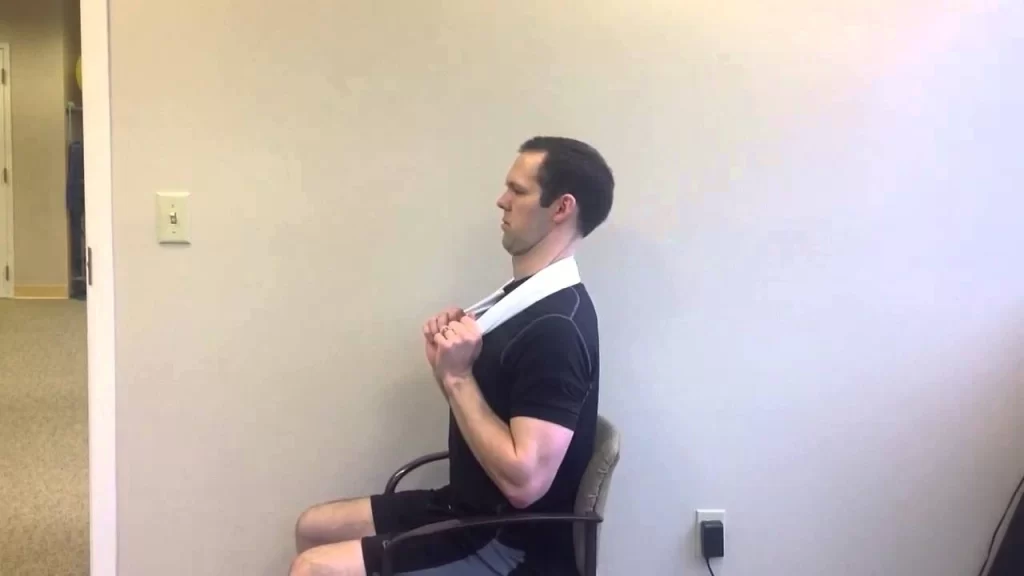
9. Lumbar Flexion While Seated
Goal:
Spinal Mobility: Encourages the lumbar spine to be flexible and mobile.
Stretching: Promotes relaxation and eases tension by focusing on the lower back muscles.
Activating the core muscles helps maintain posture and spinal stability.
Better Posture: Assists in mitigating the negative impacts of extended sitting and sedentary habits.
Implementation:

Beginning Position: Take a seat in a chair and place your feet hip-width apart, flat on the ground. Maintain a neutral posture with your spine straight.
Engage Core: To stabilize your spine and pelvis, tighten your abdominal muscles.
Bending: Gradually extend your hips forward, enabling your back to curve slightly (lumbar flexion). First, maintain a straight back; later, bend it to the desired degree of comfort.
Reach Forward: Stretch your arms out in front of you, reaching for your shins or feet. You can grab your feet or ankles if it’s comfortable for you.
Hold Position: While taking deep breaths and letting go of tension, hold the stretch for 15 to 30 seconds.
Get Back to Your Correct Position: To raise your body back up to the beginning position, gradually contract your core muscles.
Repeats:
Begin with two to three repetitions, and then increase as tolerated.
Advantages:
Spinal mobility: Expands the lumbar spine’s range of motion and flexibility.
Lower back tightness is released by muscle relaxation, which encourages relaxation and lessens stiffness.
Core activation involves using the muscles in the core of the body to maintain good posture and spinal stability.
improved Posture: By extending the lower back and encouraging improved spinal alignment, this posture helps mitigate the negative effects of extended sitting.
Advice:
Preserve Control: To prevent putting undue tension on the lower back, move slowly and deliberately.
Breathe Deeply: Take a deep breath before beginning the stretch, and release it gradually as you bend forward to achieve the stretch.
Adjust as Needed: If reaching for your feet is too difficult, try placing your hands on your thighs or shins and concentrating on keeping your back flat.
Pay Attention to Your Body: Don’t force the stretch; instead, only bend forward as far as feels comfortable.
Conclusion
In conclusion, the programme for Williams Flexion Exercises provides a thorough method for enhancing spine health and lowering back pain. People can improve flexibility, strengthen their core muscles, and encourage better posture by combining a range of exercises like pelvic tilts, single and double knee-to-chest stretches, partial sit-ups, hamstring stretches, squatting, hip flexor stretches, lumbar flexion with rotation, and seated lumbar flexion.
These exercises focus on the abdominals, lower back, hips, and hamstrings—important muscle groups that support the spine. Their goals are to lessen discomfort and enhance function in day-to-day tasks by reducing muscle tension, improving general spinal alignment, and increasing flexibility.
For the Williams Flexion Exercise programme to provide the most possible results, consistency and appropriate technique are crucial. People can promote their spine health, lower their risk of injury, and improve their quality of life by routinely performing these exercises.
FAQs
What is the programme for Williams Flexion Exercises?
A set of therapeutic exercises called the Williams Flexion Exercise programme is intended to encourage better posture, lessen lower back discomfort, and enhance spine health. Dr. Paul C. Williams created these exercises, which focus on the abdominals, lower back, hips, and hamstrings—important muscle groups that support the spine.
The Williams Flexion Exercise programme is beneficial for whom?
For those with lower back pain or those looking to enhance their spinal health, people of all ages and fitness levels can benefit from the Williams Flexion Exercise programme. People with degenerative disc disease, spinal stenosis, herniated discs, or chronic lower back pain are frequently advised to have it.
Is the Williams Flexion Exercise programme safe to perform?
The majority of people find that the exercises in the Williams Flexion Exercise programme are safe when done appropriately and under the supervision of a licenced healthcare provider. But it’s crucial to pay attention to your body, go cautiously at first, and refrain from any actions that make you feel pain or discomfort. Before beginning the programme, discuss any worries or underlying medical conditions with a healthcare provider.
How often should I perform the exercises for Williams Flexion?
Williams Flexion exercise frequency can vary based on personal needs and objectives. For optimal effects, it is generally advised to execute the exercises three to four times a week at minimum. Maintaining consistency is essential to improving the health of your spine and lowering your back pain.
Can I do other types of exercise in addition to the Williams Flexion Exercise programme?
Absolutely, you can mix the Williams Flexion Exercise programme with other workout regimens like yoga, weight training, or cardio. But it’s crucial to make sure the workouts work well together and don’t aggravate any pre-existing back problems. For individualised advice, speak with a licenced fitness instructor or healthcare provider.
How long does the Williams Flexion Exercise programme take to show results?
The Williams Flexion Exercise programme can take a while to show effects, depending on a number of personal circumstances, including consistency, following the right form, and the severity of pre-existing spinal problems. After beginning the programme, some people can see improvements in their lower back discomfort and spinal mobility in a few weeks, while others might take longer. Achieving long-term benefits requires perseverance and patience.
Is there a programme of Williams Flexion Exercise that should not be followed?
Although most people may safely follow the Williams Flexion Exercise programme, certain people may not be able to, including those who have severe spinal problems, have just had spine surgery, or have recently sustained an acute injury. Before beginning the programme, it is imperative that you speak with a healthcare provider, particularly if you have any underlying medical conditions or concerns.
Does the Williams Flexion Exercise programme address issues such as herniated discs or sciatica?
Absolutely, people with herniated discs or sciatica may benefit from the Williams Flexion Exercise programme. These exercises can help relieve symptoms, lessen pain, and enhance functional movement by focusing on important muscle groups that support the spine and encourage spinal mobility. To get personalised advice and make sure the exercises are suitable for your particular condition, it’s imperative to speak with a healthcare provider.
Are the Williams Flexion exercises modified for people with restricted mobility or flexibility?
Absolutely, the Williams Flexion exercises can be altered to meet the needs of those with restricted mobility or flexibility. People who struggle with floor exercises, for instance, can adjust by utilising a chair or bed for support. Furthermore, as flexibility increases, exercises can be modified to progressively increase intensity. Based on each person’s unique demands, a trained healthcare provider or fitness instructor can offer advice on suitable changes.
Are pregnant mothers able to participate in the Williams Flexion Exercise programme?
Pregnant women can safely perform some of the exercises in the Williams Flexion programme, but it’s important to speak with a healthcare professional before beginning any fitness programme. To preserve the safety of the mother and unborn child, some activities, such those that require deep twisting movements or resting flat on the back, may need to be adjusted or avoided during pregnancy. A medical professional can offer tailored advice depending on a patient’s health and pregnancy stage.
Can lower back discomfort be avoided by using the Williams Flexion exercises as a prophylactic measure?
Yes, you can use the Williams Flexion exercises as a prophylactic to strengthen the muscles that support your spine, increase your range of motion, and encourage improved posture. People can lessen their risk of lower back discomfort and preserve good spine health by including these exercises in a regular workout regimen. To fully benefit from the preventive effects of the Williams Flexion Exercise programme, consistency and appropriate technique are essential.
References:
- Pt, B. S. (2024, February 16). Williams Low Back Flexion Exercise. Verywell Health. https://www.verywellhealth.com/low-back-flexion-exercise-2696191
- Williams Flexion Exercises. (2023, September 9). Wikipedia. https://en.wikipedia.org/wiki/Williams_Flexion_Exercises
- Chauhan, S. (2022, February 12). William’s Flexion exercises: Goals, Indication, Contraindication. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/williams-flexion-exercises-indication-contraindication/
- Dhameliya, N. (2023, July 15). Williams flexion exercise (WFE) – Treatment of Back Pain. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/williams-abdominals-exercise/
- Physiotherapist, N. P. (2023, July 25). Low Back Flexion Exercise benefits, Low Back Pain Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/low-back-flexion-exercise-williams-flexion-exercise/
- Physiotherapist, N. P. (2023a, July 16). Williams Flexion Exercise (WFE) – For Treatment of Low Back Pain. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/williams-flexion-exercise-wfe/
- Bayramov, U. D. T., & Bayramov, U. D. T. (2023, November 14). Williams Exercises for Treatment of Lower Back Pain. Algoloji Uzmanı Dr. Tural BAYRAMOV – Kronik Ağrıların Tanı Ve Tedavisi. https://www.algolojiuzmani.com/williams-exercises-for-treatment-of-lower-back-pain/
- williams flexion exercises. (n.d.). https://www.physiotherapy-treatment.com/williams-flexion-exercises.html