Introduction
Hypnotherapy is a therapeutic technique that uses hypnosis to help individuals tap into their subconscious mind and bring about positive changes. By guiding individuals into a deep state of relaxation and heightened focus, hypnotherapy allows them to explore thoughts, feelings, and memories that may be difficult to access in a normal state of awareness.
Increased focus and concentration are hallmarks of hypnotherapy. Under the supervision of a qualified, experienced hypnotist or hypnotherapist, hypnosis makes you more receptive to recommendations for healthily altering your memories, thoughts, feelings, actions, perceptions, and sensations.
Explain to the client the operation and what they can expect before entering the operation and the interpretation of the test result is used to create a hypnotic state in the client you lead to this deep level of focus and relaxation. Tests are used to assess the level of emotional and physical suggestibility. There are four stages of hypnosis: induction, deepening, concentration, and emergence. The client could get self-hypnosis conditioning training.
Induces a hypnotic state in clients to change behavioral patterns, To improve motivation, talk about the case’s nature with the patient, To increase motivation, discuss the case’s nature with the client.
It is occasionally incorporated into phobia and other anxiety condition treatment programs. Along with many other uses, it is occasionally used for pain relief, weight reduction, and quitting smoking.
The problems that hypnosis can cure, its potential applications, and its potential efficacy in comparison to other therapies have all been investigated by contemporary researchers.
What is hypnosis?
Deep relaxation and concentrated attention are hallmarks of hypnosis, also known as hypnotherapy.
Through verbal cues, repeating it constantly, and visualization(through images), a proficient and certified hypnotist or hypnotherapist lets you into achievement of a deep state of focus and calmness. This extreme attention and concentration during hypnosis enable you to block out everyday distractions and be more receptive to directed advice on how to enhance your health.
Procedure Specifics
What usually takes place during a session of hypnosis?
Hypnosis progresses through four stages:
Introduction
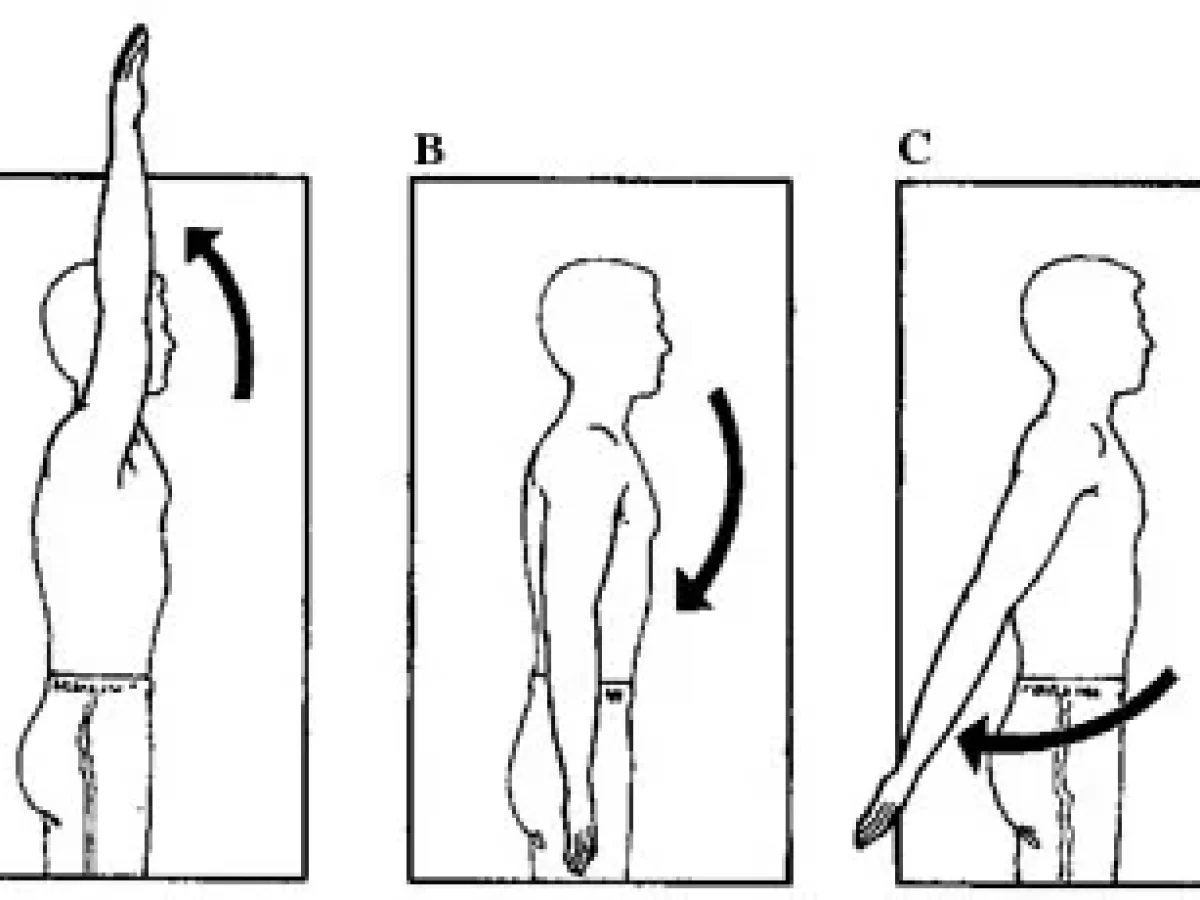
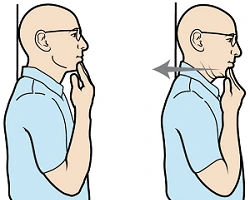
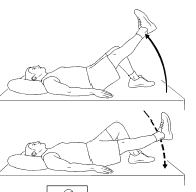
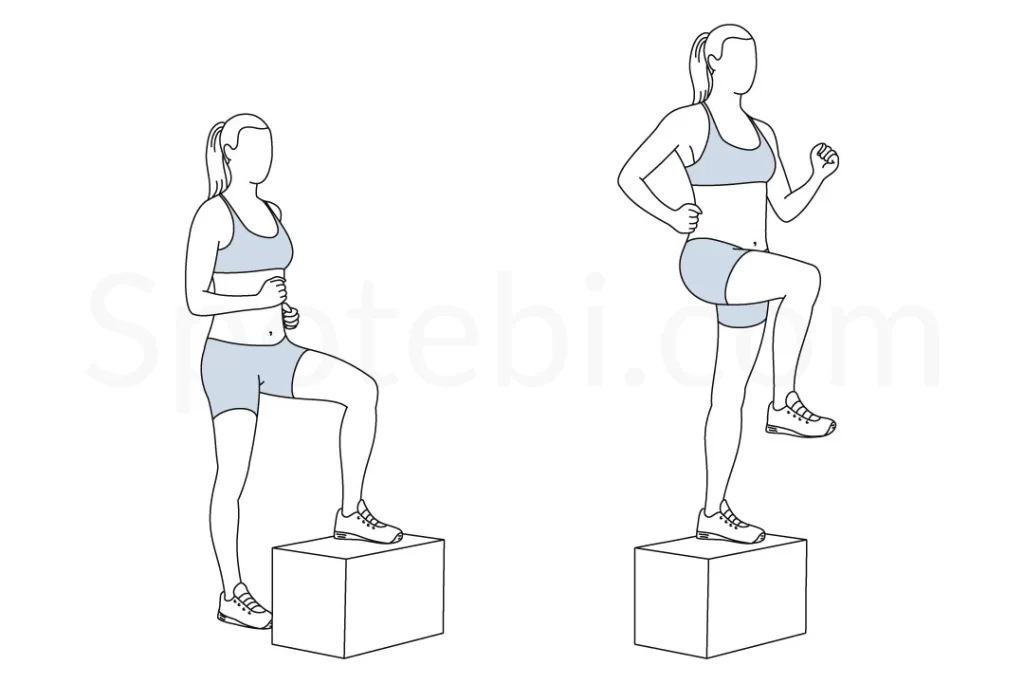
You start to calm down, concentrate, and block out distractions during this phase. and techniques such as progressive muscle relaxation (contracting the muscles during inhalation and relaxing the muscles during exhalation, then repeating in a series of muscle groups throughout the body), and controlling breathing (breathing). (count to seven, then divide by eleven) or a video image will help you in this section.
The Deepener
This step builds on the previous step and deepens concentration and relaxation. This stage frequently entails counting down or imagining a comparable descent, like going downstairs or gradually falling deeper and deeper into a cozy bed. The initial two phases aim to help you become more open to suggestions.
Suggestions
This is where experience, behavior, or thinking changes. Your hypnotist will employ well-chosen words and images. The instructions are usually exploratory (to examine events related to the start of a symptom) or target-specific (to fix a single symptom). Changes in perception, feelings, emotions, memory, thinking, or behavior are considered.
To quit smoking, for instance, you will learn how to recognize what makes you want to smoke, how to change in a good way, how to use resources to change, how to break your habit, how to respond better, how to notice the difference, and how to implement the new behavior. You might be encouraged to look into a mirror behind you to see your “old” self with unhealthy black lungs, while a mirror in front reflects your “new” healthy self with clear lungs.
After that, you’ll receive guidance on which self you like and how to move toward it.
The emergence
At this point, you awaken from hypnosis. Your attacker may use reverse immersion techniques, such as pretending you are counting or climbing.
Approaches to Hypnotherapy
People are led through a procedure to create a trance-like condition during a hypnotherapy session, which aids in mental focus, increased receptivity to suggestions, and profound relaxation. Through the increased awareness of the hypnotic state, hypnotherapy helps you concentrate more intently on an issue. Techniques used in hypnotherapy include:
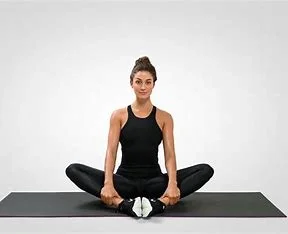
Relaxation: The hypnotherapist can help you picture yourself in a calm and relaxed condition, especially when dealing with troubling behavior or the object of your fears.
Advice: Your hypnotist could offer tactful recommendations for altering your behavior to assist you overcome your problem. For instance, you could be instructed to believe in yourself and your capacity to overcome the circumstance.
Coping mechanisms: Some cognitive-behavioral coping mechanisms include guided imagery and then one may utilize the STOP! approach to face your anxiety or fears.
Examining previous experiences: You could even be invited to discuss how you initially encountered the habit or issue you’re attempting to resolve, as well as your current feelings.
Is hypnosis the only kind of treatment?
As part of a comprehensive approach, hypnosis is typically utilized in conjunction with other therapies and treatments.
As part of a comprehensive therapy approach, hypnosis is typically utilized in conjunction with other therapies and treatments. A certified professional who has received training in the use and limits of hypnotherapy is consulted before deciding to employ it in a therapeutic environment as the only treatment or as an adjunct in psychotherapy or traditional medicine.
How long does hypnotherapy treatment usually last?
A normal length does not exist. The course of treatment will be processed by the type and up to how critical the problem is. Numerous sessions may be required for hypnotherapy.
How do you organize
Hypnosis doesn’t require any particular preparation on your part. To help you relax, it’s a good idea to dress comfortably. Make sure you get enough sleep. You’ll be less inclined to nod off throughout the session in this manner be relaxing. be relaxing. Select a medical professional with hypnotherapy certification. It’s advisable to get a recommendation from someone you trust. Find out more about any potential provider. Pose queries like:
- Have you had any specific hypnosis training?
- Do you have a license in this particular state for your specialty?
- How much hypnosis training have you received? Which schools are they from?
- You’ve been doing hypnosis for how long?
- How much do you charge? Are your services covered by insurance?
What to anticipate
Your healthcare physician goes over your treatment objectives and the hypnosis procedure with you before you start. The therapist usually starts by speaking in a soft, calming voice and explaining pictures that evoke feelings of calm, safety, and well-being. be relaxing.
Your healthcare professional makes recommendations for how you can accomplish your objectives while you’re at ease and content. For instance, strategies to lessen discomfort or lessen the desire to smoke may fall under this category. The service can also assist you in conjuring up clear, significant mental pictures of yourself achieving your objectives.
You might be able to free yourself from hypnosis when the session is completed. Alternatively, your healthcare practitioner could assist you in increasing your level of attentiveness gradually and gently.
People do not lose control of their conduct when under hypnosis, unlike what you may witness in movies or during a hypnotist stage show. During a session, they often stay conscious and recall what transpires. be relaxing. You could eventually be able to self-hypnose. Without the assistance of a medical professional, self-hypnosis allows you to achieve a state of peace and relaxation. This ability can be useful in a variety of circumstances, including before surgery or other medical treatments.
Findings
People can manage their pain, worry, and anxiety with the use of hypnosis. However, keep in mind that medical professionals usually recommend other therapies, including cognitive behavioral therapy, for those disorders either before or in addition to hypnosis. When used in conjunction with a more comprehensive treatment approach, hypnosis may be useful for weight loss or smoking cessation.
Not everyone is a good candidate for hypnosis. Not everyone can enter a deep enough state of hypnosis to make it useful. In general, people are more likely to benefit from hypnosis if they can relax and get quiet throughout a session more quickly and readily.
Why it’s carried out
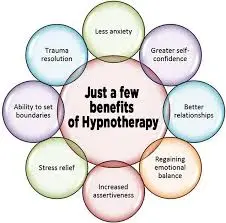
Stress and anxiety can be effectively managed by hypnosis. It may help reduce tension and anxiety, especially before a medical treatment like a breast biopsy.
Additionally, hypnosis might be useful for:
Pain management. Burns, cancer, childbirth, fibromyalgia, irritable bowel syndrome, jaw issues, dental operations, and headaches can all be less painful with hypnosis.
bursts of heat. Menopausal heat flashes may be lessened with hypnosis.
Modification of behavior. Sleep issues, bedwetting, smoking, and overeating have all been treated using hypnosis with varying degrees of effectiveness.
adverse effects of cancer therapy. The negative effects of radiation and chemotherapy have been lessened by hypnosis.
mental health issues. The anxiety brought on by phobias and anxieties may be lessened by hypnosis.
Advantages of Using Hypnosis in Therapy
Hypnotherapy may provide remarkable outcomes for certain individuals. In other cases, people may just feel exceedingly comfortable. The following are some possible advantages of hypnotherapy:
Some folks stay completely conscious during the whole encounter. They can even carry on conversations while in hypnosis and remember everything that occurs. Some people could get into profound levels of relaxation where they even feel cut off from reality.
Focus: We are frequently sidetracked by our environment. No matter how loud the TV is, your children are when your partner wants to chat or demands attention, it might be a sign that their mind is busy as well. You can feel anxious about an impending project, nervous about paying a bill, or preparing the meal for tonight. The goal of the treatment session is to overcome these daily issues and enable you to give the current issue your full attention.
Relaxation: When you are under hypnosis, you are incredibly relaxed. It facilitates your unconscious mind’s focus on your problem by relaxing your conscious mind. You are also more calm, which allows you to face your problems or fears more honestly. “You are safe” and “No one can harm you” are among the soothing phrases that most hypnotherapists use to comfort their clients so that they can address their issues honestly and without panicking when in hypnosis.
Is Hypnotherapy Effective?
Depending on the patient and the way the treatment is administered, hypnotherapy can have different effects and levels of efficacy. For various uses, hypnotherapy has been demonstrated to be somewhat effective, especially:
- Controlling and minimizing pain during dental treatments and delivery
- decrease in nausea and vomiting in patients receiving chemotherapy for cancer
- decrease in the intensity of irritable bowel syndrome (IBS) symptoms4.
- It could be most effective when used in conjunction with first-line therapies like cognitive behavioral therapy (CBT) and pharmaceuticals, even if it might assist patients deal with stress and anxiety-related issues.
According to research findings in the Journal of Affective Disorders’ May 2021 edition, hypnotherapy was just as successful as cognitive behavioral treatment (CBT) in treating mild to moderate depression. The study found that hypnotherapy reduced symptom severity by 44.6%, while cognitive-behavioral therapy reduced it by 38.5%.
Warnings
Although hypnotherapy is usually well-tolerated and safe, there are still some possible hazards, including:
- Hypnosis may be ineffective for those suffering from psychotic symptoms that consist of delusions and hallucinations.
- Under hypnosis, highly suggestible people may feel less in control of their own lives.
- Side symptoms including headaches, dizziness, or anxiety are possible for some people.
- Hypnosis may be unhelpful for people undergoing psychotic symptoms including delusions and hallucinations.
- These factors make it crucial to always get medical advice before using hypnosis. Additionally, make sure you only attempt hypnosis under the supervision and direction of a trained expert.
Common Misconceptions
Many mental health specialists continue to debate the efficacy of hypnotherapy. Myths and misunderstandings regarding hypnotherapy might influence how people perceive this therapeutic method.
Hypnotherapy is frequently mistaken for stage hypnosis. Stage hypnotists are competent entertainers who understand their audiences. They look for extroverts who can put on a terrific show for the audience. Although it’s unclear if the individuals are actually hypnotized, they are eager to follow the stage hypnotist’s often extreme instructions.
Hypnotherapy doesn’t make you forget what occurred. During hypnosis, you will recall events, remain awake, and have the ability to exit the trance at a time.
Hypnotherapy does not make you lose control. During hypnosis, you maintain control. Even as the process of hypnosis is on, you cannot be manipulated to do anything you do not want to. You may be focused on your task and not notice your surroundings, but you are always responsible for your actions, behaviors, and words.
Being hypnotizable does not imply you are less intellectual. Contrary to common opinion, research shows that most people can be hypnotized to some level.
What the experts say
According to Steve G. Kopp, a professional mental health counselor, and marital and family therapist, hypnotherapy is most effective when combined with other therapeutic methods. It can diminish a patient’s resistance to more standard therapies.
Depression, as well as other chronic mental diseases like bipolar disorder and schizophrenia, can hurt physical health. Depression encompasses more than simply sadness and bad thoughts. It is a disorder characterized by chemical imbalances in the brain.
How to Get Started
There are various options for finding a reliable hypnotherapist. Finding a practitioner by word of mouth is always a reliable method. Your mental health professional is a registered hypnotherapist or you know one.
If you know anyone who has gone through this form of therapy, inquire about their experiences. It’s important to note that certain hypnotherapists specialize in specific conditions, so a friend’s recommendation may not be appropriate for you.
While hypnosis remains controversial in certain areas, many professionals feel it may be effective. Discuss this treatment choice with your physician. Before proceeding, verify with your insurance carrier since some may not cover this.
Overview
Hypnosis enhances attention and concentration by altering consciousness and relaxing the mind. It’s also called hypnosis. Hypnosis is frequently conducted under the guidance of a healthcare professional, including vocal repetition and mental images. Most people experience a sense of serenity and relaxation while hypnotized. Hypnosis often oughts to be making people more open to suggestions for behavioral adjustments.
Hypnosis can help you acquire control over the habits you want to modify. It may improve your ability to cope with anxiety and discomfort. During hypnosis, you are more susceptible to suggestions, yet maintain control over your conduct.
FAQs
Can hypnosis cure anxiety?
This treatment includes picturing something that generates anxiety and reaching deep relaxation. Hypnosis promotes profound relaxation, which reduces tension and anxiety. This therapy involves imagining what causes
anxiety and then achieving a profound level of relaxation.
How does hypnosis actually work?
The mechanism behind this is not well known. Hypnosis has been linked to increased brain wave activity and the ability to accept new ideas. Others argue that it accesses the ‘unconscious mind’, which is more susceptible to fresh thoughts than the rational ‘conscious mind’.
Can hypnosis stop overthinking?
Hypnotherapy can relieve stress and concern, leading to less frequent and intense instances of overthinking. It provides practical strategies to minimize and eliminate ruminating, allowing individuals to reclaim control over their thought processes.
Can hypnosis stop depression?
A meta-analysis suggests that hypnosis may be equally beneficial for depression as other psychological therapies including cognitive behavioral therapy and interpersonal therapy.
Is hypnotherapy worth the money?
Hypnosis is a valid therapy that can assist with a variety of difficulties, such as quitting smoking, weight reduction, chronic pain, depression, and anxiety. It has been proven to be a useful supplement to Stanford Medicine. The study finds brain locations that change during hypnotic hypnosis.
References
- (2024b, May 1). Hypnosis. Cleveland Clinic.https://my.clevelandclinic.org/health/treatments/22676-hypnosis
- Wikipedia contributors. (2024b, October 8). Hypnotherapy. Wikipedia. https://en.wikipedia.org/wiki/Hypnotherapy
- Hypnosis – Mayo Clinic. (n.d.). https://www.mayoclinic.org/tests-procedures/hypnosis/about/pac-20394405
- (2023, November 21). Hypnotherapy: How to Benefit from Hypnosis Through Therapy. Verywell Verywell Mind. https://www.verywellmind.com/hypnotherapy-2671993
- (2019, April 1). Hypnotherapy. Healthline. https:/www.healthline.com/health/depression/hypnotherapy