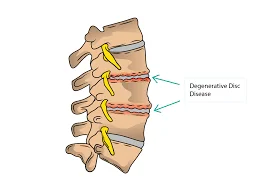
Cervical Degenerative Disc Disease: What is it?
Cervical Degenerative Disc Disease (CDDD) is a condition where the intervertebral discs in the neck (cervical spine) gradually deteriorate due to aging, wear and tear, or injury. This degeneration can lead to reduced disc height, loss of cushioning between vertebrae, and sometimes the formation of bone spurs.
Common symptoms include neck pain, stiffness, and, in some cases, radiating pain, numbness, or weakness in the shoulders, arms, or hands. Treatment typically involves a combination of physical therapy, pain management, and, in severe cases, surgical intervention.
Cervical degenerative disc disease, however, is often unknown to its sufferers. They might first learn about the illness at a normal checkup or when being evaluated for another medical issue. Asymptomatic disc disease is usually not an issue. The mere presence of abnormal X-ray data does not necessarily indicate that therapy is necessary.
Anatomy of the Cervical Spine:
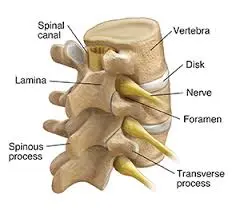
The cervical spine is an intricate and vital component of the skeletal system, situated in the neck. Its anatomy is broken down as follows:
Vertebrae
Structure:
The seven vertebrae that make up the cervical spine are designated C1 through C7.
A vertebral body, a vertebral arch, and many processes (spinous, transverse, and articular) are normally present in each vertebra.
Transverse foramina, or holes in the transverse processes that permit the vertebral arteries to flow through, are a crucial feature of cervical vertebrae.
Certain Vertebrae:
Atlas (This first cervical vertebra)
It has anterior and posterior arches but no vertebral body or spinous process.
It articulates with the skull’s occipital bone.
Axis (C2): The head can rotate thanks to this second cervical vertebra.
It includes the bony protuberance known as the dens (odontoid process), which extends upward and articulates with the atlas.
The lower cervical vertebrae (C3–C7) have articular facets, spinous processes, and vertebral bodies, making them more typical in structure.
Their uncinate processes, which aid in the formation of the uncovertebral joints, are one of their distinctive characteristics.
There is a noticeable and immediately perceptible spinous process on the C7 vertebra, sometimes referred to as the vertebra prominens.
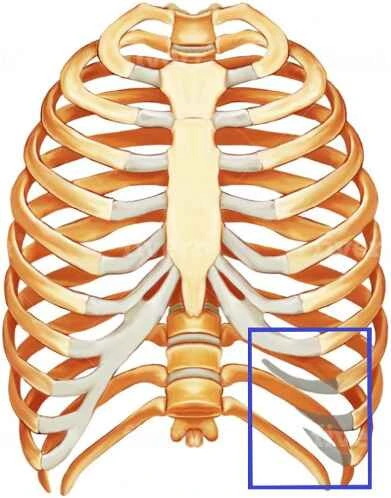
Intervertebral Discs:
These discs serve as shock absorbers and are situated in between the vertebral bodies.
They are made up of an inner gel-like core (nucleus pulposus) and an outside ring (annulus fibrosus).
Ligaments:
- The cervical spine is stabilized by several ligaments, including the anterior and posterior longitudinal ligaments.
- Flavum ligamentum.
- Ligament nuchal.
- Ligament transverse.
Joints:
- The atlanto-occipital joint, which permits nodding movements, is located between the occipital bone and the atlas.
- The atlantoaxial joint, which allows the head to rotate, is located between the axis and the atlas.
- Facet joints: These allow for gliding motions between the articular processes of neighboring vertebrae.
- Uncovertebral joints: Located between the lower cervical vertebrae’s uncinate processes, these joints are also known as the Luschka joints.
Blood vessels and nerves:
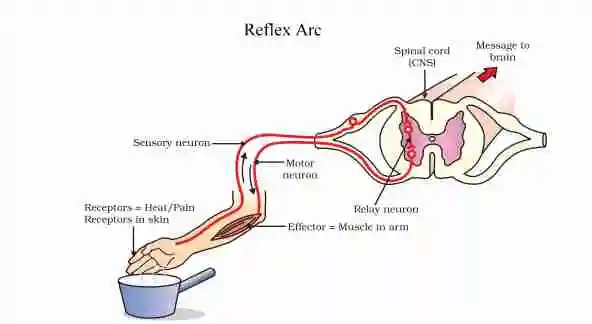
- The upper part of the spinal cord, which carries nerve impulses from the brain to the body, is housed in the cervical spine.
- Spinal nerves: Through intervertebral foramina, cervical spinal nerves leave the spinal cord.
- Vertebral arteries: These arteries feed blood to the brain by passing through the cervical vertebrae’s transverse foramina.
Causes of Cervical Degenerative Disc Disease:
Although aging naturally is the main cause of cervical degenerative disc disease, several variables can either cause it to develop or hasten its course. Below is a summary of the main reasons:
Naturally Aging :
- Disc Dehydration: As we age, the water content of the discs in our spine decreases, making them thinner and less pliable. They are less able to withstand shock as a result.
- Disc Weakening: Tiny rips or breaks in the disc’s outer layer (annulus fibrosus) can cause the disc to lose structural integrity.
Contributing Elements:
- Genetics: A hereditary tendency to earlier or more severe disc degeneration may exist in some people.
- Injury: Neck trauma, like whiplash or falls, can hasten the deterioration of the discs.
Lifestyle Elements:
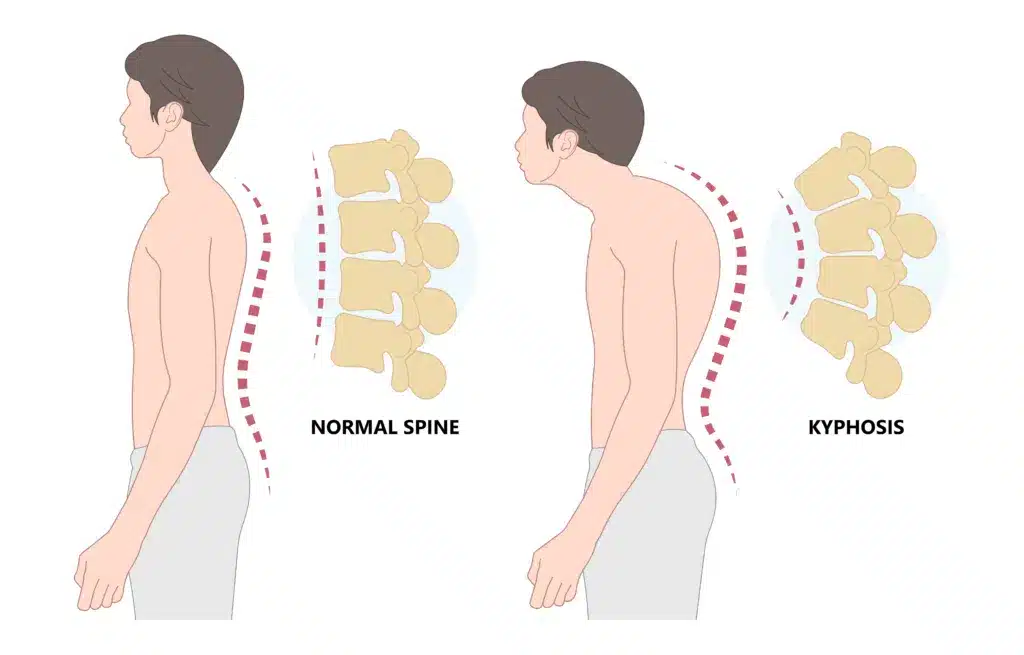
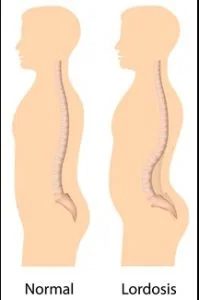
- Bad posture: Prolonged bad posture puts additional strain on the cervical spine, particularly as a result of the growing use of technological gadgets.
- Smoking: Smoking lowers blood flow to the discs, which makes it more difficult for them to absorb nutrients and causes dehydration.
- Obesity: Excessive weight puts stress on the spine.
- Repetitive Strain: Heavy lifting and repetitive neck motions are two jobs or activities that can raise the risk.
Signs and Symptoms of Cervical Degenerative Disc Disease:
The following are some typical traits of cervical DDD symptoms:
Pain in the neck. The most typical sign of cervical degenerative disc degeneration is a stiff neck with low-grade discomfort. But occasionally, the discomfort may also intensify and continue for a few hours or days.
Pain in the nerves. This kind of discomfort can travel down the shoulder into the arm, hand, and/or fingers and is typically acute or electric shock-like. Nerve pain usually only affects one side of the body.
Neurological symptoms affecting the fingers, hand, or arm. The arm, hand, and/or fingers may have pins-and-needles tingling, numbness, and/or weakness that travels down the shoulder. Daily tasks like typing, dressing, and handling objects may be hampered by these kinds of sensations.
Movement exacerbates the pain. In general, the movement seems to exacerbate degenerative disc pain, whereas rest tends to relieve it.
The discomfort will probably go away on its own in a few weeks or months if it is caused by the degenerative disc itself. In contrast, if facet joints in the neck also begin to degenerate and/or a spinal nerve becomes pinched, other symptoms of cervical degenerative disc disease are more likely to become chronic and need therapy.
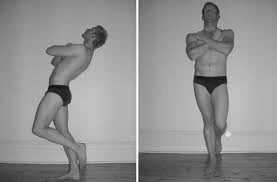
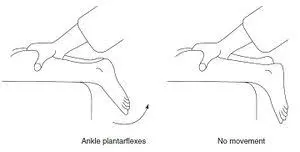
The spinal canal is more likely to constrict and endanger the spinal cord the more the cervical spine degenerates. Compression of the spinal cord may cause myelopathy, which manifests as symptoms like:
- Having trouble moving your arms or legs
- Issues with balance and/or coordination
- inability to control one’s bladder or bowels
- Anywhere weakness and/or numbness below the neck
- Aches in the arms or legs that resemble shock and are exacerbated by bending forward
Diagnosis of CDDD
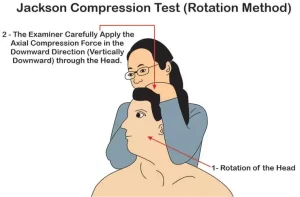
Accurate diagnosis is the foundation of all successful therapy. To guarantee an accurate diagnosis, your doctor will combine their experience with cutting-edge diagnostic tools. The diagnostic procedure consists of:
Medical background. Inquiries concerning your symptoms, their intensity, and previous therapies will be made by the doctor.
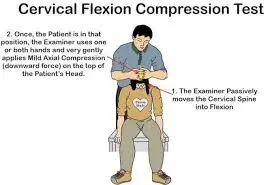
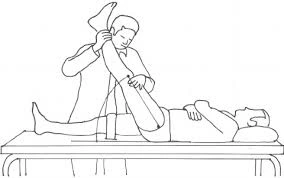
Physical assessment. You will get a thorough examination to check for discomfort, balance issues, and movement limits. The doctor will also check for neurological injuries during this examination, such as loss of reflexes, muscle weakness, or loss of sensation.
Diagnostic examinations. To rule out other issues like tumors and infections, most doctors begin with xX-rays We can also see whether the disc space between the vertebrae has decreased thanks to the films. To establish the diagnosis, we occasionally also employ a test known as a discography. To get a crisper image, contrast dye is injected into the damaged disc (or discs) during this examination.
Treatment of Cervical Degenerative Disc Disease:
Some steps can be taken to help decrease cervical degenerative disc disease symptoms and pain if they worsen. Self-care and/or non-surgical therapy alternatives are usually the first steps, and they will usually be beneficial in managing the pain.
Surgery may be considered in rare instances where spinal cord health is at risk or when pain and symptoms worsen or continue after several months of treatment.
Non-Surgical Treatment:
A physician will usually suggest one or a combination of the following treatments for neck discomfort caused by cervical degenerative disc disease:
Rest or change one’s way of life.
Certain activities, like craning the neck forward to look at the computer monitor or a particular swimming stroke, may cause greater neck pain than others. Usually, the discomfort can be lessened by avoiding or changing specific activities for a few days or weeks. Furthermore, it is advised to keep good posture (as opposed to slouching when sitting or extending the neck forward when driving, using a cell phone, etc.). Maintaining a nutritious diet, drinking plenty of water, and giving up smoking are also good for disc health.
Using medicine or injections to treat pain
Acetaminophen (found in Tylenol), ibuprofen (found in Advil and Motrin), and other over-the-counter pain medicines may be helpful. If not, a more potent painkiller, like muscle relaxants or oral steroids, might be recommended. An injection that administers medicine directly to a specific area of the neck, like a cervical facet injection or cervical epidural steroid injection, may be an additional alternative.
Heat and/or ice therapy
Applying a warm gel pack or an ice pack to the sore area of the neck helps some people feel less discomfort.
Exercise and/or physical therapy :
It’s crucial to realize that before beginning any new workout regimen, you should speak with a physician or physical therapist if you have cervical degenerative disc disease. They can offer tailored advice according to your particular situation. I can, however, offer some broad details regarding workouts that are frequently suggested for this ailment.
These exercises’ usual objectives are to:
- Enhance your posture: Good posture eases the load on your cervical spine.
- Build up your supporting muscles: Stability comes from having strong neck and upper back muscles.
- Boost flexibility: Mild stretches can alleviate stiffness and increase range of motion.
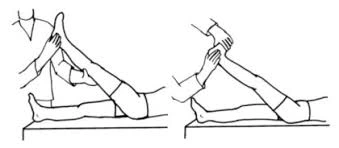
The following exercises are frequently suggested:
Chin Tucks:
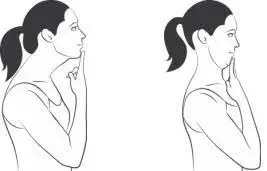
- This exercise enhances posture and strengthens the deep neck flexor muscles.
- Start by maintaining proper posture while standing or sitting.
- Pull your chin back straight and gently, like you’re doing a double chin.
- Repeat after holding for a few seconds.
Neck Retractions:
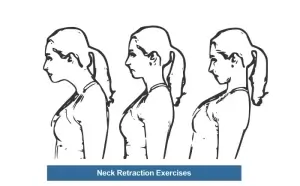
- This workout involves moving the head backward, much as chin tucks.
- With your chin tucked in, slowly slide your head back.
- This enhances the mobility of the cervical spine.
Isometric Neck Exercises:
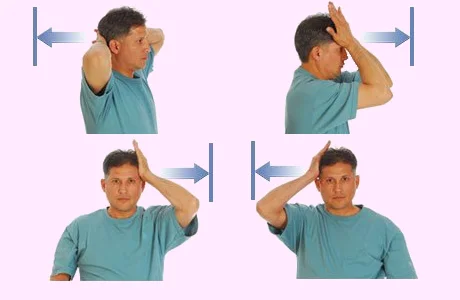
- In these workouts, your neck muscles are contracted without your head moving.
- For instance, you may put your palm on your forehead and use your neck muscles to resist as you gradually press on it.
- The muscles in the neck are strengthened as a result.
Shoulder Blade Squeezes:
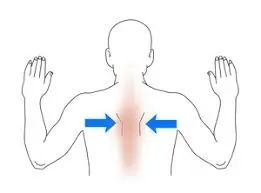
- This exercise eases neck tension and enhances posture in the upper back.
- Keep your arms by your sides while you sit or stand.
- Squeeze your shoulder blades together gently and hold the position for a few seconds.
Gentle Neck Stretches:
- These stretches aid in increasing the range of motion and decreasing rigidity.
- Aim your ear towards your shoulder while slowly cocking your head to the side.
- Repeat on the opposite side after holding for 15 to 30 seconds.
- Forward and backward flexions, as well as mild neck rotations.
Surgical procedures of Cervical Degenerative Disc Disease:
Your doctor may suggest surgery to relieve pain, weakness, and tingling if rest, medicine, and physical therapy are ineffective or if testing reveals compression of the nerve roots or spinal cord:
Cervical fusion. After replacing the damaged cervical disc with a spacer, the surgeon fuses the vertebrae on each side of the spacer.
Cervical disc replacement. Your motion is preserved when the surgeon replaces the damaged cervical disc with an artificial one.
FAQs
How is degenerative disc disease in the cervical region treated?
The most prevalent reason for patients to present is pain. Surgery may be necessary for pain or when it coexists with other neurological problems. Nonoperative methods, instrumented fusion, decompression, or a combination of instrumentation and/or laminoplasty are among the available treatment options.
When does cervical degeneration begin to occur?
By their 30s, many people exhibit cervical spine degeneration that can be shown on MRI images, and by the time they are 70, practically everyone has it.
Is it possible to treat degenerative disc disease?
No. Although the structural alterations associated with DDD will not go away, treatment may eventually alleviate the symptoms, such as back discomfort.
What signs of cervical disc disease are present?
Cervical disc disease is characterized by arm and neck pain that might spread to the hand. Numbness and tingling in the hand and arm may accompany this pain, giving the impression that they are “asleep.” Muscle weakness in the hands and arms may also occur.
Can someone with degenerative disc disease lead a normal life?
The majority of people who suffer from low back pain, sciatica, neck pain, or arm pain and tingling as a result of degenerative disc disease can effectively manage their pain and restore their lives without the need for surgery, even if there is no method to completely cure the problem.
Does degenerative disc disease benefit from walking?
Walking daily can help stop degenerative disc disease from getting worse. Walking can help develop the paraspinal muscles and prevent atrophy and excessive tension, whether it is done freely, on a treadmill, or with equipment. Walking regularly has been proven to lessen back pain.
References
- Facs, J. S. M. (n.d.). Cervical degenerative disc disease. Spine-health. https://www.spine-health.com/conditions/degenerative-disc-disease/cervical-degenerative-disc-disease
- Cervical disc disease, herniation, and degeneration – neurosurgery. (2025, January 7). Neurosurgery. https://med.virginia.edu/neurosurgery/services/spine-surgery/cervical-disc-disease-herniation-and-degeneration/
- Medtronic. (n.d.). Cervical systems – disc degeneration. Medtronic. https://www.medtronic.com/in-en/patients/conditions/cervical/disc-degeneration.html
- Cervical degenerative disc disease. (n.d.). https://www.spinesurgerydoctor.com/conditions/cervical-degenerative-disc-disease