Muscular Dystrophy
Muscular dystrophy is a set of hereditary illnesses characterized by progressive muscular weakening and deterioration. Muscular dystrophy is classified into over 30 varieties, each with its own set of symptoms, progression, and severity levels.
The most prevalent kind of muscular dystrophy is Duchenne muscular dystrophy (DMD), which mostly affects boys. The symptoms of muscular dystrophy worsen over time. It might be present at birth, develop during infancy, or develop in maturity, according to the type.
What is Muscular Dystrophy?
- Muscular dystrophies are a type of muscular illness caused by genetic abnormalities. Muscular dystrophy is a long-term disorder that causes muscular degeneration and weakness.
- This damage and weakening result from a shortage of dystrophin, a protein required for normal muscular function. A lack of this protein can cause difficulties in walking, swallowing, and muscular coordination, among other symptoms. It can also harm the muscles that assist your heart and lung function.
- The majority of diagnoses occur during childhood, although they can happen at any age. Others do not have symptoms until they are adolescents or middle-aged adults. The type of muscular dystrophy will determine how it affects you or your kid.
- Muscle weakness reduces mobility over time, making it difficult to complete daily chores. Muscular dystrophy comes in various forms, each affecting a particular section of the muscle, and its symptoms can vary in severity and appear at different ages. But not everyone experiences this.
- Other people can go for years with minor symptoms. There are over 30 types of muscular dystrophy, and each is unique based on:
- Genes that cause it
- The muscles it affects.
- The age at which symptoms first arise
- How fast the condition worsens.
- Muscular dystrophy can run in families, or a person may be the first in their family to get the condition. There may be multiple hereditary kinds within each form of muscular dystrophy, and persons with the same type of muscular dystrophy may exhibit distinct symptoms.
- Muscular dystrophies are uncommon, with limited information on how many people are affected. The Centers for Disease Control and Prevention (CDC) is attempting to estimate the number of persons suffering from each main kind of muscular dystrophy in the United States.
- Muscular dystrophies affect persons of both genders. However, the two most frequent types, Duchenne and Becker, are far more prevalent in men assigned at birth (MAAB).
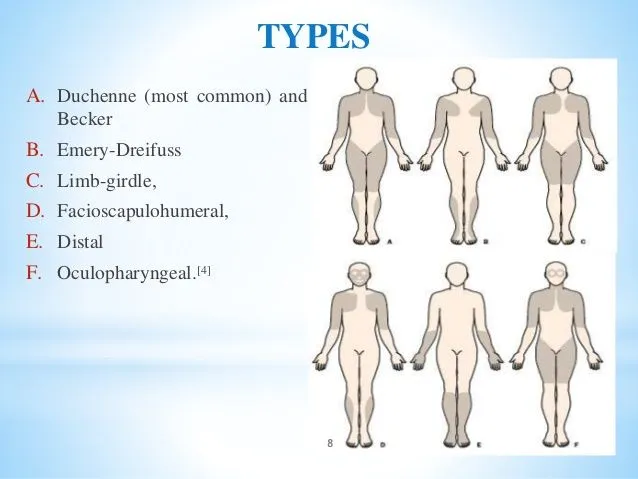
Types of Muscular Dystrophy
Muscular dystrophy types are categorized by the following:
- The degree and pattern of muscular weakening
- Age of starting
- Speed of development
- Level of Symptoms Severity
- Family background
There are about 30 different kinds of muscular dystrophy. Among the more widely used formats are:
Duchenne muscular dystrophy (DMD)
- This is the most frequent kind of muscular dystrophy. It primarily affects children assigned to males at birth (AMAB), although children assigned to females at birth (AFAB) may also experience a weaker form. DMD eventually damages your heart and lungs.
Becker’s muscular dystrophy (BMD)
- BMD is the second most prevalent kind of muscular dystrophy. It mostly affects persons with AMAB, however others with AFAB may experience lesser symptoms. BMD symptoms can emerge at any age between 5 and 60, however they usually appear during adolescence. BMD severity differs from person to person.
Myotonic dystrophy
- It is the most frequent kind of muscular dystrophy that affects adults. It has the same effect on adults who are AFAB and AMAB. People with myotonic dystrophy find it difficult to rest their muscles after utilizing them. The disorder can also harm your heart and lungs and create endocrine problems including thyroid disease and diabetes.
Congenital muscular dystrophy (CMD):
- CMD refers to a class of muscular dystrophies that appear at or around birth (“congenital” meaning “present from birth”). CMD produces muscular weakness and joint stiffness or looseness. Depending on the kind, CMD can also cause spinal curvature (scoliosis), respiratory problems, cerebral difficulties, cognitive challenges, vision problems, or seizures.
Distal muscular dystrophy:
- This condition affects the muscles in your hands, feet, lower arms, and legs. It often affects persons in their forties and sixties.
Emery-Dreifuss muscular dystrophy (EDMD):
- EDMD mostly affects children and young people AMAB. It often causes muscular weakness in the shoulders, upper arms, and shins. EDMD affects your heart as well. The illness often advances slowly.
Facioscapulohumeral muscular dystrophy (FSHD)
- FSHD mostly affects muscles in the face, shoulders, and upper arms. Symptoms usually begin before age 20. In the United States, around four out of every 100,000 persons have this type.
Limb-girdle muscular dystrophy (LGMD)
- LGMD affects the muscles of the upper arms, upper legs, shoulders, and hips. It affects individuals of all ages. In the United States, approximately two out of every 100,000 persons have LGMD.
Oculopharyngeal muscular dystrophy (OPMD)
- OPMD weakens the muscles in your eyes and throat. In your 40s or 50s, symptoms like drooping eyelids (ptosis) and trouble swallowing (dysphagia) frequently manifest. Approximately one in every 100,000 persons has OPMD.
While certain kinds manifest during early childhood or infancy, others might not show up until middle life or beyond. Skeletal muscle degeneration is a result of all forms, however incidence rates and severity are different.
The Effects of Muscular Dystrophy on Muscles
- Thousands of fibers make up an individual muscle. Every fiber is made up of cells enclosed in a membrane or outer layer. Connective tissue binds the different muscular fibers that make up each muscle.
- An impulse, or signal, travels from the brain to the neuromuscular junction—the area between a nerve fiber and the muscle it activates—through the spinal cord and peripheral nerves, which connect the central nervous system to the body’s sensory organs and muscles.
- There, acetylcholine, a neurotransmitter, sets off a chain of actions that results in the contraction of the muscle. The dystrophin-glycoprotein complex, a collection of proteins found in the muscle fiber membrane, guards against injury to the fibers during their contraction and relaxation.
- Muscle fibers start to absorb too much calcium and leak the protein creatine kinase when this protective membrane is compromised. Muscle degeneration progresses as a result of the injury and eventual death of the muscle fibers.
- Defects in this dystrophin-glycoprotein complex are responsible for certain types of MD. Some stem from imperfections in the adjacent connective tissue. Others are brought on by the muscle fiber’s production of harmful gene products.
- Damage to the integrity of muscle fibers is a sign of MD, although it can affect many bodily tissues and organs. This harm may result in:
- Degeneration of muscles
- Deterioration with time
- Phagocytosis, or the process by which scavenger cells break down and kill muscle fibers and fiber death
- Splitting and branching of fibers
- muscular tissue is replaced by fat and fibrous tissue
Causes of the Muscular Dystrophy
- Muscular dystrophy is caused by mutations (alterations) in the genes that control muscles’ proper form and function. Because of the mutations, the cells that would typically maintain your muscles cannot carry out this function, eventually resulting in gradual muscle weakness.
- Muscle function is influenced by multiple genes as well as potential genetic alterations. This causes a wide variety of muscular dystrophy types. The genetic mutation causing muscular dystrophy is inherited by the affected individual from one or both of their biological parents in most cases.
- Depending on the particular form, you can inherit muscular dystrophy in three different ways:
- Recessive inheritance: This indicates that both of your biological parents passed on the genetic mutation that causes the illness. This inheritance is present in certain cases of limb-girdle muscular dystrophy.
- Dominant inheritance: According to this theory, the illness can only arise if you receive the defective gene from one of your biological parents. This kind of inheritance is present in myotonic, facioscapulohumeral, and oculopharyngeal muscular dystrophies.
- Sex-linked (X-linked) inheritance: A genetically feminine person has two X chromosomes, and a genetically male person has one X and one Y chromosome. An X chromosome genetic mutation results in a sex-linked illness. Because genetically masculine individuals only have one copy of each gene on the X chromosome, a mutation in one of those genes will cause the disorder to manifest in them. X-linked illnesses can affect genetically feminine individuals as well, however, the symptoms are typically milder. This kind of inheritance is present in Becker and Duchenne muscular dystrophies.
Rarely, a person may develop muscular dystrophy on their own due to a chance mutation that wasn’t inherited. We refer to this as a de novo mutation.
Symptoms of the Muscular Dystrophy
Depending on the kind, muscular dystrophy symptoms might differ greatly. However, the primary symptom is weakness in the muscles and other problems relating to the muscles. Different bodily regions and muscles may be impacted by each type. Muscular dystrophy symptoms typically worsen over time.
Symptoms linked to movement and muscles may include:
- Atrophy of muscles.
- Difficulty running, walking, or climbing stairs.
- Abnormal gait when walking, such as waddling or toe walking.
- Joints that are lax or stiff.
- Your skin, tendons, and muscles will all become permanently tight (contractures).
- Velocities.Aches in the muscles.
- Fatigue is another symptom that may exist.
- Difficulty swallowing, or dysphagia.
- Cardiac issues, including arrhythmia and cardiomyopathy (heart failure).
- Scoliosis is a curvy spine.
- Breathing issues.
- Impairments of the intelligence.
- learning Difficulty.
Diagnosis of Muscular Dystrophy
- Doctors examine an individual’s medical and family history to see if the muscular symptoms are caused by an illness that mostly affects other tissues or organs and whether they may detect a hereditary problem. The medical team will also do tests to rule out muscular weakness caused by previous surgery, toxins, or present drugs.
- Thorough clinical and neurological examinations can assist doctors in the following:
- Exclude diseases of the central and/or peripheral nervous systems.
- Identify patterns of muscular weakening and atrophy.
- Test reflex reflexes and coordination.
- Check for contractions.
- Laboratory testing, such as blood and urine, can confirm the diagnosis of MD.
- Exercise testing can identify increased levels of particular substances during or after exercise. Genetic testing and counseling.
- Genetic analysis is the standard way for diagnosing and characterizing MD. Clinical studies often need a genetic diagnosis.
- Amniocentesis is a procedure performed during pregnancy to examine a sample of amniotic fluid in the womb.
- Chorionic villus sampling (CVS) is a technique used to analyze a tiny sample of the placenta during early pregnancy.
- Magnetic resonance imaging (MRI), phosphorous magnetic resonance spectroscopy, and sonography are used to assess muscle quality, atrophy, and other problems.
- Muscle biopsies are performed to assess disease progression and therapy efficacy.
- Immunofluorescence testing detects particular proteins inside muscle fibers.
- Electron microscopy is used to detect changes in subcellular components of muscle fibers. Electron microscopy can also detect alterations that indicate cell death, mutations in muscle cell mitochondria, and an increase in connective tissue.
- Neurophysiology examines physical and/or chemical changes in the neurological system.
- Nerve conduction velocity (NCV) is a measure of the speed and strength with which an electrical signal travels along the nerve. This can help assess whether nerve damage exists.
- Repetitive stimulation tests the function of the neuromuscular junction by electrically stimulating a motor neuron numerous times in succession.
- Electromyography (EMG) is used to monitor muscle fiber and motor unit activity. The results may indicate electrical activity associated with MD or other neuromuscular illnesses.
Differential Diagnosis of Muscular Dystrophy
There are several heritable illnesses affecting muscles, nerves, and the neuromuscular junction. Diseases such as inflammatory myopathy, progressive muscular weakness, and cardiomyopathy (heart muscle weakening that interferes with pumping function) can create symptoms similar to those present in some kinds of MD, although they are caused by distinct genetic flaws. The following disorders exhibit symptoms comparable to MD:
- Birth defects in myopathy
- Atrophy of the spinal muscles
- Syndromes of congenital myasthenics
Muscular dystrophy can be challenging to identify right away due to these overlapping symptoms and the prevalence of MD with no known hereditary etiology (sporadic MD). Some people may exhibit MD symptoms and signs even when they do not possess any of the known hereditary abnormalities.
Risk Factors of Muscle Dystrophy
- Genetics: It is the main risk factor for muscular dystrophy (MD). The majority of MD cases are hereditary, which means that genetic mutations inherited from parents cause the disease in offspring. These mutations may impact many proteins necessary for the structure and function of muscles.
Although heredity is the primary risk factor for MD, a few additional variables may also affect the condition’s severity or chance of complications:
- Sex: Men are more likely than women to have certain kinds of MD, such as DMD.
- Age of onset: Depending on the kind of MD and the particular mutations involved, there might be a range in the age at which symptoms first appear.
- Environmental factors: For some patients, exposure to certain chemicals or viruses can exacerbate the symptoms of multiple sclerosis.
Complications of Muscle Dystrophy
Muscular dystrophy evolves differently for each individual. Complications differ according to the kind of muscular dystrophy. Some of the most prevalent problems include: Movement, respiration, heartbeat, and spine
Mobility changes
- Progressive muscular weakening might eventually restrict movement. Many persons with muscular dystrophy will eventually require assistance equipment and gadgets, such as wheelchairs. Specially built wheelchairs can enhance comfort, perhaps reduce discomfort, and offer appropriate muscular support.
Respiratory problems
- Muscular dystrophy can create respiratory issues because muscular weakening makes breathing difficult. Trouble swallowing can result in aspiration or the accumulation of material in the airway or lungs. Overall, the respiratory system works harder to get oxygen into the body and eliminate carbon dioxide.
Cardiac issues
- Dystrophin deficiency can also affect the heart, which is a muscle. People with muscular dystrophy frequently develop cardiomyopathy or heart muscle illness. Doctors may offer heart medication as part of continuous muscular dystrophy treatment.
Contractures and Scoliosis
- Muscular dystrophy can also impair the skeletal muscles, which provide flexibility in the tendons and joints. As a result, tendons and joints are pulled into a flexed posture, which may become permanent. This is known as a contracture.
- Scoliosis, or spine curvature, can be caused by spinal muscular weakness.
Some contractures can be treated with surgery. Corticosteroids and physical therapy may assist in preventing the development of scoliosis.
Pregnancy Considerations
- People with muscular dystrophy who become pregnant are more likely to experience problems during gestation and labor. Muscle weakness in the knees, hips, and abdomen, for example, might make it difficult to push during labor, increasing the likelihood of a cesarean birth or other interventions.
- Myotonic dystrophy might cause pregnancy loss due to its generalized muscular weakness. Pregnancy can potentially cause myotonic dystrophy to progress faster and aggravate symptoms.
Treatment of Muscle Dystrophy
There is currently no cure for muscular dystrophy, however, treatments can help control symptoms and reduce the disease’s course. Treatments vary according to your symptoms and the type of muscular dystrophy you have. For example, while many different mutations can lead to both BMD and DMD, certain developing treatments for DMD may not be effective for BMD, and other types.
Available therapies try to keep patients as independent as possible while also reducing consequences caused by muscular weakness, restricted mobility, and heart and breathing problems. Physical therapy, medication therapy, and surgery may all be used together to treat the condition.
Medication
- Drug treatment may be used to slow muscle deterioration in muscular dystrophies. The Food and Drug Administration Food and Drug Administration (FDA) has authorized various medications to treat DMD (given orally or by injection).
- Steroids, such as prednisone and deflazacort, as well as immunosuppressive medicines, can help reduce muscle degeneration and damage to muscle cells. Still, some have side effects that are especially concerning in youngsters. MD symptoms, such as myotonia, can potentially be treated with medications. Antibiotics can help with breathing difficulties.
The new treatment options include:
- Eteplirsen (Exondys 51): This weekly injection is for those who have a particular dystrophin gene mutation that allows for exon 51 skipping. According to the FDA’s 2016 approval notification, this affects around 13% of persons with DMD.
- Golodirsen (Vyondys 53): This weekly injection is for those who have a dystrophin gene difference that allows for exon 53 skipping. This pertains to around 8% of persons with DMD, according to the FDA’s 2019 approval notification.
- Viltolarsen (Viltepso): This is a weekly injection for patients with a dystrophin gene difference that allows for exon 53 skipping. The FDA authorized Viltolarsen (Viltepso) in 2020.
- Casimersen (Amondys 45): This weekly injection is intended for those who have a gene difference that allows them to bypass exon 45. This pertains to around 8% of persons with DMD, according to the FDA’s 2021 approval application.
- Deflazacort (Emflaza): This corticosteroid comes in tablet and oral suspension form. It is authorized for DMD patients aged 5 and above.
Gene therapy
- Elevidys, the first gene therapy medicine for children aged 4-5 with specific kinds of DMD, was authorized by the FDA in 2023. It is provided as a single injection and induces the body to produce a shorter form of the dystrophin protein.
- Additional research is being conducted to find a viable cure for DMD. In 2018, scientists discovered a mechanism to fix a gene in canine animals, resulting in enough dystrophin production.
- They aim to one day use this powerful gene editing technology for persons with DMD. Other research is being conducted on gene therapy for muscular dystrophy.
Muscles Therapy
- Muscle treatment has proved to be helpful. These strategies require consulting with a specialist to enhance physical performance.
- Physical therapy: It can help people increase their mobility and maintain their muscles as flexible and strong as possible. Passive stretching can also help improve joint flexibility and avoid contractures. It involves exercise and stretching to maintain muscular strength and flexibility.
- Deep breathing and coughing exercises can benefit persons with MD who have difficulty breathing. respiratory treatment is used to prevent or postpone breathing difficulties.
Assistive devices
- Wheelchairs, splints, braces, spinal supports, and posture correction devices can assist patients with MD retain their mobility by compensating for muscular weakness. Assisted ventilation is frequently required to address respiratory muscle weakening that occurs with many kinds of MD, particularly in the late stages.
Dietary supplement:
- There is no evidence that dietary supplements, certain foods, or diets can stop the course of MD. People with MD should eat healthily to maintain their general health. People with MD who have difficulty swallowing may require specialized feeding approaches.
Occupational therapy
Which focuses on daily tasks, that can benefit people with muscular dystrophy:
- Become less dependent
- on gaining access to community services.
- Improve coping abilities.
- Improve social skills.
Speaking therapy, to preserve muscular strength by particular strategies such as slower talking, stopping between breaths, and utilizing special equipment.
Surgical Treatment
Corrective surgery can help with MD issues, such as
- Heart issues.
- Muscular shortening.
- To treat eye Problems
- To treat Scoliosis
Tendon or muscle release surgery for contractures, pacemakers for cardiac difficulties, scoliosis-related discomfort or postural imbalance surgery, and cataract surgery for sight problems.
Physical therapy for Muscle Dystrophy
An essential component of treating muscular dystrophy (MD) is physical therapy. While there is no treatment for MD, physical therapy can benefit those with it. Keep their mobility, strength, and independence for as many years as possible.
These are some of the primary aims of physical therapy for muscle dystrophy.
- Maintain and enhance your range of motion (ROM). Stretching exercises are an essential component of physical therapy for muscle dystrophy. They aid in avoiding contractures, which are muscular shortenings that can restrict joint movement.
- Maintain and develop muscular strength: Strengthening exercises can assist in delaying the growth of muscle weakening and improve functional capabilities.
- Improve balance and coordination: Balance and coordination issues are typical in MD. Physical treatment can assist in strengthening these abilities and lessen the likelihood of falling.
- Maintain and improve posture: Poor posture can cause discomfort and other issues. Physical therapy can help you improve your posture and avoid these difficulties.
- Reduce discomfort: Physical therapy can assist in alleviating the pain produced by muscular weakness and contractures.
- Improve general health and well-being: People with MD benefit from regular physical exercise.
Physical therapy for muscle dystrophy is often tailored to the patient’s unique requirements and skills. A physical therapist will collaborate with the patient to create a safe and effective treatment plan.
A physical therapist may utilize the following sorts of therapies for MD:
- Stretching: Stretching improves the range of motion and prevents contractures.
- Strengthening exercises can help you maintain and develop your muscular strength.
- Aerobic exercise can benefit cardiovascular health and general fitness.
- Balance and coordination exercises can assist enhance these skills and lower the chance of falling.
Here are some other things to consider regarding physical therapy for MD:
- Beginning physical therapy early and maintaining it throughout your life is critical.
- Physical therapy should be part of a multifaceted treatment strategy that may involve medication, surgery, and other therapies.
- Physical therapy can be safe and helpful for MD patients of all ages and abilities.
Prevention for Muscle Dystrophy
There is currently no way to avoid muscular dystrophy because it is a hereditary disorder. If you are concerned about the potential of passing on muscular dystrophy or other genetic problems before attempting to have a biological child, speak with your doctor about genetic counseling.
In certain cases, prenatal testing may be able to detect the issue early in pregnancy. If you have muscular dystrophy, you can take the following actions to attempt to avoid or postpone consequences and enhance your quality of life:
- Eat a nutritious diet to avoid malnutrition.
- To avoid constipation and dehydration, drink a lot of water.
- Exercise as much as your healthcare team recommends.
- Maintain a healthy body weight.
- Quit smoking now to protect your lungs and heart.
- Stay up to speed on vaccinations.
The illness is likely to have a significant impact on your family. Remember that it is OK to seek help from a doctor, counselor, family member, or friend if you are experiencing stress, depression, or rage.
Support groups are also an excellent opportunity to meet other individuals who have lived with muscular dystrophy. They may assist your kid in connecting with people who share their interests, as well as provide you and your family with guidance and support.
What are the most recent updates on muscular dystrophy?
- The NIH sponsors a wide spectrum of scientific, translational, and clinical research on MD. While certain genes responsible for muscular dystrophy have yet to be found, breakthroughs in gene sequencing have assisted in the discovery of genes that may be implicated in the majority of muscular dystrophy cases.
- A new understanding of individual disease pathways is revealing prospective targets for therapeutic development in practically all kinds of MD. For example, breakthroughs in targeted treatment have resulted in encouraging results in myotonic dystrophy and facioscapulohumeral muscular dystrophy.
NINDS, which is part of the National Institutes of Health, is the primary funder of MD research at the NIH and grantee organizations around the world.
Summary
Muscular dystrophy refers to a set of over 30 hereditary diseases that result in muscular weakening and other muscle-related symptoms. Understanding your muscular dystrophy diagnosis might be stressful.
Your healthcare team will provide a comprehensive management strategy tailored to your symptoms. It’s critical to ensure you’re getting the help you need and to pay attention to your health. Understand that your healthcare staff will be there to help you and your family.
FAQs
What is the prognosis of muscular dystrophy?
The prognosis (outlook) for muscular dystrophy varies according to the kind. Your healthcare professional will be able to give you a clearer sense of what to expect depending on your kind of muscular dystrophy and your circumstances.
What is the life expectancy for people with muscular dystrophy?
The life expectancy for muscular dystrophy varies greatly according to the kind.
For example, patients with Duchenne muscular dystrophy (DMD) frequently die before the age of 25. Other types of muscular dystrophy, such as oculopharyngeal muscular dystrophy, seldom influence life expectancy.
What might cause muscular dystrophy?
Muscular dystrophy is a hereditary disorder. A family history of muscular dystrophy increases the likelihood of becoming a carrier or getting the condition.
DMD and BMD are connected to the X chromosomes, therefore children assigned male are significantly more prone to develop them.
Even though female offspring get an X chromosome from each parent and should produce enough dystrophin, they may nevertheless develop DMD or BMD symptoms such as muscular cramping, weakness, and heart problems.
What is the life expectancy for people with muscular dystrophy?
The life expectancy of someone with muscular dystrophy varies depending on the kind. People with BMD, for example, often live for 40-50 years, but those with EDMD may survive into their middle years.
Can you completely recover from muscular dystrophy?
There is presently no known cure for any of the muscular dystrophies, however treatments and therapies do exist.
What is the earliest age for muscular dystrophy?
Congenital muscular dystrophy normally develops from birth.
Is there a treatment for muscular dystrophy?
Treatments may include steroid medications to maintain muscle strength for as long as possible; stretching and other exercises specifically designed for people with muscular dystrophy; braces and splints; assistive devices such as lifting equipment, computer technologies, and wheelchairs to assist those suffering from DBMD.
References
- Muscular dystrophy – Symptoms & causes – Mayo Clinic. (2022, February 11). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/symptoms-causes/syc-20375388
- Professional, C. C. M. (n.d.-j). Muscular dystrophy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14128-muscular-dystrophy
- What is Muscular Dystrophy? | CDC. (2022, November 21). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/musculardystrophy/facts.html
- Muscular dystrophy. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/muscular-dystrophy
- Martel, J. (2023, October 5). What you need to know about muscular dystrophy. Healthline. https://www.healthline.com/health/muscular-dystrophy#fa-qs
- Watson, S. (2014b, September 20). Muscular dystrophy. WebMD. https://www.webmd.com/children/what-is-muscular-dystrophy





7 Comments