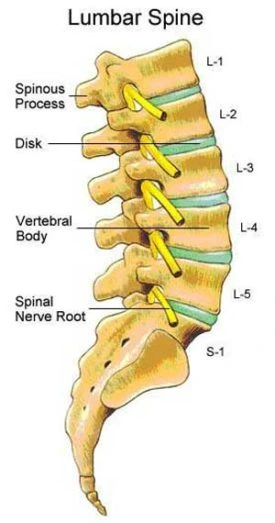
Lumbar Spine
Lumbar Spine Anatomy
The lower end of the spinal column between the first sacral vertebra (S1) and the last thoracic vertebra (T12) is known as the lumbar spine. The five robust and movable vertebrae (L1–L5) that provide the dispersion of axial stresses shield the spinal cord in this area.
At the level of the L1 and L2 vertebrae, the spinal cord ends in the conus medullaris, which passes through the middle of the vertebral column. The bundle of spinal nerve roots known as the cauda equina, or horse’s tail in Latin, starts at the spinal cord’s termination and descends along the remaining portion of the canal.
Bone, cartilage, ligaments, nerves, and muscles make up the lumbar spine. Every one of these elements is essential to the shape and functionality of the lumbar spine.
Structure and Function
The lumbar spine serves three primary purposes. To begin with, the lumbar spine helps to sustain the upper body. Because they are larger than other spinal column sections, the lumbar vertebrae (L1–L5) can absorb axial pressures from the head, neck, and trunk.
The spinal cord and spinal nerves are shielded by the canal formed by the lumbar vertebrae. Information can go from the central nervous system to the lower extremities and vice versa thanks to this configuration.
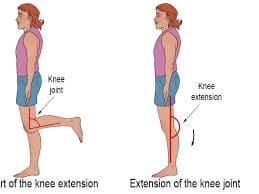
Many truncal motions, such as flexion, extension, rotation, and side bending, are possible with the lumbar spine. The term “lumbar lordosis” refers to the concave curvature of the lumbar spine as viewed from the side. This varying degree of curvature distributes the weight of the upper body over the pelvis to facilitate effective bipedal movement.
Every lumbar vertebra is made up of several parts. These consist of the posterior elements, which are dorsal structures, and the vertebral body. Two pedicles that adhere to the laminae are located immediately dorsal to the vertebral body. Forces from the posterior elements are transmitted to the vertebral body through the pedicles, which also oppose motion. In posterior direction, the spinous process extends from the junction of the two laminae.
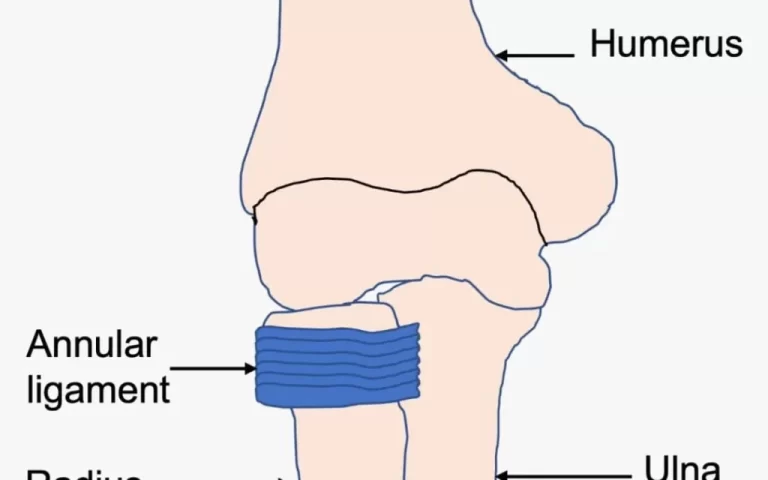
Four articular processes and two transverse processes are located where the pedicles and laminae meet. Ligaments and muscles can attach to the transverse processes, which extend laterally. The zygapophyseal joints, also known as the facet joints, are produced by the superior and inferior articular processes. The superior articular process and inferior articular process of a vertebra meet at this joint, which is located immediately cephalad.
These sagittal plane joints help move the lumbar spine in both flexion and extension. Stress fractures, also known as spondylolysis, can occur in the pars interarticularis, which is the lamina between the superior and inferior articular processes in the growing spine.
A fibrocartilaginous structure situated between two vertebral body endplates is the lumbar disc. It is made up of an external fibrous annulus fibrosus and an internal gelatinous nucleus pulposus. Shock absorption is the lumbar disc’s main purpose. The vertebral body is positioned anteriorly and posteriorly by two longitudinal ligaments. The lumbar region cannot be extended, translated, or rotated because of the anterior longitudinal ligament.
The lumbar flexion is inhibited by the posterior longitudinal ligament. The ligamentum flavum, one of the segmental ligaments, is pierced during a lumbar puncture. The remaining segmental ligaments include the supraspinous and interspinous ligaments, which lie between the spinous processes and oppose lumbar flexion.
Embryology
Around the third week of pregnancy, the lumbar spine starts to grow. This process is started by the notochord, which secretes growth hormones that encourage the ectoderm to change into a neuroectoderm. The neural tube, which eventually gives rise to the spinal cord, is created during the process of neurulation. A variety of congenital abnormalities, from moderate (spina bifida) to severe (anencephaly), can be caused by errors made during neurulation.
Additionally, the paraxial mesoderm divides into pairs of somites on either side of the neural tube by the end of the third week. A dermomyotome and a sclerotome develop from each somite. The sclerotome divides into cranial and caudal cell clusters. Neural tube neurons enter these clusters and innervate particular dermatomes and myotomes. The cranially placed clusters of the adjacent sclerotome fuse with the caudally located cell clusters to form the vertebral body. The intervertebral disc forms in between each cluster of cells. The vertebral arch is formed when sclerotome cells travel around the neural tube and fuse dorsally at the same time.
Endochondral ossification is the process by which mesenchymal cells develop into cartilage and ultimately bone in each vertebra. Around week six, chondrification centers begin to form, followed by primary ossification centers in week seven. The ultimate vertebra is strengthened as a result of these processes. Bone remodeling is a lifelong process that is heavily influenced by mechanical loads and stress.
Blood Supply
Three major longitudinal arteries provide the spinal cord with an abundant blood supply. The anterior two-thirds of the cord is supplied by a single anterior spinal artery. The posterior one-third of the cord is supplied by two posterior spinal arteries on the dorsal side. A number of radicular arteries, both anterior and posterior, feed the vertebral column with collateral blood flow. The ventral and dorsal nerve roots are supplied with blood by these radicular arteries as they pass across them. The greatest radiculomedullary artery, the artery of Adamkiewicz, supplies blood to the lumbar spinal cord.
The artery branches from a posterior intercostal or radicular artery and has a varied origin between T8 and L2. It usually ascends the spinal canal, making a hairpin loop before joining the anterior spinal artery, to the left of the spinal cord.
Four pairs of lumbar arteries, unique to the lumbar spine, emerge from the abdominal aorta. To supply each vertebra, these paired arteries move posteriorly along the vertebral bodies. The transversus abdominis and internal oblique muscles, two nearby musculatures, are likewise supplied with blood by these arteries.
Lymphatic Drainage
Lymph from the pelvis and lower limbs is drained by a vast network of lymphatics in the lumbar area. The aorta and inferior vena cava both have these lymph nodes. The lymph is transported to the thoracic trunk by the lumbar lymph nodes, which receive outflow from the common iliac nodes.
Nerves of Lumbar Spine
After leaving the neural foramen, the spinal nerves split into ventral and dorsal rami. Five pairs of mixed spinal nerves, carrying both motor and sensory nerve fibers, emerge from either side of the lumbar spinal cord. The dorsal rami provides sensation to the skin of the back and motor innervation to the erector spinae musculature. To the remaining prevertebral musculature and lower limbs, the ventral rami supply motor and sensory fibers.
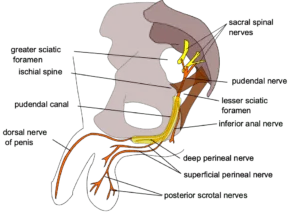
The lumbar plexus is a network of nerves made up of the ventral rami T12 to L4. The obturator (L2-L4) and femoral (L2-L4) nerves, respectively, originate from the lumbar plexus. The genitofemoral (L1-L2), iliohypogastric (T12-L1), ilioinguinal (L1), and lateral femoral cutaneous nerve of the thigh (L2-L3) are the remaining lumbar plexus nerves. The lumbosacral plexus forms from the L4 to S4 ventral rami. The lumbosacral trunk, which descends into the pelvis to reach the sacral plexus, is formed by the union of the L4 and L5 roots.
The sciatic nerve (L4-S3), which splits into the common peroneal and tibial nerves, is derived from the lumbosacral plexus. The posterior femoral cutaneous of the thigh (S1-S3), the pudendal nerve (S1-S4), the superior gluteal (L4-S1), and the inferior gluteal (L5-S2) are also parts of the sacral plexus.
The L4 nerve, for example, leaves the body below the L4 vertebra via the L4-L5 neural foramen. Each lumbar spinal nerve terminates below the appropriate vertebra. The majority of lumbar disc herniations do not compress the nerve root that exits at the disc level; instead, they occur centrally.
One level below the herniated disc is where the nerve root that is most frequently impacted escapes. As an illustration, an L4-L5 central disc herniation will often compress the L5 nerve root in the spinal canal’s lateral recess. Though less frequently, the L4 nerve root is crushed in the context of a far lateral disc herniation. This discrepancy results from the traversing spinal neurons’ more center location as opposed to the departing spinal nerves’ more lateral position.
Afferent sensory fibers are supplied to a specific skin area by each spinal neuron. We call this region of skin a dermatome. Every lumbar spinal neuron also contains motor fibers that innervate a myotome, which is a collection of muscles. Our embryonic development can be linked to both dermatomes and myotomes. Because they can be utilized to identify the lumbar spinal nerve(s) involved in the setting of disease, dermatomes and myotomes are therapeutically useful.
The important muscular and sensory innervations of the lumbar spinal nerves will be covered in this section. The iliopsoas muscle, the inguinal crease, and the medial thigh receive sensory innervation from L1 and L2. The muscles of the adductors, iliopsoas, and quadriceps are partially innervated by L3. Anterior-medial thigh sensory innervation is supplied by L3. L4 innervates the tibialis anterior, adductors, quadriceps, and iliopsoas in addition to contributing to the femoral and sciatic nerves. The anterior thigh and medial lower leg are innervated sensory regions by the L4 nerve. The patellar reflex arc is influenced by the L3 and L4 nerves.
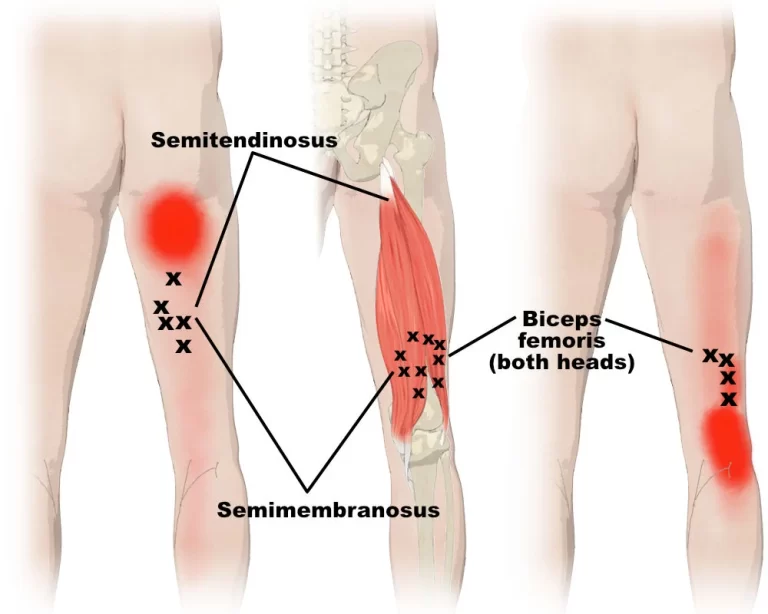
The gluteus medius, flexor digitorum longus, tibialis anterior, extensor hallucis longus, extensor digitorum longus/brevis, peroneus longus, tibialis posterior, and medial hamstrings are all innervated by the L5 nerve. The dorsum of the foot and the lateral leg receive sensory innervation from L5. The fact that each dermatome overlaps with neighboring dermatomes is significant from a clinical standpoint.
Consequently, in the presence of nerve root compression, thick numbness is incredibly uncommon. Because each myotome overlaps, two or three lumbar spinal nerves innervate almost all of the lower extremity’s muscles.
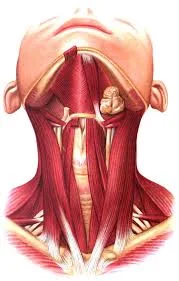
Muscles related to Lumbar Spine
The lumbar vertebrae serve as attachment points for numerous muscles. These muscles enable regulated, fluid movement in several functional planes. In addition, these muscles have a supporting function in proprioception, protection, and stability. To facilitate mobility, three main muscle groups attach to or arise from the lumbar spine. Initially, the multifidi and erector spinae make form the extensor group. This group is situated behind the lumbar region. The erector spinae muscles in this area comprise the iliocostalis lumborum and longissimus thoracis. This group contracts, causing the lumbar spine to experience an extension moment.
Trunk and hip flexion are made possible by the flexor group, which is located anterior to the lumbar spine. The iliacus in the thigh is joined by the psoas major, which comes from the T12-L4 transverse processes, to form the iliopsoas (composite muscle). The iliopsoas is an important muscle that helps arch the lumbar spine and facilitates hip flexion. Truncal flexion is primarily controlled by the abdominal muscles (rectus abdominis, internal/external oblique). Lastly, to produce rotation and lateral flexion (side bending) of the lumbar spine, a coordinated effort involving multiple muscles is needed. These motions are mostly produced by the multifidi, psoas major, abdominal musculature, and quadratus lumborum.
The most common cause of lumbar strains in muscles is aberrant stress on a tendon, which can be brought on by overstretching a muscle, overusing a muscle, or tearing a muscle with too much effort. The majority of lumbar muscle strains will improve with conservative care.
Surgical Importance
When conservative measures fail to relieve low back pain, lumbar radiculopathy, and lumbar spinal stenosis, spine surgery may be considered. When it comes to more serious and urgent disorders including conus medullaris syndrome, cauda equina syndrome, primary or metastatic malignancy, osteomyelitis/discitis, epidural abscess, and trauma, spinal surgery is the first line of therapy. The patient’s characteristics and the diagnosis that needs to be treated determine the surgical approach and equipment used.
A procedure called lumbar decompression is used to treat pain brought on by a compressed nerve root or nerves. As we will discuss in the next section, lumbar radiculopathy, and lumbar central canal stenosis are two of the most prevalent forms of nerve root compression. There are various methods of lumbar decompression, such as laminotomy, microdiscectomy, foraminotomy, laminectomy, or a combination of these. The most common surgical procedure for treating lumbar spinal stenosis is a laminectomy, or the surgical removal of the laminae. In the event that the aforementioned decompression causes iatrogenic instability, a fusion is also carried out.
A frequent surgical procedure for treating radiculopathy, discogenic/facetogenic low back pain, and spinal deformity (scoliosis/spondylolisthesis) is lumbar fusion. There are two primary groups of surgical techniques: interbody fusion and posterior techniques. The more conventional method uses rods and pedicular screws in a posterior spinal fusion. This method’s drawbacks include the requirement for retraction of the nerve roots and thecal sac, as well as iatrogenic damage to the paraspinal muscles. After a discectomy, an implant, such as a cage or bone graft, is placed within the intervertebral space (removing the intervertebral disc). This procedure is known as interbody fusion.
There are several different surgical techniques for interbody fusion (posterior, transforaminal, oblique, lateral, and anterior). Although the canal and nerve roots are avoided, problems including vascular damage and incisional hernia are still present with anterior spinal fusion. Comparative evidence supporting the superiority of one strategy over another is few. Chronic postoperative problems after fusion include neighboring segment degenerative disc degeneration above/below the fusion level and pseudoarthrosis, or failure of fusion.
Physical therapy and/or manipulation therapy are examples of non-surgical treatment. The degree of the injury, patient compliance, and symptom severity will all play a role in the choice of whether or not to use these procedures.
Clinical Importance
Estimates of the indirect costs of non-specific low back pain in the US range from 18.5 to 28.2 billion dollars, making it one of the major causes of illness burden worldwide. Both physical (such as improper lifting technique) and psychosocial factors can cause low back pain. Frequently, a precise trigger remains unidentified.
Numerous distinct disease processes can present with low back pain as a symptom. To rule out certain illnesses that would need an urgent or emergent workup and therapy, triage is required. Trauma, age more than 70, inexplicable weight loss, a history of cancer, constitutional symptoms, nocturnal pain, saddle anesthesia, and impaired bladder or bowel function are all considered “red flags” for the lumbar spine. Red flags include conus medullaris/cauda equina syndrome, infection (osteomyelitis/discitis), malignancy, and spinal fracture (discussed below).
The conus medullaris, the name for the spinal cord’s terminal, is located between the L1 and L2 vertebrae. This structure is important from a clinical standpoint for procedures in this field, particularly lumbar punctures. A lumbar puncture, often known as a spinal tap, is a procedure used to obtain a sample of cerebrospinal fluid by passing a needle between the vertebral lamina.
To avoid the spinal cord, this treatment must take place between the L4-L5 or L3-L4 laminae, below the level of L2. Severe compression or damage to the conus medullaris causes conus medullaris syndrome. The most frequent causes of this illness are epidural abscesses, disc herniations, and trauma.
Severe or abruptly developing low back pain, symmetrical weakness in both legs and abrupt loss of bladder and bowel function are signs and symptoms of conus medullaris syndrome. In order to maintain lower extremity neurologic function and avoid irreversible injury, immediate therapy is required. The cauda equina is located in the spinal canal caudal to the conus medullaris.
A group of spinal nerves from L1 to L5 in the spinal canal make up the cauda equina. The L2-L5, S1-S5, and coccygeal nerves are the spinal nerves that make up the cauda equina. A surgical emergency also arises when the cauda equina is compressed. Urinary retention, saddle anesthesia (numbness of the inner thighs/peritoneum), and radicular leg discomfort are the most prevalent signs and symptoms.
There exist multiple conceivable pathoanatomical conditions affecting the lumbar spine. Potential sources of discomfort include the facet joints, spinal nerves, intervertebral discs, and surrounding muscles. Nonetheless, the majority of low back pain lacks a pathoanatomical cause and is considered non-specific.
Unless the inquiry might result in a different course of treatment for a particular disease process, diagnostic examinations are generally not recommended in the initial care of low back pain. If there are any red flags, immediate imaging may be necessary. As part of the standard diagnostic workup, lumbar spine MRI is conducted after plain film radiography. In certain situations, CT scanning might still be useful.
A degenerative cascade affecting the facet joints and the lumbar intervertebral disc leads to lumbar spondylosis or osteoarthritis. As one age, the cascade is believed to have been started by an insult or hurt. Genetic variables also play a major role in the cascade. The lumbar disc first experiences internal disc disruption due to circumferential annular rips; disc resorption then occurs, resulting in disc height loss and the eventual development of an osteophyte (bone spur). Degeneration starts with a synovial response that causes the facet joints’ cartilage to become disrupted. From there, osteophytes, joint capsular laxity, and joint subluxation develop.
When these disorders come together, it can cause spondylolisthesis, or segmental spinal instability (slippage of one vertebra on another). Radiculopathy and/or spinal stenosis in the lumbar spine can be caused by progressive spondylosis, which can cause structural constriction around the lumbar nerve roots. The most prevalent location for lumbar spondylosis, which is a common asymptomatic disease, is the L4-5 segment.
There are several possible causes of lumbar spinal nerve root compression, damage, or irritation. This usually happens as a result of an acute disc herniation or the degenerative cascade. Compression of the lumbar nerve can cause a constellation of symptoms known as lumbar radiculopathy, sometimes known as sciatica. Patients report with varying degrees of lower extremity weakness, paresthesia (numbness/tingling), and radiating pain.
The disease known as lumbar stenosis causes the spinal canal to narrow. Usually, spondylolisthesis and degenerative spondylosis are the causes of this constriction. Individuals typically present with pain/paresthesias in the lower extremities and/or lower back, which exacerbate with lumbar extension, standing for extended periods of time, and walking. The pathophysiology seems to be caused by ischemia brought on by mechanical compression of the lumbosacral spinal nerve roots.
Depending on the confirmed diagnosis, low back pain treatment is tailored. The first course of treatment is conservative and involves a multidisciplinary strategy using both pharmaceutical and non-pharmacologic therapy. Physical therapy, manual therapy, acupuncture, at-home exercise, cognitive behavioral therapy, etc. are examples of non-pharmacological therapies. To address lumbar radicular pain that is resistant to treatment, clinicians can employ interventional therapies such as epidural steroid injections. Radiofrequency ablation of the medial branch can be used to relieve pain originating from the facet joints.
Conclusion
The lower back portion of your spinal column, or backbone, is called your lumbar spine. There are five bones in total (L1-L5). The muscles, tendons, ligaments, spinal cord, intervertebral disks, and nerves are additional components in or surrounding your lumbar spine.
Your lumbar spine facilitates a broad variety of motions and bears the weight of your body. Your lumbar spine may be impacted by a number of conditions. Thankfully, these problems can be treated with a variety of surgical and nonsurgical treatments.

28 Comments