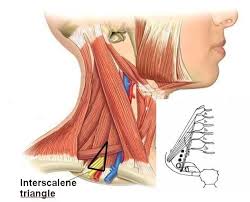
Inter Scalene Triangle
What is an Inter Scalene Triangle?
An important structural segment near the base of the neck is the inter-scalene triangle. The upper limbs depend on the neck’s components functioning properly. The lower section of the first rib, the medial boundary of the scalene anterior muscle, and the scalenus medius muscle’s midpoint line define the inter-scalene triangle’s borders.
A diagnostic sign of problems in the interscalene triangle is the thoracic outlet syndrome which should cause compression at the interscalene triangle, which should result in harm to the upper limb’s vascular or neurological systems. If the condition’s symptoms are severe enough to interfere with everyday activities or compromise the upper limb, surgery may be necessary to decompress.
Structure and Function
The first vertebrae is the most balanced, wide, and twisted of all the spinal columns. The medial half of the first vertebrae adheres to the manubrium sternum, while the head of the vertebrae clings to the T1 vertebra’s body along its length. The inter-scalene triangle’s top surface has features such as a subclavian artery groove and the scalene tubercle, with which the scalenus anterior muscle is connected.
The transverse process gives rise to the anterior scalene, which ends as a little tendon at the first rib and is joined to the scalene tubercle on its upward aspect of the C3–C6 cervical spine anterior tubercles. These muscles help with respiratory effort by supporting the elevation of the first rib and facilitating postural stability, neck flexion, and rotation.
Nerve Supply
The c3 to c5 cervical spine, which is home to the higher part of the interscalene triangle, corresponds to where the brachial plexus lies at a particular landmark where the muscle punctured. The brachial plexus’s cords regulate sensation and motor movement from the shoulder to the fingers.
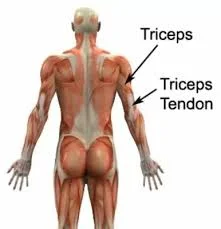
Major declines in quality of life can result from injuries to this plexus. The brachial plexus branches then travel behind the collarbone, and the cords extend out from the axillary artery to end in separate branches that feed the upper limb’s muscle and cutaneous innervation.
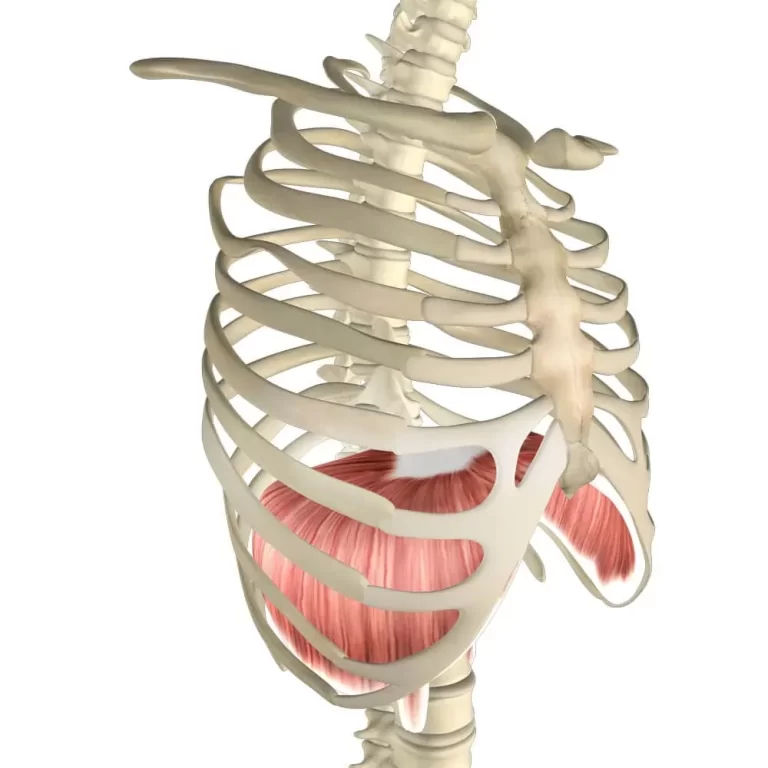
The phrenic nerve, which is not located within the triangle but regulates the diaphragm muscle for respiration, is comparable to the subclavian vein in that affecting Its proximity to the scalene triangle. The long thoracic nerve is an accessory nerve that has links to the inter-scalene triangle but not the inner part of the inter-scalene triangle. The serratus anterior muscle receives sensation from this sensory nerve, which also becomes subcutaneous close to the first and second ribs.
The study of embryology
This anatomical region is not particularly related to embryology, knowledge of how the surrounding muscles and tissues grow can offer some background.
Occasionally, during embryonic development, the primary source of the neck muscles, which includes the scalene muscles, is restricted to mesodermal tissue. These sometimes produce Myotomes, which are later separated into distinct muscles. The fourth, fifth, and sixth cervical myotomes are specifically where the scalene muscles get their start.
In clinical practice, the inter-scalene triangle is a crucial anatomical marker, especially when working with the brachial plexus, subclavian artery, and other systems that travel through or close to this triangle. Surgeons, anesthesiologists, and other medical professionals who work in this area must comprehend its contents and boundaries.
Somatic cells, which are unique cell masses, make up the paraxial mesoderm. These subsequently create the sclerotome and dermomyotome, the latter one of which forms the body wall muscles.
Blood Flow and Lymphatic System
It begins on the aortic arch’s left and right sides at the brachiocephalic artery. The subclavian arteries climb superolaterally from their initiating point, curve laterally, and travel posteriorly to the anterior scalene triangle to penetrate the scalene triangle. The subclavian vein is still present at the triangle’s bottom edge. The contraction of these vascular structures must impact imperfection, numbness, and vascular impairment.
Adjacent to the medius and posterior scalene muscles, the anterior scalenus is the front side muscle for which it is responsible. The interscalene triangle begins at the vertebrae’s transverse processes and the cervical spine’s anterior tubercles, which extend from C3 to C6. initially, the first rib uppermost margin and scalene tubercle are joined just in front of the subclavian artery groove by a single, flat tendon that is released by the scalene anterior.
Initial and ending location of scalene anterior
Every so often, a few muscle slippages that penetrate the suprapleural membrane are released by the scalenus anterior muscle. The muscles that cause these slips are the Sibson, Albinus, or scalenus minimus (pleuralis) muscles. This anatomical difference is 7–46 percent common in people in general. For the people who possess it, the front portion of the transverse process of the anterior primary rami of the cervical c7 vertebra is where the scalene minimus muscle begins.
Relationships
There exists a relationship between the center part of the scalene anterior and the initiating regions such as the brachial plexus, pleura, suprapleural membrane, and subclavian artery, vein. The first vertebrae generate the scalene anterior gap’s lowest boundary, while the scalenus medius generates its posterior part. The inferior border and posterior region are significant even though they pass through the brachial plexus trunks and the third portion of the subclavian artery.
The scalenus anterior was perforated by cervical segments C4 to c6.
Blood transfer: The scalene muscles receive blood supply from the thyroid artery’s cervical branch. The thyrocervical trunk accesses the thyroid artery.
Function: The scalenus anterior muscle affects the atlanto-occcipital joints, which are located in the middle of the cervical vertebrae. Depending on how the head is positioned and how the muscle contracts, the scalenus anterior can execute the following movements.
- The neck flexes when bilateral muscle contraction occurs when the costal attachment is fixed.
- One unilateral muscular contraction causes the neck to bend to the same side when the head is in the straight position of anatomy and facing forward or to the same side.
- The first rib may be stabilized or raised upwards by the scalenus anterior muscles when they are stabilized about the spinal column. The ribs are raised 2–12 when the external intercostal muscles contract in tandem with the scalenus anterior action, increasing the thorax’s anteroposterior width. The muscle functions as an auxiliary respiratory muscle rather than a major respiratory muscle because it only does so during forced breathing.
Initial and terminating location of the scalene medius muscle
The medius is the scalenus’s biggest and widest muscle. It originates from the transverse processes of the C2 and the posterior tubercles of the transverse processes of the C3 to C7 and the transverse processes of the atlas (C1). A tendon derived from the posterolateral extension of muscle fibers pierces the upper margin of the first rib.
Relationships
The front side outer surface of the scalenus medius is surrounded by a muscle defined as the sternocleidomastoid. The root of the scalene medius muscle is home to a few anatomical features. The anterior surface of the scalene medius is the location of the dorsal scapular nerve as well as the nerve that penetrates the serratus anterior muscle.
The muscles that these axons supply, the rhomboids and serratus anterior, are where they begin on the lateral side of the muscle and extend toward them in that sequence. the muscles that are linked to the posterolateral surface of scalene medius are two levator scapulae
the nerves which passed via scalene posterior are c6 to c8 cervical spine
Blood transfusion: The scalenus anterior, which parallels the upper cervical segment of the inferior thyroid artery, shares the same blood supply with the scalenus medius.
Function: when the neck flexes excessively that time the scalene medius muscle contracts easily. Similar to the scalenus anterior, this muscle helps raise or stabilize the first rib during breathing when its spinal attachment is fixed.
The initial and terminating landmark of the posterior scalenus
the scalene family constitutes three muscles in which the scalene posterior-most the shortest member. The fibers of the cervical vertebral column begin at the scalene posterior’s back region.
Stretching out sideways, the muscle slowly narrows into a thin tendon that binds the exterior edge of the second rib, and The serratus anterior muscle’s connection point is situated at the site of insertion.
the nerves which passed via scalene posterior are c6 to c8 cervical spine
Blood transfer: The upper cervical branch of the thyroid artery supplies blood to the scalenus posterior, exactly like it does to the other scalene
Function: Adjacent lateral neck flexion results from asymmetrical contraction of the scalenus posterior muscle when the costal attachment has been secured.
Anatomical variantions
There are deviations in the origin of the anterior scalene muscle and the ending point is the same from c2 to c6. The anterior scalene in particular may cause hypertrophy in certain cases, which could lead to subclavian artery aneurysmal alterations later on.
There can be variations in the anterior and middle scalene insertions on the first rib, resulting in a narrow area that raises between the subclavian artery and brachial plexus above normal. When conducting a surgical intervention in this spot, it is crucial to remember this.
In a similar vein, an insertion of muscle might go through the middle scalene and under the first rib. Rarely, the brachial plexus and artery must pass through the muscular sheat due to the mingling of the anterior and middle scalenes. There are other variations than the muscles. The first rib may have a fusion of ribs, irregular placement, or a repaired fracture, among other structural abnormalities that reduce the available space. Any difference can make the structures more difficult to see and may require additional non-surgical or surgical treatment.
Clinical Importance
The scalenus syndrome
The pathological condition known as “Scalenus syndrome” is characterized by symptoms that stem from the contraction of the c3 to c5 nerves in the inter-scalene triangle. Pain, numbness, tingling, alterations in sensation, and weakening in the muscles of the upper extremities could be the clinical presentation. The neurovascular strategy in the inter-scalene triangle is shortened as an outcome of secondary hypertrophy fetched on by spasms in the scalenus anterior muscle.
It is believed that the muscle’s myositis is what triggered the spasm. Additionally, hypertrophy applies strain on the subclavian artery and lower brachial plexus. Williams also mentioned that the triangle’s neurovascular structure naturally tends to move ventrally. Scalenus syndrome and TOS are assumed to be comparable. Nonetheless, these two medical categories differ in several ways.
A condition resulting from anomalies in the musculoskeletal system that create irregularities in motor function and sensory perception. Pain in one particular region of the body is referred to as myofascial pain syndrome. The existence of a taut band, which produces irritable areas called trigger points induced by acute trauma, chronic strain, or sustained contraction of a single muscle, can separate myofascial pain syndrome from fibromyalgia.
The anterior and medial scalene muscles are the source of one of the most prevalent forms of myofascial pain syndrome, which results in regional pain syndrome that radiates down the neck and into the arm. Even though the nomenclature for this illness is already widely recognized Because they are less knowledgeable about soft-tissue issues, doctors frequently mistake or overlook it in regular practice, and it reproduces radiculopathy. Inadequate diagnosis may outcome in improper therapy, which in turn can cause reflex sympathetic dystrophy.
Interscalene Block
Nerve blocks might be utilized during the postoperative phase following surgery to lessen the patient’s pain. The inter-scalene nerve block is a commonly employed type of nerve block that is exclusively utilized for numerous upper extremity injuries. This nerve block allows for anesthesia of the cervical plexus, musculocutaneous, suprascapular, lateral pectoral, and axillary nerves.
Anesthesia is possible to do earlier or following shoulder surgery. Lessening the chance of damaging the closest major nerve structures, such as the dorsal scapular and long thoracic nerves, the needle is put in a mediolateral manner. One prospective trial found that the probability of long-term problems after interscalene nerve blocks was 0.4%; yet, as the upper limb is essential to everyday functioning, any malfunction has a markedly damaging effect on a patient’s standard of living.
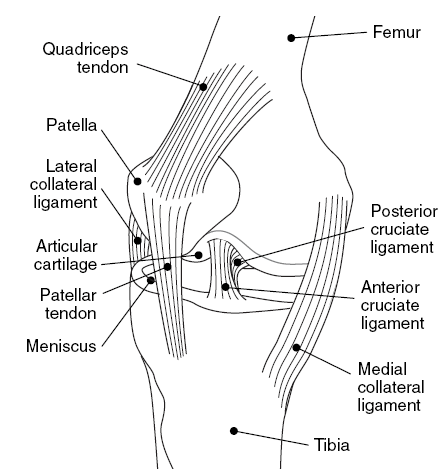
The Thoracic Outlet syndrome
At 3 to 8 cases per 1000 persons, thoracic outlet syndrome (TOS) is a prevalent syndrome caused by strange regional architecture or damage to the related systems. Crucially, the interscalene triangle is one of three locations where compression can occur to the vital neurovascular structures that go from the neck to the upper limb. compression of the vein also happens in patients without having TOS, compression of the subclavian artery is a more accurate diagnosis. Numerous factors can lead to this illness, such as trauma, congenital anomalies of the first rib, cervical ribs, fibrous bands, aneurysms, and supernumerary scalene muscles.
The clinical thing known as thoracic outlet syndrome is a collection of pathological things that vary depending on the particular structure being compressed and causing symptoms, as well as the site of squeeze: the subclavian vein’s thoracic outlet syndrome, the brachial plexus’s thoracic outlet syndrome, the subclavian artery’s thoracic outlet syndrome, and the differed Thoracic outlet syndrome, which is a general TOS with no clear explanation.
Thoracic outlet syndrome has historically been seen as a challenging condition to diagnose for these reasons, in part because there isn’t a recognized clinical diagnostic tool. Any paraesthesia, weakness, or heaviness in the affected upper limb, together with any discomfort in the chest, neck, occiput, shoulder, or upper limb, must be noted. Examining the patient may reveal Raynaud’s phenomenon, upper limb ischemia, edema, cyanosis, muscle atrophy, or wasting, according to the source and spot of the compression. Moreover, the interscalene triangle mandates to reproduction of the patient’s symptoms if this type of thing comes to mind at the palpation level. It is well known that thoracic outlet syndrome does not have a different clinical appearance.
When examining a patient who may have thoracic outlet syndrome, diagnostic techniques such as CT angiography, magnetic resonance angiography, specialized venography or arteriography, nerve conduction investigations, needle electromyography, and ultrasound may be used. Numerous factors should help in the diagnosis of TOS. Pain or weakness in the face and upper torso, irritation in the anterior or middle scalene, a positive Tinel test, a positive neck tilt test, and a positive costoclavicular compression test are among the conditions that may be present.
Brachial Plexus Injuries
The nervous system extending from the brachial plexus to the upper limb is responsible for controlling movement and sensations. Injuries to this network should outcome from trauma or contraction within the interscalene triangle. In this field, research on epidemiology examines the prevalence, causes (such as trauma from accidents or sports injuries), and consequences of these injuries.
Subclavian Vein Thrombosis
Compression or injury to the interscalene triangle may cause this disorder, which should result in the appearance of a clot in the subclavian vein. Epidemiological studies look at incidence rates, treatment outcomes, and risk factors (including variables such as venous catheterization or hypercoagulable conditions).
Anatomical Variations
Someone may be predisposed to specific illnesses due to variations in the anatomy of the interscalene triangle, such as the existence of an additional muscle or incorrect positioning of components. Research in epidemiology may examine the frequency and therapeutic consequences of these differences.
Anesthetic and Surgical Considerations
Epidemiological studies also look into the results of surgeries or interscalene triangle-related regional anesthetic methods. Complications, treatment efficacy, and patient outcomes after local interventions are all included in this.
Surgical Points to Remember
Scalenectomy
Scalenectomy is one potential therapy for upper thoracic outlet syndrome; first rib reduction might also be considered for lower thoracic outlet syndrome. For optimal outcomes, both procedures could be carried out together. In any case, the purpose of these procedures is to provide more access for the vascular and nerves to reach the remaining upper limb. The trans-axillary or supraclavicular approaches can be used to execute this treatment, and the available data does not show any appreciable differences in safety or complication rates between the two methods.
It is achievable to carry out a scalenectomy strategy without separating the anterior scalenus muscle. Before the first rib partitions, the scalenus anterior and medius muscles are determined and disjoined. Nonetheless, a scalenectomy technique can also be carried out without dividing the anterior scalenus by employing an interscalene approach. Otherwise, scalene muscle injections might be used as a precautionary approach to lessen pain instead of surgical surgery. Patients with whiplash or traction injuries that result in thoracic outlet syndrome respond better to this injection.
Treatment
Treatment with physiotherapy for problems associated with the interscalene triangle, like thoracic outlet syndrome (TOS), usually takes an integrated approach to lessen pressure on the blood vessels and nerves that run through this region. These are a few typical physiotherapy interventions:
Correcting any anomalies in posture that could lead to compression in the interscalene triangle is known as postural correction. This covers evaluations of workstation ergonomics and daily tasks.
Exercises to Stretch and Strengthen:
- stretching exercises of the scalene muscle can help release stress in the inter-scalene triangle.
- Upper Limb Strengthening: Exercises that target the muscles of the upper limb and shoulder girdle can assist increase stability and lessen stress on the nerves that go through the interscalene triangle
A Manual Methods:
- Soft Tissue Mobilization: Massage therapy and myofascial release techniques can help loosen up stiff muscles and improve the triangle’s tissue’s smoothness
- Joint Mobilization: To enhance joint function and lessen nerve compression, mild mobilization procedures can be used for the thoracic and cervical spine
- Neuromuscular Re-education: Methods to enhance movement patterns and coordination can assist minimize the risk of re-injury and maximize the shoulder and arm’s functional range of motion.
- Modalities: To control pain and inflammation, modalities including ultrasonography, electrical stimulation (like TENS), or heat/cold therapy may be utilized, depending on the individual symptoms and clinical findings.
- instruction and Lifestyle Adjustments: Patients can be empowered to adopt lifestyle adjustments that promote long-term symptom treatment and prevention by receiving instruction on posture, ergonomics, and other related topics.
- Respiration Exercises: Targeted breathing exercises to improve thoracic mobility and diaphragmatic respiration may be helpful in cases where thoracic outlet syndrome affects the brachial plexus and causes arm symptoms.
It is significant to acknowledge that the treatment approach has to be customized according to the patient’s unique ailment, symptoms, and therapy response. Creating a successful treatment plan requires a comprehensive evaluation by a physiotherapist or other healthcare professional with experience treating thoracic outlet syndrome or comparable diseases.
Summary
The important anatomical region described as the inter-scalene triangle can be found in the neck between the anterior and middle scalene muscles. Two important anatomical networks are the subclavian artery and the brachial plexus, which is composed of nerves providing the upper limb.
Thoracic outlet syndrome (TOS) can result from problems with the interscalene triangle, including compression of these blood vessels and nerves. Pain, tingling, numbness, and weakness in the hand, arm, and shoulder are possible symptoms.
Conditions affecting the interscalene triangle are usually treated using a multifaceted strategy. A key role is played by physiotherapy, which focuses on methods to reduce pain and enhance function, including posture correction, strengthening and stretching exercises, manual treatment techniques, and neuromuscular re-education.
Additionally, for long-term care and prevention of symptoms associated with interscalene triangle difficulties, patients must receive instruction on posture, ergonomics, and lifestyle adjustments. To optimize healing and enhance the quality of life for individuals affected, a comprehensive treatment plan that is tailored to each patient’s requirements and supervised by a medical professional is implemented.
FAQs
By what nerve does the scalene triangle pass?
The anterior and middle are the aimed muscles found in the center of the first rib. Before the scalene triangle crosses the subclavian nerve. The scalene is the muscle where the subclavian artery and brachial plexus nerves pass through.
By which route do the interscalene triangles travel?
the subclavian artery serves circulation to the interscalene triangle.
The Interscalene triangle: what is it?
The portion of the neck referred to as the interscalene triangle, or scalene triangle, is crucial to the operation of the upper limbs.
In thoracic outlet syndrome, what are the triangles?
A series of illnesses known as thoracic outlet syndrome causes compression of the neurovascular structure flowing via the thoracic outlet. It was initially identified in 1956. The three places where TOS usually appears are the subcoracoid area, the costoclavicular area, and the scalene triangle.
References
- Physiotherapist, N. P. (2023b, December 13). Inter-scalene Triangle – Structure, Function, Border. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/inter-scalene-triangle/
- Europe PMC. (n.d.). https://europepmc.org/article/med/31334942
- Scalene muscles. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/scalene-muscles
- Anatomy, Head, and Neck: Inter-scalene Triangle. (2024, January 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/31334942/