Foot Drop
What is a Foot Drop?
Foot drop is the incapacity to elevate the forefoot as a result of the foot’s dorsiflexor insufficiency. This can thus result in a dangerous antalgic gait and even falls.
Drop foot, a broad phrase indicating difficulties elevating the front portion of the foot is frequently used to refer to foot drop. When walking, a person with a foot drop may feel their front foot-dragging on the ground. Foot drop isn’t an illness. Instead, it indicates the presence of an underlying neurological, musculoskeletal, or even anatomical issue. Foot drop can occasionally be transient or permanent. In order to maintain the foot in its natural posture, a patient with a foot drop may need to wear an ankle and foot brace.
Foot drop is an irregularity in gait caused by the dropping of the forefoot. It can be caused by injury, irritation, or weakening of the deep fibular nerve (deep peroneal), which includes the sciatic nerve, or it can be caused by paralysis of the muscles in the anterior part of the lower leg.
Usually, foot drop is not the illness as such, but rather a sign of a larger issue. The primary characteristic of foot drop is dorsiflexion, or the inability or reduced capacity to elevate one’s foot off the ankle. Depending on the degree of muscular weakness or even paralysis, it might be either transient or permanent and affect one or both feet.
Before creating a therapeutic strategy, a complete knowledge of the underlying pathophysiology is required. This article will go over the diagnosis, therapy, clinical characteristics, and causation.
Anatomy
Lumbar Nerve Roots
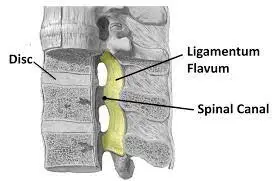
The lumbar vertebrae number five. The inferior facet of the rostral vertebrae and the superior facet of the caudal vertebra create the lateral spinal recess from which the lumbar nerve roots emerge. Between the L5 and S1 vertebrae is where the L5 nerve root exits.
Lumbar Plexus
The anterior rami of spinal nerves L1-4 make up the lumbar plexus. This plexus gives rise to many nerves. The transverse abdominis and internal oblique muscles are supplied by the iliohypogastric and ilioinguinal nerves. The thigh’s adductors are supplied by the obturator nerve. Large and supplying the quadriceps femoris group, the femoral nerve continues as the saphenous nerve, the medial leg’s sensory nerve.
Sciatic Nerve
The sciatic nerve, which has nerve roots from L4 to S4, is the biggest branch of the lumbosacral plexus. It passes through the popliteal fossa in the rear thigh. The tibial and common fibular (formerly peroneal) nerves split off at this point. The plantar flexors, invertors of the foot, and hamstrings are innervated by the tibial.
Common Fibular Nerve
The sciatic nerve’s lateral terminal branch, which crosses the gastrocnemius muscle’s lateral head laterally, is called the common fibular nerve. After there, it goes around the fibular head, where it is susceptible to compression since it is subcutaneous. It splits into the deep and superficial fibular nerves as it moves between the fibula and the fibularis longus muscle.
A little region in the first web gap between the first and second toes receives sensation from the deep fibular nerve, which also innervates the ankle and toe extensors. The dorsum of the foot and the lateral calf get sensation via the superficial fibular sensory branch, whereas the superficial fibular nerve provides the brevis, fibularis longus, and major evertors of the foot.
Causes of Foot Drop
Compressive Disorders
Compressive neuropathy can result from impingement syndromes of the fibular nerve at different points along its anatomical course. The most prevalent mononeuropathy affecting the leg is common fibular neuropathy at the fibular head. Pressure palsies can occur because the fibular nerve is rather superficial in proximity to the fibula’s head.
Between the gastrocnemius and distal biceps, anatomic differences in the biceps femoris muscle can help generate a tunnel that may put the nerve at risk of compression. Weight loss, extended bed rest, constriction of the cast, lesions consuming space, and bone metastases affecting the fibular head are further contributing factors
Foot drop has been observed as a result of sciatic nerve compression between the two heads of the piriformis muscle.
It has been observed that prolonged bed rest can cause compression palsies in intensive care units. It has been estimated that 10% of patients who remain in the intensive care unit (ICU) for more than four weeks may get fibular paresis. Foot drop can also be a symptom of many motor and sensory nerve polyneuropathy associated with critical disease. The degree of participation will determine if a weakness is bilateral. Individuals with diabetes are at an increased risk of developing compression neuropathies.
Foot drop can also be often caused by lumbar radiculopathy. The most prevalent kind of lumbar radiculopathy, L5 radiculopathy, is usually caused by spondylitis or lumbar disc herniation in the spine.
It is known that disc herniations and bony (osteophytes ) or ligamentous (sacroiliac ligament and lumbosacral band) compression can cause extraforaminal compression of the L5 nerve. Foot drop can be caused by cancer of the bone at the fibular head, though this is not frequent.
Traumatic Injuries
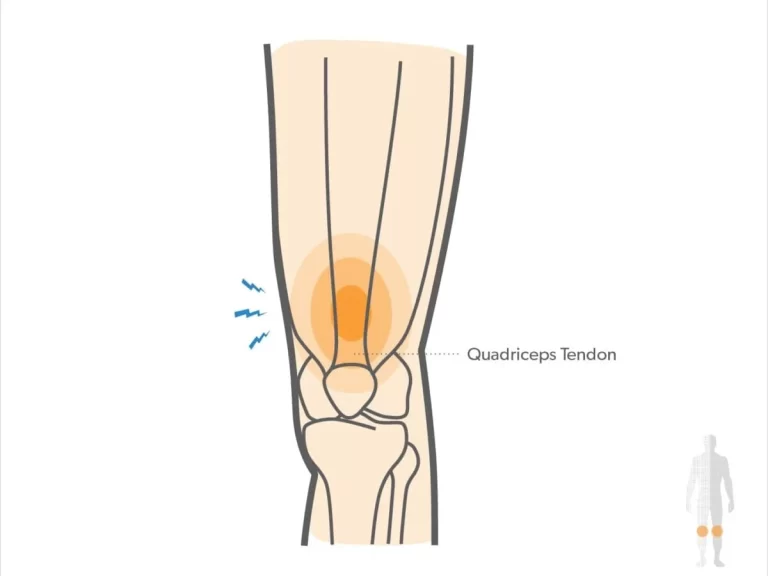
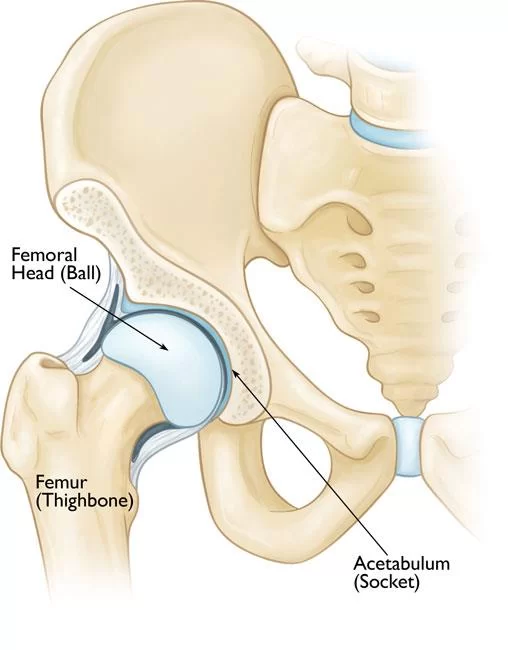
Orthopedic injuries such as fractures, musculoskeletal injuries, blunt trauma, and knee dislocations frequently occur with traumatic injuries. The most prevalent causes of sciatic neuropathy are hip traumas or complications from surgery. The second most prevalent mononeuropathy affecting the lower limb is sciatic neuropathy, which usually occurs as a foot drop.
Lumbrosacral plexopathies, which can be brought on by radiation therapy, neoplasms, abdominal or pelvic surgical complications, or severe injuries, are less prevalent causes.
Neurologic Disorders
Amyotrophic lateral sclerosis (ALS), sometimes referred to as Lou Gehrig disease or motor neuron disease (MND), is a neurodegenerative illness that causes muscular weakness, and difficulty speaking and swallowing due to the loss of motor neurons in the anterior horn cells. A simple foot drop might be used for the initial presentation.
Hemiplegia is one of the symptoms of cerebral vascular disease (CVD). There is a foot drop in this presentation. Additional indications of involvement of higher motor neurons include hyperreflexia, circumduction of the lower extremities while walking, and elevated muscular tone. Depending on where the ischemia occurs, aphasia may manifest.
The term “mononeuritis multiplex” refers to the involvement of one or more peripheral motor and sensory nerves. Usually, it pains and is asymmetrical. It has been linked to rheumatoid arthritis, granulomatis with polyangiitis (Wegener granulomatosis), hepatitis, leprosy, and AIDS. Certain nerve malfunctions may be linked to loss of mobility and sensation. One of the nerves that are frequently affected by this illness is the sciatic nerve. Small epineuria artery vasculitis damages the axons, impairing nerve transmission and ultimately resulting in muscular weakness.
Acute inflammatory demyelinating polyneuropathy (AIDP), which is often referred to as Guillain-Barré syndrome, is an autoimmune disorder characterized by increasing motor weakness, sensory loss, and areflexia. Motor weakness frequently predates sensory complaints. This illness frequently comes with autonomic dysfunction. Segmental demyelination is caused by damage to the myelin sheath. The slowing of nerve conduction velocities and conduction block are characteristic features of AIDP. A clinical presentation may include a foot drop.
One of the most prevalent types of hereditary neuropathy is Charcot-Marie-Tooth (CMT), a primary congenital demyelinating peripheral neuropathy. Both motor and sensory nerves are affected. It occurs once every 25000 years. One of the primary signs and symptoms is lower leg muscular atrophy and foot drop, which results in the typical “stork leg” image.
Foot drop is frequently caused by somatic stimulation conditions and conversion response. If the diagnosis is generally routine, a mental examination needs to be taken into consideration. It should be pointed out that in situations of poor or no effort for ankle dorsiflexion or other motor groups, both the needle EMG and nerve conduction components of the electrodiagnostic medicine testing will seem normal.
Other causes include:
- Complete or partial hip replacement
- knee replacement
- injury to the sciatic nerve
- The cauda equina condition. This disorder involves compression of the spinal cord’s tail nerves, typically brought on by a tumor or “slipped” disc.
- Peripheral neuropathy with diabetes
- Different kinds of stroke
- cause of the epidemic attack
- Multiple sclerosis
- cerebral palsy
- The illness Charcot-Marie-Tooth.
- The poliomyelitis
- illness of the motor neurons
- Ataxia Friedreich’s
- brain tumor
- adverse response to booze or drugs.
- Even though they may have a comparable high-stepping stride, patients experiencing discomfort in the soles of their feet are not experiencing foot drop; rather, they are raising their feet for other reasons.
Epidemiology
There is variation in the reported incidence of fibular neuropathy. According to research, the prevalence is 19 per 100,000 persons, with men more likely to have it than women. It is estimated to be 0.79 following a total knee replacement, with a small male predominance of 2.8 to 1. Ninety percent are unilateral. Both the left and right sides are impacted equally.
ALS: The annual incidence of ALS is estimated to be 1.54 per 100,000 people globally. Though it can strike at any age, the frequency of ALS peaks between the ages of 50 and 75.
It is known how common mono neuritis multiplex is throughout the world at large and in the US in particular.
Men are affected by AIDP at a rate of around 1.5 times higher than women; the yearly incidence was found to be 1.0 to 1.2 per 100000 and increased linearly with age.
Pathophysiology
An understanding of the categorization of nerve injuries is required in order to understand the pathophysiology and project the future prognosis of peripheral nerve damage. London offered the following categorization in 1943 (Seddon), 1953 (Sunderland), and 1944 (Neurapraxia, axonotmesis, and neurotmesis).
Myelin breaks down in neurapraxia, even though axons are spared. There are no injuries to the endoneurium, perineurium, or epineurium. At the location of damage, there are changes in the conduction of nerve impulses. Clinically speaking, this is sensory loss and weakening. This is reflected in the EMG as a slow nerve conduction velocity throughout the compressed segment and a prolonged delay. This kind of damage heals the most rapidly.
Axonotmesis is a condition where the perineurium and epineurium are undamaged but the axon is injured. Below the site of nerve damage, these nerves indicate sensory and motor deficiencies when stimulated. Long-term recovery is possible, but it might not always be complete.
The most serious kind of nerve damage is called neurotmesis. There is damage to the myelin, axons, and supporting connective tissue. Wallerian degeneration takes place away from the damaged site. Clinically, this manifests as deficiencies in motor and sensory function. Healing on its own is not possible. Sometimes surgery is required, and this might involve tendon transfer or nerve grafting.
Histopathology
Neurapraxia, axonotmesis, or total neurotmesis may occur, depending upon the degree of compression, inflammation, or damage.
The myelin sheath is momentarily damaged in neuropraxia, while the nerve itself remains unaffected. Usually, recovery is complete.
The breakdown of the myelin and axon is known as axonotmesis. However, the connective tissue is still present. There is Wallerian degeneration. When electromyography (EMG) is conducted two to four weeks after the injury, the implicated muscles distal to the site demonstrate positive sharp waves and denervation potentials known as fibrillations.
Although a more severe crush or contusion is typically the cause of axinotmesis, it can also happen when the nerve is stretched (without damaging the epineurium). The nerves try to regenerate distally via regeneration at a rate of either 1.5 mm per day or 2 to 3 mm per day. Regeneration takes weeks or years to complete
A complete division of the nerve, as in penetrating trauma, is known as neurotmesis. The axons are totally damaged, and the myelin is absent. The perineurium may be intact when endoneurium tubes and connective tissue elements rupture, are disturbed, and/or transected. There is no chance of recovery without surgical re-anastomosis.
Signs and symptoms of the Foot Drop
Steppage gait is the primary indicator of foot drop. The issue causes people to drag their toes along the floor when walking, thus they may bend their knees to raise their feet higher than usual to prevent the dragging. The anomalous decrease in the foot’s potential to be lifted off the ground during the swing phase of typical walking is this. In a gait cycle, the portion of the foot that rises off the ground before the heel presses down for the following step is referred to as the swing phase. In order to avoid slapping and toe dragging, this raises the foot sufficiently.
The patient may employ the typical tiptoe walk on the opposite leg, which involves elevating one thigh excessively and having the toe drop, in order to accommodate the toe drop. Foot drop can also be indicated by other gaits, such as an extensive outward leg swing, which is primarily used to prevent elevating a thigh excessively or even to round corners in the opposite direction of the affected limb.
Even though they do not have a foot drop, patients with painful abnormalities of feeling (dysesthesia) of the soles of the feet may have a similar walk. A patient feels as though they are walking foot on scorching Sand since even the smallest pressure on one foot causes excruciating discomfort.
Unable to hold shoes: When wearing shoes that feel loose, it might hurt and drag the injured foot when you walk.
Tripping: Recurrent tripping may be caused by weakness in the toe and foot muscles.
Falls: It’s normal to lose one’s balance, walk, and fall with a foot down. The incapacity to raise the front of the foot and toes correctly when walking is the reason behind falls.
Circumduction gait: This walking pattern, which involves keeping one leg straight while swinging it to the side in a semicircle to go forward, is occasionally tried to prevent falls or even tripping.
Limp foot: An injured foot may droop away from the body and make stair climbing difficult.
Numbness: Loss of feeling may occur in the upper portion of the foot as well as the front, outside, or back of a lower leg.
Usually unilateral: When a foot drop occurs, it usually affects one foot, especially if the lower back or leg is squeezed.
Loss of muscle mass: Loss of muscle can result from weakening of the muscles, particularly in cases where autoimmune diseases like multiple sclerosis induce foot drop.
Romberg’s sign: Losing balance can occur when standing unsupported and when closing one’s eyes.
symptoms of foot drop due to a certain type of nerve compression foot drop, due to the underlying compressed nerve, can result in weakness, numbness, and/or discomfort in some parts of the foot and leg.
Typical instances include the following:
L5 radiculopathy, also known as lumbosacral plexopathy: Compression of the L5 nerve root or even an accumulation of lumbar and sacral spine nerves can result in a foot drop that can cause: Having difficulty moving the foot up or down at the ankle joint, turning the foot to the inner or outer side at the ankle joint, extending a leg away from the body at the hip joint and inward from the thigh, and experience lower back discomfort that travels down a leg are all examples of weakness in this area.
Common neuropathy or peroneal injury: A foot drop resulting from compression of the common peroneal nerve may induce weakness while rotating the foot to the outside of the ankle and when elevating the ankle joint upward. numbness in the front, side, and top of the foot of the lower leg.
Neuropathy caused by sciatica: When a sciatic nerve is compressed, a foot drop can result in Pain and numbness in the back of the thigh, side of the leg, and upper portion of the foot; weakness in rotating the foot to the outside and/or inner side at the ankle; and difficulty bending the knee.
Deep peroneal neuropathy: Compression of the deep peroneal nerve resulting in a foot drop may cause: unable to raise an ankle joint. In between the first and second toes, there is numbness in the skin
Differential Diagnosis
- Upper motor neuron involvement: a cerebrovascular accident might result in limb weakness. It is an unnaturally lengthy limb due to spasticity. A
- person must circumduct, or move their leg in a semicircular motion, in order to walk. There is also obvious dysphagia, aphasia, or paralysis in the upper limbs.
- Cerebellar gait: The balance and mobility of walking are due to the cerebellum. Two symptoms of cerebellar gait impairments include ataxia and inability to walk simultaneously.
- Bilateral presentation of ataxic gait. Position and vibration perceptions are impaired because of the involvement of lengthy spinal cord tracts. This causes side-to-side sway and excessive steppage, which are symptoms of alcohol use disorder.
- Extensive lumbar radiculopathy at L5
- Parkinsonian gait: Festinate gait, which is characterized by short, rapid steps, is brought on by substantia nigra involvement, which affects the gait cycle’s smooth transition.
- diseases of the lumbar plexus, such as diabetic amyotrophy, autoimmune diseases, and compressive tumors.
- In cases when the examination is normal and there is a possibility of significant secondary gain, depression, anxiety, or other suspected psychological problems, conversion response, sensory overload condition, and malingering should be taken into consideration.
Diagnosis
History and Physical Examination
Determining the probable cause of foot drop can be aided by a thorough history and physical examination.
It is important to see the patient do basic musculoskeletal testing, which includes heel standing, toe standing, and deep knee bending. It is recommended to perform and grade the primary lower extremity muscle groups (ankle plantarflexion, ankle dorsiflexion, ankle inversion, ankle eversion, knee extension, knee flexion, and hip flexion) using the MRC scale grading 0–5. In the distribution, a neurosensory examination for pinprick should be carried out, searching for lumbar dermatomes as well as peripheral nerves.
Manual motor testing may effectively measure muscle mass by comparing the major muscle groups’ bulk regions side by side. Measurements of the circumference taken side to side can be recorded and used to track the mass loss or gain over time. The American Spinal Cord Injury Association’s (ASIA) point and motor groups are standardized, which facilitates professional communication, however, they do not assess particular peripheral sensory nerves.
It is thought of as an extension of the physical examination to go for a formal electrodiagnostic medicine consult, which includes nerve conduction investigations and EMG. This may need to be obtained from the subspecialist, who is not usually the initial clinician involved in the patient’s treatment.
Any injury that affects the peripheral nerve’s neuraxis, which runs from the roots to the nerve, might impair the muscles it supplies.
Because the anterior compartment musculature is weak, a lesion of the lumbar plexus, sciatic nerve, common peroneal nerve, or deep peroneal nerve may result in foot drop. The inability to walk as previously is the presenting symptom. Specifically, a decrease in the foot muscles involved in dorsiflexion. The pain could be present or absent. Dorsiflexion won’t be possible for the person during the heel strike. The foot stays level with the surface. can occasionally result in toe drag and the inability to remove the foot. Falls might result from this.
Neuropathic pain usually begins in the lumbar area and radiates down the posterior thigh, anterolateral leg, foot, and big toe when there is radiculopathy affecting the fifth lumbar nerve root. The medial part of the foot, including the first webspace, is a site of sensory complaints. Foot dorsiflexor and evertor weakness are examples of motor symptoms.
Sciatic neuropathy-like sensory and motor impairments can also be present in lumbosacral plexopathies. Hip girdle muscles, such as hip abduction (gluteus medius) and hip extension (gluteus maximus), may also be affected by weakness.
The characteristic presentation of sciatic neuropathy is a sensory loss in the whole foot, along with ankle inversion and weakness in the gastrocnemius and soleus plantar flexors. One possible outcome is “flail foot.” Knee flexion weakness may also be caused by the involvement of the hamstring muscles. An incomplete sciatic neuropathy frequently manifests as a typical peroneal neuropathy. In the sciatic nerve, peroneal fascicles are frequently more susceptible to damage than tibial fascicles.
The patient with common fibular neuropathy has both motor and sensory impairments. Leg crossing, extended kneeling, immobility, or trauma are possible historical factors. The lateral leg below the knee and the anterolateral foot are affected by sensory loss or paresthesias. Ankle dorsiflexion (tibialis anterior), toe extension (e.g., extensor hallucis longus), and ankle evertors (peroneus longus and brevis) are all impacted by muscle weakness.
The only sensory impairments observed are localized toe and ankle extensor weakness and mild sensory abnormalities restricted to the web area between the first two fingers if only the deep fibular region is damaged. Eversion and inversion of the ankle are common.
Rarely occurring isolated superficial fibular neuropathy manifests as a sensory deficiency in the foot, with the exception of the first webspace. The only possible outcome is ankle eversion/inversion.
The stance phase makes up 60% of the gait cycle while the swing phase makes up 40%. In the stance phase, one foot is in motion while the other is in swing. Heel strikes on the same side represent the beginning and finish of the gait cycle. The foot stays level on the ground in the stance phase. Before entering the stance phase, the foot is in dorsiflexion during the heel strike, getting ready for a steady descent. When dorsiflexors are absent, the foot stays in plantar flexion during the stance phase. This keeps them from being able to get off the ground and get ready for the next step of their gait cycle. Either dragging their toes or raising their foot to a high level, the patient.
Evaluation
Plain radiographs of the pelvis, tibia, and fibula should be taken as part of diagnostic testing after a thorough physical examination to rule out fractures or dislocations. An MRI could be necessary.in plexopathies that may be caused by tumors or masses. When compressive neuropathies are present, lumbar spine, knee, and/or ankle MRIs may be recommended to look for possible soft tissue masses. If there is any indication of swelling at or close to the compression site, MSK ultrasonography is also employed.
When it comes to collagen vascular illnesses, it is important to evaluate key labs such as ANA and rheumatoid factors. To rule out alternative etiologies, a chemical panel and CBC differential should be taken into account.
An electrodiagnostic study is frequently a crucial test to support the clinical diagnosis or offer a different location and diagnosis. Additionally, this research can specify the extent of the damage and offer prognostic information. There are two sections to this study.1) Needle electromyography (EMG) and nerve conduction studies (NCS).
Studies on nerve conduction provide insight on the myelin’s energy. Reduced conduction latency is a sign of nerve compression. Nerve compression is indicated by the presence of delayed latency, slow velocity, and conduction block at the affected segment.
Needle electromyography: The muscles supplied by the studied nerve are injected with monopolar needles. Thus derived motor unit potentials are examined for recruitment patterns, firing rates, and amplitude. Potentials known as positive sharp waves and fibrillation potentials, which signify axonal involvement, are indicators of muscle denervation.
The electromyography can determine the location and degree of the lesion as well as predict the likelihood of recovery using the combined use of nerve conduction tests and EMG. A positive prognosis is indicated by the lack of denervation potentials and the existence of enough functional motor units on the needle EMG.
A weak probability of recovery is indicated by the presence of denervation potentials along with non-functioning motor units.
There is a wide range of neuropathy and myopathy associated with autoimmune and critical illnesses, and a comprehensive and exhaustive workup frequently yields a “clinical syndrome” instead of a definitive diagnosis.
Treatment of Foot Drop
Approach to the Patient
The approach to therapy for a patient is determined by the type of compressive lesion and the cause of the foot drop. Many options are available based on the assessment and diagnostic results.
Conservative Management
This includes the use of splints, physical therapy, and/or pharmaceutical treatment to treat pain. Stabilizing the gait and preventing falls and contractures are the main objectives of conservative therapy. Muscle strengthening and stretching are the main goals of physical therapy. Techniques for electrically stimulating the dorsi flexors on the weekends have demonstrated potential. An essential component of therapy should be a home exercise protocol, with the goal being to preserve the range of motion and strength of the muscle groups involved in flexion contracture prevention.
The use of splinting reduces contractures. To stop more plantarflexion in cases of full nerve palsies with minimal recovery, an ankle-foot orthosis (AFO) should be prescribed. It is important to provide adequate instruction and training to help with the correct use and care of the brace.
Medical treatment
Sympathetic blocks or even laparoscopic synovectomy can occasionally be used to effectively control the syndrome if unpleasant paresthesias occur.
Amitriptyline, nortriptyline, gabapentin, pregabalin, and duloxextine are alternative managements. Using diclofenac or transdermal capsaicin for local therapy may also help reduce symptoms. Narcotic drugs may be minimized even in cases of severe pain.
The naturally occurring hormone erythropoietin has been licensed by the US Food and Drug Administration for the treatment of anemia. It may also have neurotrophic and neuroprotective qualities. The action’s putative mechanism promotes cell survival by acting as an anti-inflammatory and anti-apoptotic agent.
Space-occupying lesions or underlying malignancy may give birth to medical oncologic problems. Peripheral neuropathy, usually symmetric and distal, can also be brought on by prior chemotherapy drugs. Peripheral nerves may become more susceptible to compression, nevertheless, if this or any other underlying peripheral neuropathy etiology is present.
Surgical Treatment
Nerve repair in trauma instances should happen no later than 72 hours after the damage. The most common primary nerve repair method is autologous nerve grafting.
Necrolysis and nerve decompression are necessary for total nerve compression. Generally, 97% of cases have reported going back to normal. Patients with equinus deformity may require surgery to relieve the deformity.
It may be necessary to transplant a nerve or tendon in situations of severe nerve dysfunction. This article is not intended to provide a comprehensive review of surgical alternatives.
Treatment for the other etiologies is initially conservative due to the possibility of spontaneous remission of symptoms, either partially or completely, over time.
Treatment Planning
Planning should be done for an early range of motion and possible strengthening. The electrodiagnostic study may help determine whether long-term bracing is necessary for the patient and whether the weakness will likely worsen or affect other motor groups. Early use of the ankle dorsiflexor brace helps to avoid more secondary musculoskeletal issues resulting from the changed gait cycle, as well as improving gait mechanics and fall reduction.
Radiation Oncology
Radiation-induced plexopathy can occur after previous radiation therapy. The electrodiagnostic investigation often reveals particular “myokymic discharges.” Potential recurrence should be taken into account in individuals who have needed radiation therapy in the affected area.
Surgical Oncology
There is a possibility that the space-occupying lesion will impact the lumbosacral plexus, which might lead to weakness in the legs. When considering other possible constitutional signs and symptoms and an underlying disease in situations of otherwise unexplained weakness, care should be taken. On the other hand, these instances are more likely to have a tendency toward genital femoral neuropathy and weakening of knee extension.
Postoperative and Rehabilitation Care
As already stated, occupational and physical therapy can have a significant impact on whether a patient receives conservative or surgical care.
Consultations
A physiatrist or neurologist consultation is required if the diagnosis is in issue. To determine the location of the damage and assess its severity, which affects the result, a referral to an electrodiagnostic laboratory is necessary. It is recommended to refer patients for gait examination, fall prevention, and brace maintenance to physical therapy. Whether the patient needs a permanent brace in the event of a bad recovery or a temporary brace while they wait for the nerve to regenerate, they should consult an orthopedist. Orthopedic surgery, neurosurgery, oncology, hematology, and psychiatric referral may all play a part in the patient’s overall care when they come with foot drop.
Physical Therapy treatment
Electrical modalities
- Electrical stimulation: Using electrical stimulation during walking may help reduce foot drop symptoms. Functional electrical stimulation is the name given to this management technique (FES). The little devices worn next to the knee respond to a leg’s movement and provide the muscle with low electrical stimulation to promote healthy movement.
- Transcutaneous electrical nerve stimulation, or TENS, is a pain management technique that uses a small electrical current. A TENS machine is a compact, battery-powered device with leads attached to adhesive pads known as electrodes.
- paraffin wax bath is a primary benefit of wax treatment for a patient is pain relief.
Exercise for Foot Drop
Passive range of motion exercise

- Passive dorsiflexion
First, the therapist should instruct the patient to sleep in a comfortable posture. For example, the patient may sleep on a bed with their knee straight and their foot elevated up off the bed. A physical therapist then lays one hand on the heel and the other on the bottom of the foot. Then, a physician carefully elevates the foot so that the patient’s toes face upward. Do it 10 times in one sitting. Work out three times a day.
- Passive inversion
Ask the patient to get into a comfortable posture before starting, such as resting on a bed with their knee straight and their foot out of the bed. Next, the therapist lays one firm hand on the heel and the other on the sole of the foot. Subsequently, the therapist softly inverts the foot, preventing the leg from rotating. Ten times throughout each session, do this. Work out three times a day.
- Passive eversion
A physical therapist should first instruct a patient to lie in a comfortable posture, such as on a bed with their foot propped up and their knee straight. Next, the medical professional lays one firm palm on the heel and another on the foot’s underside. Next, a medical professional gently extends the foot, but they prevent the leg from rotating. Ten times in a single session, execute it. Work out three times a day.
- Passive toe extension
First, take a seat on a chair and place the foot that needs to be treated over the other knee. Subsequently, the patient places one hand on the heel and the other on the toes. The patient then raises the toes as far as it is comfortable to do so. 10 times in a single session, do it. completing three sessions in a single day.
- Passive toe flexion
A physical therapist will first instruct a patient to sit in a chair and place the foot that needs to be exercised across the knee of the opposing side. The patient then places one hand on the base of one heel and another on the toes, moving the toes as far down as comfortable toward the tibia’s shin. Perform 10 times in a single session. In a single day, conduct three sessions.
Stretching exercises
- Achilles stretch

The calf stretch that the patient may already be used to is similar to the Achilles stretch:
To begin, first position yourself close to a wall or other support, such as a chair, and place your hands at eye level on the wall. The injured leg should then be positioned one step behind the undamaged limb. Next, maintain the heel of the affected leg on the ground while bending the damaged knee until the patient experiences a stretch in the leg.
The secret is this: To extend the Achilles tendon, slightly bend the maintain knee.

- Towel stretch
To do this, first, sit on the ground with your legs straight in front of your face. Next, round each foot’s toes with the towel. Next, slowly push back until the patient begins to feel a stretch in the back of their lower legs and at the very bottom of their feet. Try to maintain this position for around 30 seconds. Three times throughout a session, repeat it. Work out three times a day.
- Big toe stretch
It’s important to maintain a large range of motion in the big toe.
To carry out this task: Tell the patient to sit up straight in the chair and place their foot flat on the floor to start. Next, place the foot that is injured on the thigh that is not injured. Next, gently extend a big toe sideways, upward, and downward with your fingers. After that, hold each big toe position for thirty seconds. Three times throughout a session, repeat it. Work out three times a day.
- Band Stretch
The band or strap can be used by the patient to help with stretches as well. Similar to a towel stretch, this type of prop can help extend a stretch further.
To stretch a towel inside out: Place the band or towel around the injured foot and sit down to begin. The patient’s hands should then be used to firmly grip either end of a towel. Next, progressively rotate the ankle inward so that the patient stands with the undamaged foot with their sole pointing front. Then, to deepen a stretch, pull up on the towel using the hand side that is not injured. Take a 30-second break between each repetition. Perform it thrice in a session. Make three sessions a day.
- Standing calf stretch
A patient may get into the standing posture in order to increase the stretch’s tension:
Start by placing one foot approximately 12 inches in front of the patient while standing facing a wall or other support, such as a chair. Point the toes upward next. Subsequently, the therapist instructs the patient to gradually bend forward until the rear of the lower leg is stretched. For thirty seconds, maintain this posture. Do this exercise three times in a session. Work out three times a day.
- Standing soleus stretch
The patient is first instructed by the therapist to face the wall or other support while standing a few feet away from it. Next, plant one leg behind you so that your heel is flat on the floor. The opposite leg can then advance in the direction of the support. After that, move the affected leg’s foot gently in the direction of the other foot. Next, bend the front knee slightly toward the support until the patient feels a stretch in the affected leg. For thirty seconds, hold this stretch. Perform three sets of three repetitions. Work out three times a day.
- Cross-leg ankle stretch
To begin, select a comfortable seat and cross the affected leg over the unaffected knee. Next, use the patient’s hands to grip the unaffected foot. Next, bend the ankle and push the affected toes downward with the unaffected hand, making it appear as though the patient is pointing at their toes. The patient should then be able to feel this stretch on the front of their foot and ankle. For thirty seconds, maintain this posture. Do this drill three times in a session. Work out three times a day.
- Chair pose
The therapist should instruct the patient to start by standing straight in tadasana. As the patient raises both arms up, inhale and turn their palms inward. Next, slightly bend both knees while the patient exhales, trying to bring the thighs parallel to the floor. Subsequently, the upper thighs and torso should form a right angle. Lastly, attempt to hold it for thirty seconds. Perform three sets of three repetitions. Work out three times a day.
Active-assisted ankle range of motion exercise
- Active-assisted dorsiflexion
First, instruct the patient to lie in a comfortable posture. For example, they can lie on a bed with their knee straight and their foot propped up off the bed. Next, a medical professional grips a heel with one powerful hand and applies pressure to the foot’s bottom with another. Subsequently, a physical therapist instructs the patient to elevate their foot for as long as possible. If the patient is unable to raise their foot between the range of motion, a clinician assists them in reaching the maximum range of dorsiflexion. So the toes point in the direction of the face. Ten times throughout each session, do this. Work out three times a day.
- Active-assisted inversion

First, instruct the patient to lie in a comfortable posture. For example, they can lie on a bed with their knee straight and their foot supported off the bed. Next, a physical therapist lays one firm palm on the inner border and the other on the foot’s bottom. The patient is then instructed to move their foot inside for as long as they can by a physical therapist. If the patient is unable to move their foot inward in between the motions, a clinician assists them in achieving the entire range of motion. Ten times in a single session, execute it. Work out three times a day.
- Active-assisted eversion
First, instruct the patient to lie down on a bed in a comfortable posture, with their foot propped up and their knee straight. Next, a medical professional lays one firm palm on the inside border and the other on the foot’s bottom. After that, a physical therapist assists a patient in achieving the entire range of motion when the patient is unable to move their foot outward during an action. The clinician offers the patient instructions to move their foot outward as long as possible. Ten times in a single session, do it. Work out three times a day.
- Active assisted toe flexion
First, instruct the patient to lie in a comfortable posture. For example, they can lie on a bed with their knee straight and their foot supported off the bed. Next, a medical professional lays one firm palm on the toes and the other on the bottom of the foot. The patient is then instructed to point their toes as far as possible toward the ground. If the patient is unable to bend their toes in between the actions, the physical therapist will assist them in reaching the maximum range of the movement. Ten times during a session, do it. Work out three times a day.
- Active-assisted toe extension
Ask the patient to first assume a comfortable posture, such as resting on a bed with their knee straight and their foot outside of the bed. Subsequently, a physical therapist applies pressure with one hand to the rear of the toes and another to the bottom of the foot. The patient is then instructed to move their toes upward, or toward their face, for as long as they can. If the patient is unable to extend their toes between actions, the physician will help them achieve the complete range of the extension movement. Ten times during a session, do it.
Active range of motion exercises
- Active ankle circles
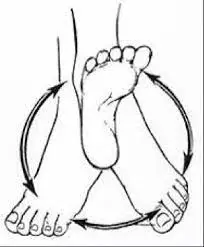
The range of motion can be improved with this exercise. The patient is able to do ankle circles while sitting or even while lying down:
Starting at the left ankle, slowly rotate it in circles, then move it to the right. Using the affected foot to create an alphabet in the air might be a simpler exercise for the patient. Take the big toe and lead it. Start with a small movement and focus on using only your foot and ankle—not your entire leg. Try performing ten circles in each direction when your foot is affected. If the patient is practicing the alphabet, have them finish three sessions a day on the affected foot.
- Toe extension
In order to perform this exercise, instruct the patient to sit up straight on a chair with their feet flat on the floor. Next, position the affected foot on the normal thigh. Next, raise the toes in the direction of the ankle. Not only should the heel chord feel stretched, but so should the bottom of the foot. While stretching, massage the arch of the foot to help release tension and soreness. Ten times during the session, repeat this exercise. Work out three times a day.
- Toe flexion
The patient should first be instructed to sit up straight in a chair with their feet flat on the floor. Next, position the injured foot on the healthy thigh. The toes should then be lowered toward the ground. Perform ten rounds in a session. Work out three times a day.
- Active dorsiflexion
First, have the patient lie down on a bed or select another comfortable posture. The patient should next be instructed by a physical therapist to bend their foot as far upward as possible, or toward their face side. In a single day, complete 10 repetitions of each session. Work out three times a day.
- Active ankle inversion
First, have the patient lie down on a bed or choose another comfortable posture. The patient should next be instructed by a physical therapist to bend their foot as far upward as possible, or toward their face side. In a single day, complete 10 repetitions of each session. Work out three times a day.
- Active ankle eversion
First, instruct the patient to lie down in a position that is comfortable for them, such as on a bed. Subsequently, the patient should be instructed by a physical therapist to move the foot inside as far as possible. Repeat a set 10 times in a session. Work out three times a day.
- Hip adduction and abduction
This exercise works the leg, but because it improves the tone (stiffness) of the leg, which may also help the foot, it is also helpful for foot drop. Start this lower-body workout while sitting down. Next, do a hip adduction, or inward push, toward the midline with the affected leg. Next, abduct your hips and push the damaged leg outward, as if the patient were kicking a ball to one side. Ten times during the session, repeat this exercise. Work out three times a day.
- Toe raise
It mostly works the lower leg muscles, particularly the tibialis anterior, which is found on the outside of the tibia, or even the shin. This muscle is responsible for extending the toes and stretching the foot upward. The patient should be instructed by the therapist to aggressively raise their toes as far as they can. Do this ten times in a session. Work out three times a day.
Strengthening
- Single leg stands
Ankle eversion can also be effectively practiced by standing on one foot, which also tests ankle stability in general.
Starting out, the foot drop patient with sufficient strength and balance can attempt to stand for 10 seconds at a time on their damaged leg. To prevent the patient from falling, make sure you maintain stability by holding onto the chair’s back. Skip this step because patients who have foot drop are more likely to fall. Ten times during a session, do it. Conduct three sessions per day.
- Toe-to-heel rocks
Place yourself in front of the patient’s sturdy support system, such as a chair, table, wall, or other item. Lift your weight forward and raise yourself onto your toes. For 10 seconds, maintain this posture. Then, by returning the weight to the heels, lift the toes off the ground. Hold on for a full minute. Ten times for each session, repeat the process. Work out three times a day.
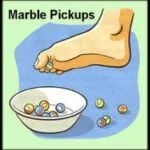
- Marble Pickup
The patient should be instructed by the therapist to sit on the chair with both feet flat on the floor. Put a container of twenty marbles on the ground in front of the patient. Pick up each stone with the damaged foot’s toes and drop it into a container. Continue until all the marbles have been collected by the patient.
- Ball lift
Sit on the chair with both feet flat on the floor to start. The little, spherical object—roughly the size of a tennis ball—should be placed on the ground in front of the patient. Extend your legs to hold an item between your feet and lift it slowly. Hold for 10 seconds before lowering gradually. Ten repetitions are required for each session. Work out three times a day.
- Toe raise, point, and curl
There are three primary steps to this exercise, which will help strengthen the toes and the entire foot.
To carry out this task: Sit up straight on the chair, keeping your feet flat on the floor. Next, elevate the heels while maintaining the toes on the ground. When the soles of your feet are still on the ground, halt. Ten seconds of holding it, then drop the heels.
In order to reach the second level, point your toes and elevate your heels until just the tips of your big and second toes are in contact with the floor. Ten seconds should pass before bending.
In order to achieve the third stage, curl your toes inward and elevate your heels until just the tips of your toes are in contact with the ground. Hold it for 10 seconds. In a single session, perform each step ten times to increase your range of motion and flexibility. In one day, complete three sessions.
- Toe splay
The toe splay exercise can help you have better control over your toe muscles. People can perform it simultaneously on both feet or alternately, primarily based on which foot the patient finds more comfortable.
To carry out this task: First, take a seat in the chair with a straight back and place your feet lightly on the floor. Next, stretch your toes apart as widely as you can without exerting yourself. For 10 seconds, maintain this posture. Ten times throughout each session, repeat this motion. Work out three times a day. After gaining more strength, the user can attempt wrapping the rubber band around his or her toes. This will increase the exercise’s difficulty and supply resistance.
- Toe curls
Performing toe curls increases strength overall and strengthens the flexor muscles in the feet and toes.
In order to complete this exercise:
Sitting upright on the chair with your feet flat on the floor is the proper position to begin. With the short side opposite the feet, place a little towel on the ground in front of the body after that. Put one foot on the short side of the towel next, then try to put the towel between your toes and pull it inward toward you. For each session, do it ten times. Three sessions should be completed each day. Using the object to weigh down the other end of the towel might increase the challenge of the workout.
- Sand walking
The greatest approach to strengthen and extend your legs and feet is to go barefoot on the beach. Because walking becomes more difficult for the body due to the softness of the sand, this is the best workout overall.
To carry out this task:
Go to the beach, the desert, a volleyball field, or any other place with sand to start. Take off your socks and shoes. Stride as far as you can. To prevent overusing your calves and foot muscles, try increasing the distance gradually over time.
- Golf ball roll
Plantar fasciitis pain can be reduced and discomfort in the arch can be relieved by rolling a golf ball beneath the foot.
To carry out this task:
First, take a straight seat on the chair with your feet flat on the floor. The golf ball or another tiny, hardball should then be placed on the ground close to the feet. Next, place one foot on a ball and roll it around, applying as much pressure as feels comfortable. Go on for 10 more seconds. If the ball isn’t acceptable, a frozen water bottle might be a calming substitute.
- Seated ball lift
First, instruct the patient to sit with their feet flat on the floor on the chair. Next, place a small ball—a tennis ball, for example—on the ground in front of the patient. To lift the ball, carefully stretch your legs and hold it with both hands. After 10 seconds of holding, return to the floor. Ten repetitions are required for each session. Work out three times a day.
- Toe-to-heel rocks
To get onto your toes, push your weight forward and hold the posture for ten seconds. Next, raise your toes off the ground and rock the weight backward while holding the position for 10 seconds. Ten times a session, repeat. Work out three times a day. The patient can perform this task while standing on one leg for an added difficulty. In order to allow the physical therapist to hold on for more support, the patient could want to perform it next to the wall, with a chair, or in front of a counter.
- Dorsiflexors strengthen with the band
First, the patient is instructed by the therapist to sit in a chair and wrap the theraband around a heavy table or other sturdy object that won’t move. Next, the patient extends their lower leg and the therapist instructs them to wrap the other end of a band around the top of their foot. Next, perform a foot flexion exercise while using the theraband to reverse the movement. In a single session, repeat ten times.
- Investors strengthen with the use of the band
First, wrap the affected foot with a band around the leg of the chair or the table. Next, use the remaining band end to make a circle around the inside of the injured foot. The therapist then gives the patient instructions before attempting to flip the foot inside. Do it ten times in a session. Spend three times each day working out.
- Everson strengthening exercise with the use of the band
The therapist instructs the patient to start by finding a comfortable posture, such as sitting on the chair, and then tying a theraband to the chair leg across from the affected foot. Next, wrap the wounded foot’s outside with one more end. When a patient tries to turn their foot outdoors, a physical therapist should give them an order. Ten times throughout a session, repeat it. Work out three times a day.
Gait Training
One’s gait is indicative of their walking style. The departure from typical walking is known as a gait anomaly.
Patients with major gait issues are the main ones for when gait training is advised. Through the use of various strength and balance exercises, this therapy helps the patient walk more effectively and improves stability. To be able to keep a patient safe during gait training, walkers, canes, and parallel bars may occasionally be needed. The assistive technology that helps the patient stay balanced during exercising is called a gait belt.
Home exercise
- At-home passive dorsiflexion using a belt or towel
A physical therapist will first instruct a patient to sit with their leg extended and their knee straight. Then, round the ball of the foot with the belt or cloth. Next, bring the foot toward the face by pulling back with a towel as the clinician holds either end of the towel in their hands. The patient’s hamstring and calf muscles should feel stretched. Perform ten rounds in a session. Perform two at-home workouts per day.
- At-home passive ankle inversion using a towel or belt
First, the patient is instructed by a doctor to sit with their leg extended and their knee straight. After holding the ends of the towel in the patient’s hands, wrap the belt or towel over the ball of the foot and gently slide the foot inside. Ten times in a single session, do it.
- Passive ankle eversion with the use of a towel or belt at home
A physical therapist will first instruct a patient to sit with their leg extended and their knee straight. Next, wrap the belt or towel over the ball of the foot, hold both ends in the hands of a physical therapist, and then gently push the foot outward. Ten times in a single session, do it. Conduct three sessions per day.
- Passive plantar flexion with the use of a towel or belt at home
The patient is instructed by the therapist to sit with their leg extended and their knee straight before starting. Next, wrap a football with a belt or cloth. Next, lift the foot toward the face by pulling back with a towel as a physical therapist holds either end of the towel in their hands. Both the calf and the hamstring muscles should feel stretched by this treatment. In one session, perform 10 repetitions. Work out twice a day at home.
- At home, passive toe extension against the step
Start by placing your toes on the wall’s base or placing your heel on the ground. Next, drive the toes back towards the tibia’s shin by gently leaning against a wall; however, do not maintain this posture. Ten times in a single session, do it. Work out three times a day.
Prognosis
The degree of the damage and the underlying diagnosis both affect the prognosis.
The best prognosis is for neuropraxia, and recovery often takes three months.
Recovery from axonal loss takes six to twelve months. The prognosis for neurotmesis is unclear, and surgery may be necessary to treat it with a tendon or nerve transplant. It is best to consult a peripheral nerve surgeon six to nine months following the damage. After eighteen months, the denervated muscle does not regain much function.
In situations when there are other causes, such as Lou Gehrig’s disease or lesions occupying space, the outcome will vary and be determined by the diagnosis rather than the involvement of peripheral nerves.
Complications
Braces and gait aids can cause complications, or the injury itself may cause complications.
Nerve injury causing foot drop makes it difficult to clear the ground, which can lead to a fall. Walking sticks and canes can sometimes be a hindrance, particularly on uneven terrain, therefore gait aids are helpful. Ulcerations can arise from anesthetic skin.
Braces that fit poorly might cause abrasions. Depending on how the mass changes, bracing might need to be adjusted. Different bracing may need to be supplied for different phases of edema and swelling in instances such as renal failure and congestive heart failure.
Deterrence and Patient Education
A good outcome requires the patient to be included at every stage of the decision-making process. It is important to educate the patient and their family members on the pathology, etiology, diagnosis, and severity of the illness process. Documents and detailed instructions pertaining to skincare, brace maintenance, and at-home workout regimens should be provided.
To keep effective braces, a doctor must be able to get in touch with the orthopedist in between appointments. This is because all braces ultimately need to be replaced and maintained. It is important to give follow-up instructions so that any modifications to treatment, bracing, or other diagnostic tests in the future may be maintained.
Braces or splints or AFO (Ankle foot Orthosis)

- The foot or splint that fits inside the shoe, together with the ankle brace, may aid in maintaining the foot’s natural posture.
- Splinting
- Splints are one method of improving function while a foot drop recovers. To maintain the foot in plantar grade, one may utilize a foot-up splint or solid ankle-foot orthoses (AFO). Because the toes do not catch on the ground, this helps to enhance the amount of dorsiflexion the foot maintains in during steps and can reduce falls.
- Specialized shoes
- Wearing shoes with spring-loaded bracing can help keep the foot from falling as you walk. A particular style pulls the foot up when walking by using a cuff around the ankle, a spring above, and a hook in the shoelace region that attaches to the spring.
- Ankle-foot orthoses (AFOs)
- These particular orthosis types are L-shaped ankle splint specialists. To prevent the foot from dropping, it just keeps it at a 90-degree angle to the lower leg. Wearing the foot support brace that helps the patient elevate their foot is an easy and affordable solution for solving these problems.
- Dorsiflexions help in ankle-foot orthotics (AFOs), which are available in a variety of designs. These include heavier foot-drop shoes that may be worn at night, soft foot-drop braces that can be worn even while the patient is without shoes, and posterior leaf spring (PLS) AFOs made of plastic or even lightweight carbon fibers.
- The soft foot drop brace, which the patient can wear with shoes or without, is one of the best-selling items. Ankle-foot orthoses (AFOs) made of plastic or carbon fiber are often criticized for their tendency to break down into the leg or foot and for being too bulky to be used with certain types of jeans and shoes.
Conclusion
It might be worrying if you can’t manage your foot as well as you once used. The good news is that drop foot may be treated entirely and is often a short-term condition. If you have weakness in your foot or find it difficult to walk, consult a medical professional. After ordering tests to determine the reason, you and the doctor will decide on a course of therapy.
FAQ
What is the main cause of foot drop?
Compression of a nerve in the leg that regulates the muscles used to raise the foot is the most frequent cause of foot drop.
Can foot drop be cured?
The cause of foot drop determines how to treat it. Foot drops can sometimes be cured by addressing the underlying reason. Foot drops cannot go away if the underlying cause is a persistent or long-term disease. Physical and occupational therapy may be advantageous for certain individuals.
Which medicine is best for foot drop?
Amitriptyline, nortriptyline, duloxextine, pregabalin, and gabapentin are among the other therapies.. Local treatment with transdermal capsaicin or diclofenac can also reduce symptoms. Even if there is significant pain, narcotic medications should be kept to a minimum.
Which nerve causes foot drop?
Foot drop is a gait abnormality brought on by peroneal nerve injuries. These symptoms might include numbness, tingling, discomfort, and weakness.
Is foot drop permanent?
You might have a temporary or permanent foot drop. One aid for keeping the foot in place is a brace. Foot drop treatment is based on the underlying reason. If the underlying reason is properly resolved, foot drop may become better or even go away.
How long is the recovery for foot drop?
The state of your general health and underlying issues will determine how quickly you recover. Within three to four months, patients often regain full use of their feet and resume their regular daily activities. Physical therapy is something your doctor may suggest as part of your recovery strategy.
What is the success rate of foot drop surgery?
In our investigation, we discovered that 88% of patients had recovered, with 61% of them achieving a full recovery. This was in line with previous research that indicated recovery rates ranging from 61% to 84%.



4 Comments