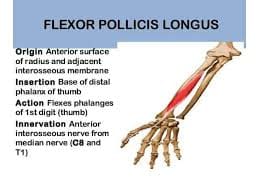
Flexor Pollicis Longus Muscle
What Is The Flexor pollicis longus Muscle?
In the anterior compartment of the forearm, the flexor pollicis longus (FPL) is a long muscle situated at the deep layer with the flexor digitorum profundus and pronator quadratus. Despite being located in the forearm, it is considered a component of the hand’s extrinsic muscles because it is involved in thumb movement.
Structure Of Flexor pollicis longus muscle
The thumb’s major flexor, the FPL muscle, flexes the interphalangeal (IP) and metacarpophalangeal (MCP) joints. Additionally, FPL has minimal effect on radial wrist rotation and wrist flexion.
FPL forms on the volar aspect of the radius and the surrounding interosseous membrane, directly distal to the radial tuberosity. Its proximal attachment is located distal to the supinator muscle and deep and radially to the flexor digitorum superficialis (FDS) radial head. The muscle tapers into a long, flat muscle that comes straight lateral to the FDS index finger and superficial to the pronator quadratus muscle.
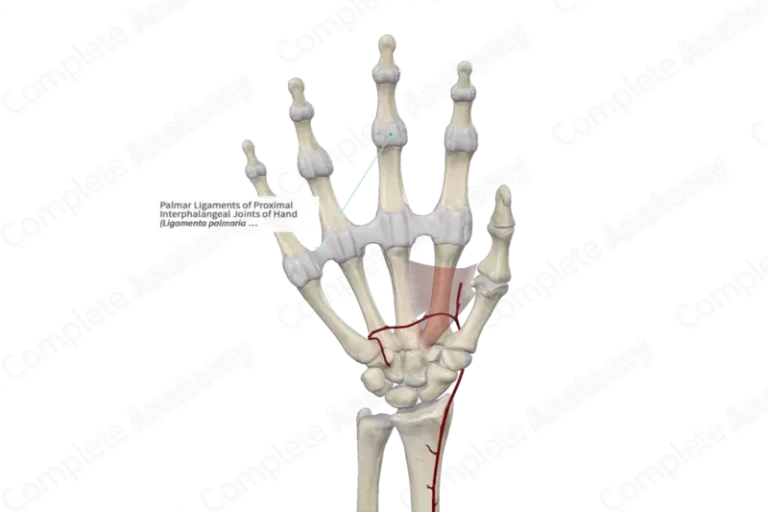
Now covered in the radial bursa’s synovial sheath, the FPL muscle passes deep into the transverse carpal ligament, or flexor retinaculum, as it passes into the carpal tunnel. Between the two sesamoid bones on the volar face of the thumb MCP joint, FPL continues along the first metacarpal.
Function Of Flexor pollicis longus muscle
The main function of the flexor pollicis longus is to flex the thumb at the interphalangeal joint. The flexor pollicis longus is critical for activities requiring hand grasping since it is the only muscle capable of bending the thumb’s interphalangeal joint.
In addition to flexing the thumb at the metacarpophalangeal joint, the flexor pollicis longus aids with wrist flexion. This muscle in the bottom layer of your forearm is easily felt when you flex your thumb. muscles three circular ligaments (A1, Av, and A2), and one oblique ligament form up the thumb’s flexor pulley system.
Ligaments are positioned proximally to distally in the form of A1, Av, oblique, and A2. The oblique ligament is the main pulley of the FPL muscle. Damage to the A1 and oblique ligaments will cause the FPL muscle to the bowstring. In 7% of cases, there is no AV ligament. A malfunctioning excursion of the FPL muscle through the pulley system is the cause of the trigger thumb.
Origin
It originates from the central region of the radius’s front surface and the corresponding section of the interosseous membrane. Furthermore, it has been found that the flexor digitorium superficialis, the medial epicondyle of the humerus, and the coronoid process of the Ulna are the origins of FPL.
According to a study by Ballesteros et al. the flexor digitorium superficialis accounts for 47.1% of the auxiliary head of FPL, the epicondyle of the humerus for 29.4%, and the coronoid process of the Ulna in the forearm for 23.5% of the muscle. According to Hemmady et al. of the 66.6% accessory head of FPL discovered, 16.6% comes from the ulna’s coronoid process and 55.5% from the medial epicondyle of the humerus.
Insertion
Forming a flattened big muscle, the muscle attaches at the base of the distal phalanx after passing through the carpal tunnel and three hand joints.
Nerve Supply
The FPL muscle is innervated by the anterior interosseous nerve (AIN), a branch of the median nerve. The anterolateral segment of the median nerve provides the origin of the AIN just proximal to the point where the nerve crosses over the two heads of the pronator teres muscle. The AIN flows distally with the anterior interosseous artery at the interosseous membrane that separates the FPL and FDP. The three deep flexors innervated by the AIN are the pronator quadratus, FPL, and FDP. The volar wrist capsule receives sensory innervation from the AIN as well.
Actions
When the thumb is fixed, the flexor pollicis longus, a flexor of the thumb’s phalanges, helps to flex the wrist.
Blood Supply
The common interosseous artery divides off as the ulnar artery passes beneath the teres minor muscle’s ulnar head. It goes laterally and profoundly before abruptly dividing into the anterior and posterior interosseous arteries. The anterior interosseous artery and anterior interosseous nerve (AIN) run distally along the interosseous membrane between the flexor pollicis longus and flexor digitorum profundus.
The pre-digital section of the FPL muscle receives its blood flow from branches of the median nerve artery. The connection V1 and V2 supply the digital component of the FPL muscle. V1 comes from either the Princeps pollicis artery or both digital arteries and is situated right proximal to the MCP joint. V2 is located near the IP intersection and is supplied by both digital arteries.
Lymphatic Drainage
The lymphatic drainage of the hand and forearm uses both superficial channels that run beside the basilic and cephalic veins and deep channels that run accompanying arteries. The lymphatics drain to lymph nodes inside the elbow, such as the cubital and epitrochlear lymph nodes, before mostly emptying into the axillary or infraclavicular lymph nodes.
Embryology
The three primary signaling centers area of polarizing activity (ZPA), nonridged ectoderm, and the tips ectodermal ridge (AER) cooperate to direct the formation of the appropriate developmental axis for the upper extremities. By the conclusion of the fourth week of embryonic development, four limb buds sprout from the ventrolateral surface of the growing embryo.
The cuboidal ectoderm that encloses somites and mesenchyme generated from the lateral plate dermis makes up the limb buds. The lateral plate mesoderm cells eventually continue to develop into the connective tissue of the extremities. The limb musculature originates from the paraxial dermis cells of the somites that have migrated into the limb buds. Muscle progenitor cells travel in a specific segmental pattern from somites.
The dermis layer at the distal tip of the growing limb gradually enlarges, causing the formation of the AER. While more proximal limb cells farther away from the AER start to develop into connective tissue and muscle cells, the AER causes nearby mesenchymal cells to stay undifferentiated to increase.
At the end of the sixth week of embryonic development, chondrocytes produce the fundamental structure of hyaline cartilage. This construct will eventually undergo endochondral ossification and will end in its ossification into the bones of the upper extremities.
Anatomical Variations
An auxiliary FPL muscle head might originate from the FDS muscle, the middle cortex of the humeral, or the coronoid process of the muscle of the ulna. The accessory head is eventually placed into the ulnar aspect of the FPL or FDP muscles. Many recent investigations have shown that Gantzer’s muscle, already believed to be an anatomical variation, is present in up to two-thirds of the population.
The Gantzer muscle has many clinical effects. The accessory head may compress the median nerve or AIN, based on its anatomical placement. When the AIN is squeezed, the pronator quadratus, FPL, and FDP might all exhibit symptoms ranging from weakness to paralysis. Most thenar and intrinsic hand muscles will become paralyzed in the case of median nerve compression, and sensory deficiencies will also result.
The Linburg-Comstock phenomenon is a persistent correlation between FPL and the FDP of the second digit. Because of this muscle slip, the thumb IP joint and the index finger distal interphalangeal joint cannot be flexed individually. But usually, this aberration does not result in the emergence of any symptoms.
Surgical Considerations
The most frequent causes of flexor muscle lacerations, including FPL, are blade, glass shard, or sharp metal cut injuries. Primary muscle repair is the entire reattachment of the damaged muscle.
Hand flexor muscle injuries are classified into many areas. The A1 pulley is connected to the carpometacarpal joint by T3, the A2 pulley to the A1 pulley, and the FPL muscle insertion to T2. These three locations begin distally in the thumb. In addition to treating digit muscle challenges, areas 4 and 5 include the region above the wrist.
Damage to the FPL muscle may result in a whole or partial laceration.
Treatments for partial flexor muscle lesions vary depending on the percentage of the muscle diameter that has been injured.
Nonoperative Management
- Damage to the FPL muscle may result in whole or partial tears.
Surgical repair indications
- More than 75–80% of the muscle has tears.
- More than half to sixty percent of the muscle has caused tears.
A complete FPL muscle tear may cause the proximal muscle to regress proximally, making muscle retrieval more difficult.
Primary muscle repair is an option for zone I injuries if the distal muscle stump measures more than 1 cm. To allow for proper healing, the proximal muscle has to be attached to the cancellous bone if the distal muscle stump is less than 1 cm. The connecting is done with button anchors or suture bases. Direct, end-to-end repair is used in the surgical management of areas II through V.
Many attached techniques are used to anastomose the two muscle ends. The amount of stitches placed inside the muscle is closely proportional to the muscle’s strength following surgery. To guarantee a solid bond and seamless passage through the flexor muscle pulley system, many strands of epi tendinous suture are employed in the most popular core suture repair approaches.
As of present, no research has created a multi-strand core suture technique that is universally accepted. The greatest risk of muscle re-rupture occurs in the first two weeks after surgery. It has been shown that the range of motion can be improved without significantly increasing the risk of re-rupture by employing a post-operative splint and early active mobilization.
Among the factors that can impact the outcome of surgically mending an FPL muscle are the location of the injury, the length of time between the injury and operation, postoperative care, and the presence of muscle retraction.
A particular kind of FPL rupture known as a Mannerfelt’s lesion develops in the carpal tunnel as a result of chronic tendon deterioration. After the scaphoid moves volar, abrasion results in this progressive weakening. Mannerfelt’s injury is most commonly caused by rheumatoid arthritis. It is a chronic systemic inflammatory disease that usually causes chronic synovitis, which can lead to carpal dislocation.
The FPL muscle is the one that gets injured most frequently in the carpal tunnel because it is the most radial muscle. However, this could affect any or all of the muscles in the carpal tunnel. One way to differentiate patients with FPL rupture from those with trigger thumbs is by looking for passive thumb flexion rather than pushed IP joint flexion.
If the rupture is detected within four to six weeks muscle grafting may be used to repair the FPL muscle. If the problem is not fixed in that period, a muscle transfer is a necessary medical procedure because the muscle would experience myostatic contraction.
Clinical Significance
Trigger Thumb
From a medical perspective, the flexor pulley system is important since a trigger thumb can result from a pulley compressing the FPL muscle. The FPL muscle’s incapacity to pass through the pulley system smoothly is known as the trigger thumb. Mostly affecting the A1 pulley, pulley is a condition most usually brought on by tendinitis.
Activity modification, corticosteroid injections, NSAIDs, and splinting are the first lines of treatment for trigger thumb. Between 50% and 92% of patients respond well to these conservative therapy choices. 60% to 100% of patients who do not improve have their symptoms reduced once the issue pulley is surgically removed.
A crippling disease known as Volkmann’s contracture develops as a result of untreated acute compartment syndrome. Although it can happen in the leg, Volkmann’s contracture usually affects the forearm.
Acute compartment syndrome of the forearm is most commonly caused by fractures and severe soft tissue damage, such as those resulting from crush injuries. These wounds produce swelling and edema and may increase the intra-compartmental pressure significantly and prevent the compartmental tissues from receiving enough blood. Ischemia of the muscles and nerves follows, leading to necrosis in time. As the damaged tissue heals, the myofibroblasts in the granulation cells will contract, allowing the damaged tissue to contract.
First to suffer damage are the flexor digitorum profundus and FPL in the forearm. The characteristically flexed deformity of Volkmann’s contracture is explained by a significant shortening of these muscles due to fibrosis. Within six months of the initial injury, the abnormality will reach its final stage if treatment is not received, leaving the hand with minimal functionality.
Treatment of acute compartment syndrome and early diagnosis is crucial in preventing Volkmann’s contracture. The “Six Ps” system can help assess people with injuries that increase their chance of developing compartment syndrome.
- extreme discomfort during a physical examination; discomfort when the afflicted compartment is passively stretched.
- Paresthesia
- Paresis
- Pallor
- Pulselessness
- Poikilothermia
Even though a clinical diagnosis of compartment syndrome is typically made, depending on the patient’s cognitive state, it is occasionally possible to diagnose the condition by measuring the intra-compartmental pressure. If there is a difference between the intra-compartmental pressure and diastolic blood pressure of less than 30 mm Hg, revascularization and an urgent open fasciotomy are required.
If left untreated, acute compartment syndrome results in nerve ischemia in 30 minutes and attached damage within 12 hours. The first four hours will experience a decrease in muscular function, and the following six to twelve hours will see long-term muscle decline.
Two systems are used to classify Volkmann’s contracture: the Seddon classification system (Grades I–III based on contracture severity) and the Tsuge classification system (Mild, Moderate, and Severe based on muscles and nerve involvement as well as presentation). For mild to grade I contractures, conservative therapy with splinting and stretching is the first line of treatment Surgery is not required for moderate or severe contractures, but it is possible for mild contractures. Surgical interventions include muscle slides, free functional muscle transfers, and lengthening.
Assessment
To test the flexor pollicis longus, the distal phalanx of the thumb is flexed against resistance while the proximal phalanx is maintained inactive.
Exercises of Flexor Pollicis Longus Muscle
Stretching Exercise
Extensor Stretch

- Stretch out one arm straight from the elbow.
- Grip it at the side of the thumb with the other hand, then bend the wrist downward.
- Give the stretch a 20–30-second hold.
Flexor Stretch

- With your elbow straight in the afflicted arm, hold the palm of one hand with the other.
- Gently draw your hand back to get a forearm stretch.
- Give the stretch a 20–30-second hold.
Strengthening Exercise
Wrist flexion:
- While seated, rest your forearm on the table with your wrist hanging over its edge.
- Flex your wrist to raise the weight or draw the resistance band closer to your body while you hold a lightweight resistance band in your hand.
- Return the weight or band to its original position slowly, then repeat a few times.
Thumb flexion:
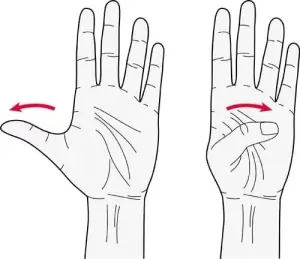
- When seated at a surface, place your palm downward and rest your forearm on the surface.
- Put something little on the table, like a coin, and use your thumb to pick it up and bring it to your palm.
- Release the object gradually, then repeat a few times.
Finger walks

- Spread your fingers wide and place your hand down on a table.
- One finger at a time, slowly extend your fingers forward until your fingers are gathered into a fist.
- After that, carefully extend your fingers once more. Repeat many times.
Grip strengthening

- Squeeze a softball or grip strengthener for a moment before releasing your hold.
- Repeat many times.
Pinch grip exercise
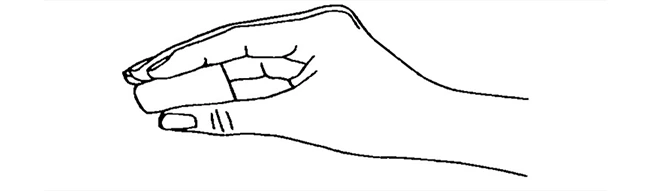
- Using your thumb and fingers, hold a small object between them, like a ball or a pen.
- After a few seconds of firm pressure, release the object.
- Do this ten to fifteen times.
Fingertip push-ups
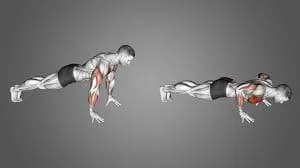
- With your torso straight and your weight evenly distributed over your toes and fingertips, begin in the push-up position.
- Bending your elbows, slowly drop your body toward the ground.
- Try to raise yourself back with the tips of your fingers, not your palms, as you push yourself up.
- Do this ten to fifteen times.
Conclusion
The flexor pollicis longus, or FPL, is the main forearm muscle tasked with bending the thumb. It enters the base of the thumb’s distal phalanx from the middle third of the front surface of the radius and the nearby interosseous membrane.
The thumb muscle is necessary for numerous daily tasks that include thumb movements, such as pinching, gripping, and grasping. Because it passes through the carpal tunnel alongside the median nerve, its muscle compresses in conditions such as carpal tunnel syndrome.
FAQ
What is the purpose of the longus flexor pollicis?
The main function of the flexor pollicis longus is to flex the thumb at the interphalangeal joint. The flexor pollicis longus is crucial for activities requiring hand grasping since it is the only muscle capable of bending the thumb’s interphalangeal joint.
What nerve Innervates the flexor pollicis longus?
The FPL muscle is innervated by the anterior interosseous nerve (AIN), a branch of the median nerve. The anterolateral segment of the median nerve provides the origin of the AIN just proximal to the point where the nerve crosses over the two heads of the pronator teres muscle.
What is the action of the pollicis longus?
The thumb’s terminal phalanx is extended by the extensor pollicis longus. The thumb’s interphalangeal joint can be extended to its neutral position by the abductor pollicis brevis and adductor pollicis, which both attach to the extensor pollicis longus muscle.
Is flexor pollicis longus a thenar muscle?
Three small muscles on the hand’s lateral (radial) portion cosmetics the thenar muscles. These muscles are the opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis.
What type is flexor pollicis longus?
In the anterior compartment of the forearm, the flexor pollicis longus (FPL) is a long muscle situated at the deep layer with the flexor digitorum profundus and pronator quadratus. Despite being located in the forearm, it is categorized as an extrinsic hand muscle because it participates in thumb movement.
How do you treat flexor pollicis longus?
The preferred course of treatment for Flexor Pollicis Longus (FPL) injuries is primary repair with end-to-end sutures. muscle transfer and grafting are performed when primary repair is impossible; each procedure has advantages and disadvantages.
Where do you palpate the flexor pollicis longus?
Simply place your palpating finger pads on the radial side of the anterior, distal forearm and ask the patient to bend their thumb’s distal phalanx at the interphalangeal joint to palpate this muscle.
What is a flexor pollicis longus symptoms?
An injury to the flexor pollicis longus may manifest as noticeable thumb weakness, localized discomfort, or a reduction in thumb range of motion. The flexor pollicis longus muscle becomes inflamed, leading to the excruciating disease known as trigger thumb.
What is the muscle attachment of the flexor pollicis longus?
The flexor pollicis longus is a muscle located in the deep compartment of the front forearms. This attachment: Originates from the interosseous membrane that covers the radius’s anterior surface. The muscle exits the carpal tunnel and joins at the tip of the thumb’s distal phalanx.
How do you heal abductor pollicis longus pain?
Heat or cold packs. Myofascial relaxation of the muscle and stretching are part of manual therapy. the type of activity recommended for long-term conditions. Taping, medication, and thumb splinting (thumb spica) can be utilized for intense pain and severe conditions.
How do you identify flexor pollicis longus?
One of the muscles of the deep anterior compartment of the forearm is the flexor pollicis longus. This kind of skeletal muscle is called unipennate. Its muscle leaves the wrist and goes deep into the hand’s flexor retinaculum, where it enters the tendinous sheath of the flexor pollicis longus.
References:
- Flexor pollicis longus muscle. (2024, January 4). In Wikipedia. https://en.wikipedia.org/wiki/Flexor_pollicis_longus_muscle
- Flexor Pollicis Longus. (n.d.). Physiopedia. https://www.physio-pedia.com/Flexor_Pollicis_Longus
- Benson, D. C., Miao, K. H., & Varacallo, M. (2023, July 24). Anatomy, Shoulder and Upper Limb, Hand Flexor Pollicis LongusMuscle. StatPearls – NCBI Bookshelf.
- https://www.ncbi.nlm.nih.gov/books/NBK538490/
- Flexor pollicis longus muscle. (2023, October 30). Kenhub.



One Comment