“Dancer’s heel,” also called “dancer’s tendinitis,” is a condition that mainly affects people who do activities like dancing and athletics that require them to use their foot and ankle muscles excessively or repeatedly.
Pain and discomfort in the back of the heel, especially in the area around the Achilles tendon and the surrounding tissues, are the main characteristics of this condition.
What is a Dancer’s Heel?
Dancer’s heel is a foot condition that develops when the tissues at the back of the ankle are compressed. As the name suggests, this is usually seen in dancers who frequently place massive pressure on their heels with their dance moves. The ankle is one of the most frequently injured sites of the body when dancing.
Flexor Hallucis Longus tendonitis, or dancer’s tendinitis, is an overuse injury caused by repeated bending of the plantar joints. Dorsal flexion, or pointing and flexion, of the foot, is the cause of FHL tendinitis. FHL injuries in dancers are frequently caused by repetitive motions from hunching over to standing up.
Because of its capacity to regulate pronation and supination between the feet as well as its physiological and mechanical characteristics that allow it to act as a powerful transducer from the back of the foot to the big toe, Flexor Hallucis Longus (FHL) is also referred to as the “Achilles of the foot.” Due to its remarkable anatomical structure and function, the muscle-tendon unit frequently gets injured in athletes.
Anatomy
Flexor Hallucis Longus (FHL)
- The interosseous membrane of the leg, the intermuscular wall, and the posterior and distal two-thirds of the fibula are the origins of FHL.
- It is situated deep within the soleus and leg muscles, as well as distal and lateral to the ventral side of the flexor long finger (FDL). It is pennant-shaped, so the muscle fibers elongate and converge toward its tendon as it passes through the back of the lower tibia.
- It forms a transverse cortical bone above the calcaneus muscle and exists beneath it because it rotates towards the arch.
- It follows that the FHL is situated behind the vascular bundle and is a component of the tarsal tunnel.
- Hallucis Longus passes through the foot arch. This is called “Henry’s Knot”. “. Dorsally on the medial edge of the plantar fascia is where the FHL is located.
- Thus, the FHL binds to three retinal structures (at the level of the tarsal tunnel, Henry’s node, and the intervertebral ligament) and tension on the tendon that may result in damage.
- When dancers don’t follow the joint’s natural movement requirements, FHL injuries happen.
- Increased bone load, overuse syndrome risk, and bone misalignment may arise from this.
- Because the ankle and foot bear a lot of weight and the soft tissue must compress them enough to maintain their position and reduce the risk of damage, these actions put a lot of strain on those bones.
Heel bone (calcaneus):
The major bone of the foot is located posterior to the foot and forms the bottom of the heel.
Growth plate (epiphysis):
This is the area of cartilaginous tissue at the end of the bone that grows new bone. Dancers’ heels affect the heel bone’s growth plate.
Achilles tendon:
The calf muscle and the back of the heel bone are joined by this strong tendon.
- The calf muscles and Achilles tendon could tighten up during periods of rapid growth, which increases the strain on the growth plate located behind the heel.
- This may induce inflammation and aches in the area.
- Sufficient rest, stretching, and good footwear are mostly recommended to manage the condition and relieve symptoms.
- If you are concerned, it is important to consult your physician for an accurate diagnosis and therapy advice.
Epidemiology of dancer’s heel
Heel epiphysitis, also known as dancer tendonitis, is a more common condition in young athletes and active young people. It usually impacts children between the ages of 8 and 14, usually during the growth period that occurs in adolescence. The following are a few important facts about the prevalence of tendinitis in dancers:
Age:
Dancer tendonitis primarily affects girls aged 10 to 12 and boys aged 12 to 14, with an average age range of 8 to 14 years. This is by the time of active growth plates and rapid bone formation.
Gender:
The boys are more prone to affect than girls due to their growth spurt a little later than girls.
Activity level:
Young athletes and active people who perform running and jumping sports like basketball, gymnastics, dance, and soccer are prone to the condition.
Risk factor:
Significant risk factors include tight calf muscles, fast growth, and intense exercise that puts strain on the growth plate and heel bone.
Prevalence:
Tendonitis is one of the most common causes of heel pain in children and adolescents, even though the precise prevalence of the condition varies among dancers.
Self-limitation:
A condition called dancer tendonitis typically goes away on its own. Symptoms usually get better and eventually go away as growth slows down and growth plates close.
It’s essential to understand that, even though its sometimes severity and duration, dancers’ tendonitis is not a serious or chronic illness. A speedy recovery can be assured and symptoms can be relieved with appropriate management, which includes rest, appropriate footwear, stretching, and sometimes physical therapy. A doctor should be consulted for an accurate diagnosis and advice if your child has severe or persistent heel pain.
Causes of Dancer’s Heel
Severe disorder, also known as calcaneal spondylitis, is mainly induced by repetitious stress and pressure put on the growth plate of the heel bone (calcaneus) during a period of rapid growth. many factors contribute to the development of dancer’s tendonitis
Rapid growth :
Muscles and tendons tighten during the growth phase because bones typically grow more quickly than these soft tissues. Increased pressure on the growth plate may result from an imbalance between the growth of bones and the flexibility of soft tissues.
Muscle and tendon strains:
Achilles tendonitis and tight calf muscles can increase growth plate pressure. The bone may not have been stretched sufficiently or it may have grown too quickly to account for the tightness.
High-impact activities:
High-impact exercises like jumping, running, and other physical activities can strain the growth plate more. Due to these movements, sports like football, basketball, gymnastics, and dance are often linked to tendonitis in dancers.
Unsuitable footwear:
Wrong or unsupportive shoes can contribute to the development of a dancer’s tendonitis. Shoes that don’t provide arch support or good cushioning can relieve stress on the heel region.
Biomechanical factors:
The risk of developing a dancer’s disease can be raised by abnormal foot mechanics, such as spending too much (excessive rolling inward of the foot) or high arches of the foot.
Excessive activity:
This condition may be worsened by vigorous exercise without adequate rest. The soft tissues are unable to sufficiently adapt and recover from overtraining and insufficient rest periods. On the other hand, it happens during growth spurts and is more prevalent in young, active people who play high-impact sports.
Symptoms of Dancer’s Heel
This disease is characterized by a variety of symptoms, especially involving pain and discomfort in the heel. Common symptoms of dancer’s tendonitis include:
Heel pain:
The main symptom is pain in the posterior to the heel, usually felt where the Achilles tendon attaches to the heel bone. One way to characterize the pain is as a throbbing or dull aching.
Limping:
The kid may limp a little or alter the way he walks to avoid placing pressure on the aching heel.
Discomfort during activity:
The pain is often more pronounced during or after physical activities that involve running, jumping, or impacts, such as playing sports or active play.
Morning stiffness:
When they wake up in the morning or after taking a nap, certain kids might feel pain and stiffness in their heels.
Redness and swelling:
In some cases, there may be little redness and swelling near the heel area.
Tenderness to touch:
The heel can be painful to touch or pressure.
Heel warmth:
Because of the inflammation in this area, the affected heel may feel warm to the touch.
- It’s essential to remember that dancer’s tendonitis is a temporary illness that frequently goes away on its own when a child’s growth plate closes and their bones cease growing quickly.
- To minimize discomfort and prevent it from getting worse, though, appropriate management is crucial.
- Your child should consult a medical professional, such as a pediatrician or sports medicine specialist if they show symptoms that could indicate Sever’s disease. This will help to confirm the diagnosis and provide the right guidance for treatment and symptom relief.
Differential diagnosis
When diagnosing a child with heel pain, it’s essential to rule out the possibility that the child has dancer’s tendonitis because several conditions can have symptoms that are similar to that of this condition. Dancer’s tendonitis can be mistaken for several conditions, including:
Plantar fasciitis:
The tissue that runs along the sole, known as the plantar fascia, is inflamed in this condition. Heel pain may result from it, particularly in the morning or following rest periods.
Achilles tendonitis:
Ankle pain in the back of the heel may be caused by Achilles tendinitis. Although it is more common in adults, active adolescents can also experience this condition.
Stress fracture:
There may be localized pain associated with a stress fracture of the heel or other metatarsal bone that gets better with rest and gets worse with movement.
Tarsal Coalition:
This is a congenital disorder in which two or more bones in the foot joint together abnormally, inducing pain and stiffness in the foot.
Calcaneal bursitis:
Pain and swelling in the back of the heel can be caused by bursitis, a fluid-filled sac.
Bone cysts or tumors:
Tumors or bone cysts in the heel region are rare, but they can cause localized pain.
Inflammatory conditions:
Joint pain and inflammation can be caused in the heels as well as other parts of the body by conditions such as juvenile idiopathic arthritis.
Proper examination by a medical professional, such as a pediatrician, orthopedist, or sports medicine specialist, is required for an accurate diagnosis and appropriate treatment. History, physical examination, and occasionally imaging studies (such as X-rays) can be used to distinguish a dancer’s heel from other possible reasons for heel pain.
Diagnosing a dancer’s heel
A medical history, physical examination, and occasionally imaging tests are used to diagnose Achilles tendonitis, also known as dancer’s tendinitis. The medical professional will start by inquiring about the child’s symptoms, including the onset of the pain, activities that make it worse or better, and any pertinent medical history.
Physical examination:
The doctor will perform a complete physical examination of the affected leg. They will consider the heel area for pain, edema, and warmth. They may also assess the person’s gait and foot mechanics to identify contributing factors.
Palpation:
The physician may gently press the back of the heel to evaluate tenderness in the growth plate and covering areas.
Range of Motion:
The provider may test the ankle and foot range of movement to assess for any limitations or abnormalities.
Image studies:
In most patients, imaging studies such as X-rays are not needed to analyze a dancer’s tendonitis because it is a clinical diagnosis. However, an X-ray may be ordered if the healthcare provider wants to rule out other possible reasons for heel pain, such as stress fractures or structural problems.
Positive Tomasen test:
- This test assesses the effect of the first movement MTP.
- This test was done by assessing the first MTP movement in both positions, i.e. maximal arch flexion and moderate dorsal ankle flexion.
- To conduct the test correctly, the first tarsal head must be stabilized to avoid compensatory flexion of the first tarsal head.
- A positive test is a discomfort or decreased extensibility of the first MTP joint 20 degrees with ankle reflex.
- When a therapist allows the person to release the foot directly flex the sole and point the foot out, they will have a better big-toe range of motion.
The physician will rule out diseases that resemble Dancer’s tendinitis and investigate different possible causes of heel pain. If the clinical findings are consistent with the clinical characteristics, the healthcare provider will diagnose the dancer’s disease based on information obtained from the medical history, physical examination, and any required imaging studies.
Medical treatment for Dancer’s Heel
The main goals of medical care for children with heel tendonitis, also known as dancer’s tendonitis, are to heal the injured area and manage their symptoms.
Here are a few typical methods of medical treatment:
Rest:
Resting the involved foot is important to give the inflamed growth plate time to recover. Lowering or avoiding movements that make pain exaggerated, such as running or jumping, can help with recovery.
Ice:
Using ice on the painful site for about 15 to 20 minutes every few hours can assist decrease inflammation and relieving pain.
Anti-inflammatory drugs:
Ibuprofen and other over-the-counter NSAIDs can help decrease pain and inflammation. However, their use should be under the guidance of a healthcare expert, especially in children.
Heel pads or orthotics:
Reducing pressure on the heel and enhancing foot mechanics can be achieved with the use of heel pads or customized orthopedic pads that offer arch support and cushioning.
Physical therapy:
Physiotherapists can provide exercises and techniques to address muscle imbalances, improve flexibility, and promote useful foot mechanics.
Activity modification:
Adjusting a child’s training level or changing their exercise training to avoid high-impact exercises can prevent further stimulation of the growth plate.
Suitable footwear:
Choosing supportive cushioning footwear with good arch support can assist relieve stress on the heel area. It is important to avoid shoes with reduced cushioning or inadequate support.
Gradual Return of activity:
Physical activity should be gradually resumed under the guidance of a medical professional once the pain goes away and the healing process grows.
Monitoring Growth:
When a child gets older the growth plates close and the child’s bones mature, the symptoms of the dancer’s tendinitis usually disappear. Routine examinations with a physician can ensure that the condition is progressing as expected.
Physical therapy treatment of dancer’s heel
Because every person’s condition is different, the physical therapy treatment plan will be specific according to their requirements. You should speak with a doctor if you’re thinking about physical therapy for a dancer’s heel to make sure that the plan of treatment is suitable for your condition and medical history. Here are some common physical therapy treatments for Dancer’s heel:
Conservative care for dancer’s tendonitis
Protocol
- Following protocol, especially with anti-inflammatory medications and frequent ice application, can help decrease inflammation significantly in the early stages of this disease.
- It is also necessary to follow the appropriate nutritional, dietary, and possibly pharmaceutical recommendations.
Stretching exercises:
A physiotherapist can guide children via specific stretches to enhance flexibility in the calf muscles and Achilles tendon. Gentle stretching can help reduce tightness and relieve stress on the growth plate. Stretching practices can help manage a dancer’s tendonitis by helping to relieve tension in the calf muscles and Achilles tendon, which can contribute to heel pain. Here are some stretching exercises that may be recommended:
Calf stretching against the wall:
Standing Calf Stretch

- begins with standing facing the wall with the hands relaxing on the wall at shoulder height.
- Step back with one foot and keep it straight, heel touching the floor.
- Flex the front knee while keeping the back leg straight and the heel touching the floor.
- Maintain the stretch for about thirty seconds, then do both sides.
On Stairs calf stretch:
Calf stretch off step
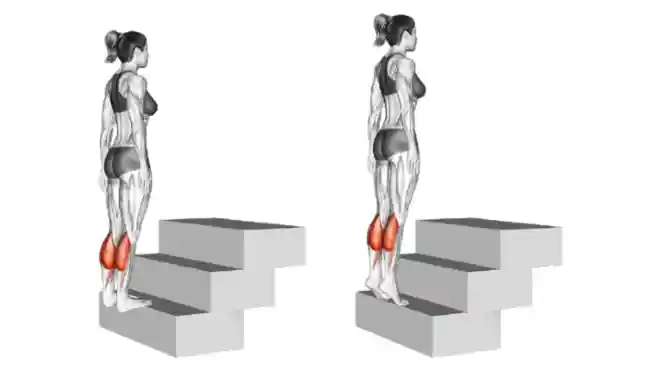
- Begin with standing on stairs or steadily increased surfaces with the soles of the feet relaxing on the step and heels hanging over the edge.
- slowly lower the heels to the bottom of the ladder to feel the stretch in your calf muscles.
- Hold the stretch for about thirty seconds.
Achilles stretch while sitting:
- Start with sitting on the ground with your legs stretched out in front of you.
- Wrap the soles of the feet in a towel or resistance band.
- To bring the toes closer to you, flex the ankle and gently pull on the bandage or towel.
- Maintain the stretch for about 30 seconds, then switch sides.
Toes raise on one step:
- Start by placing your heels over the side of a ladder and standing there.
- Slowly lower the heels below step level, feeling the stretch in the calf.
- raise the heels back to the start position.
- Do several repetitions of this exercise.
Ankle circles:
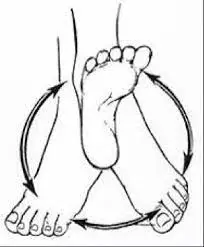
- Start with sitting in a chair or on the ground.
- Raise one foot off the ground and slowly rotate the ankle in clockwise and counterclockwise circles.
- Make several circles in both directions.
It is essential to consult a health care professional or physical therapist before beginning any new training routine, particularly if your child is experiencing pain. They can advise on appropriate stretches and make sure they are safe and useful for your child’s specific condition.
Strengthening exercises:
Strength workouts can target the appropriate mechanical support muscles of the foot. This includes activities for the calf muscles, as well as other leg muscles, to promote stability and balance.
Strength training helps promote proper foot mechanics and improve muscle balance, both of which can assist manage tendinitis in dancers. Here are some strength activities that may be advised:
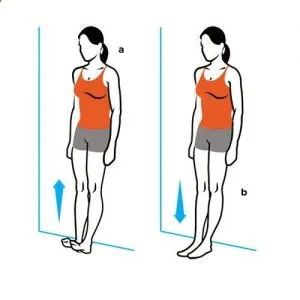
Toe raises:
- Begin with standing straight with your feet flat on the ground.
- Gradually raise your heels off the floor, placing your weight on your toes.
- Lower your heel to the ground.
- Do several repetitions of this exercise.
Calf raises:

- Begin with standing straight with your feet flat on the ground.
- now raise your heels off the ground.
- Gradually lower your heel to the ground.
- Do several repetitions of this exercise.
Heel drops on a step:
Bilateral heel drop
- Stand on the border of the step with the soles of your feet relaxing on the step and your heels slumping over the edge.
- Stand up on your toes.
- Do several repetitions of this exercise.
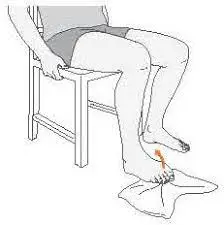
Ankle plantarflexion with resistance band:
Ankle planter flexion
- Seat in a chair with a resistance band covered around the ball of one foot.
- Grab the ends of the band and flex your ankles under the resistance of the band.
- Slowly release the tension and back to the initial position.
- Do several repetitions on both legs.
Single-leg balance:

Full Weight-Bearing Single Leg Stance
- Standing on one leg maintains your balance.
- Keep your abdominal engaged and your body steady.
- Maintain this position for about thirty seconds and then do it with the other legs.
Calf Raises on an Incline Surface:

- Stand on a little inclined surface (like a corner or a ramp), face up.
- Standing on your toes, raise your heels off the ground.
- Gradually lower your heel to the floor.
- Do 20 repetitions.
Towel scrunch with a heel lift:
Toe Curls with a Towel
- Put the towel on a smooth surface, such as tile or hardwood; put one foot on the towel.
- Actively begin rubbing the big toe ball under the toes.
- One by one, raise the heel of the towel (heel and big toe should be in flexion if done correctly).
- Put the heel back onto the towel and bend the big toe to begin the sequence again five times.
Marble/ ball pickups:
marble pickup
- Using the 1st and 2nd toes, flex your back to pick up the marble/ball and drop it into the cup/box by flexing the soles of your feet.
- Must be completed in a standing position.
Strengthens the gastrocnemius and soleus complex:
- From a standing position, complete a step raise by keeping one big toe on the outside of the step and pushing up into the step position.
- This exercise strengthens the gastrocnemius and soleus complex.
Remember that this activity should be performed in a painless range of movement. Begin with a controllable number of repetitions and slowly increase as your child’s strength improves. You should consult a healthcare professional or physiotherapist before beginning a new workout routine to ensure that the activities are suitable for your child’s condition and to prevent any serious signs.
Gait analysis:
A physical therapist can examine the child’s gait, or walking pattern, to look for any imbalances or anomalies that might be causing the problem. One way to lessen the strain on the heel is to mechanically modify one’s gait.
Manual therapy:
The affected area can benefit from improved blood circulation, lowered muscle tension, and increased wound healing when hands-on methods like massage and manual manipulation are used.
Dancers suffering from tendonitis can benefit from massage therapy and manual manipulation, which also helps to increase blood flow and release tense muscles. Here we explain some methods a medical professional or trained therapist can use:
Soft tissue massage:
A therapist will gently massage and apply pressure with their hands to the muscles surrounding the heels and calves. It helps release tight muscles, relieve muscle tension, and improve blood flow to the affected area.
Myofascial release:
- These techniques target the fascia, the connective tissue around the muscles, and additional structures.
- The therapist utilizes gentle pressure to stretch and remove constraints in the balance, which can contribute to muscle tension.
Active release technique (ART):
- ART is a process that affects a combination of movement and deep pressure to treat soft tissue constraints and adhesions.
- It is mainly used to break up scar tissue and enhance flexibility.
Joint mobilization:
- Joint mobility affects the therapist by gradually moving the joints of the foot and ankle through their natural range of motion.
- It can help improve joint mobility, reduce stiffness, and promote healing.
Trigger Point Therapy:
Trigger points are regions of muscle that are sensitive to the touch and can contribute to referred pain.\ Therapists apply force to these points to remove tension and relieve pain.
Heat therapy:
Heat can be used on the site before or after the massage to loosen muscles and enhance blood circulation.
- It is essential to note that these procedures must be completed by qualified medical professionals or therapists trained in these modalities.
- You have to consult a physician before beginning any manual therapy technique, particularly for children.
- They can help determine the right approach and ensure that therapy is appropriate for the child’s specific condition and requirements.
Orthotics prescription:
If required, a physiotherapist can advise and specify custom orthotics that deliver the right cushioning and arch support to help reduce discomfort.
Education and Activity Modification:
A physical therapist can inform parents and kids about the condition, appropriate footwear, and ways to modify activities to keep symptoms from getting worse.
FAQ
How do you cure a dancer’s heel?
Applying an ice pack can also help reduce swelling and may encourage a more rapid return to normal ankle movement. Your physician may suggest a steroid injection into the painful area, to help reduce irritation and swelling in the soft tissues that are being pinched, decreasing their tendency to get pinched.
What is dancers’ Sever’s disease?
It occurs when the tendon that connects to the posterior to the heel, called the Achilles tendon, pulls on the growth plate of the heel bone. This disease does not discriminate among genders. females usually experience symptoms from age 8 to 13, with males experiencing similar symptoms from age 10 to 15.
Are heel spurs typical among dancers?
Dancers usually have bone spurs on the talus. This can induce a posterior ankle bump at the back of the ankle. However, dancers are no better likely to have a typical heel under the foot than anyone else.
Can dancing induce heel pain?
Dancers who have more active training or class schedules frequently report having more heel pain. Furthermore, heel pain may be more common in en pointe dancers, or those who begin or perform more challenging sections. It should be noted, however, that not all dance forms cause heel pain.
Is heel pain relieved by walking?
You can improve your walking endurance and speed without aggravating your Achilles tendon by walking on flat ground.
References
- Thakkar, D. (2023b, August 19). Dancer’s Heel – Cause, symptoms, treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/dancers-heel/
- Dancer’s feet: Foot problems & their treatment | CK Birla Hospital. (2021, November 18). CK Birla Hospital. https://www.ckbhospital.com/blogs/foot-problems-in-dancers-and-treatment/

