Cheiralgia Paresthetica (Warternberg syndrome)
What is a Cheiralgia Paresthetica?
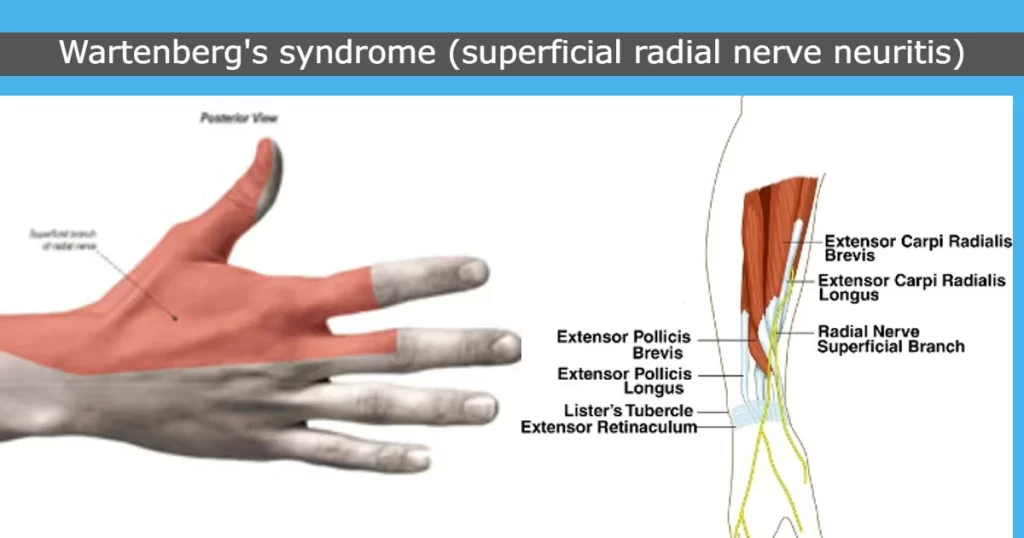
Cheiralgia Paresthetica also called Wartenberg Syndrome) is a condition that occurs mostly due to the compression or entrapment of the superficial branch of the radial nerve. This nerve, responsible for sensory functions in the back of the hand and thumb, can cause numbness, tingling, and pain on the radial (thumb) side of the wrist when compressed.
Warternberg syndrome, another name for Cheiralgia Paresthetica, is a compressive neuropathy. because of compression caused by the extensor carpi radialis longus (ECRL) and brachioradialis movements during forearm rotation, such as when turning a key. The disease comes and goes, causing prolonged periods of time possibly years without any complaints, occasionally broken up by one or more consecutive bouts. It’s regarded as a harmless disorder. Conservative therapies include rest, wrist splints, and, in certain situations, CSIs with surgical decompression.
Rarely, the incidence was less than 1 per 100,000 per year. The male-to-female ratio is 1:4, and women between the ages of 20 and 70 are thought to be more likely to have it.
Compression of the superficial branch of the radial nerve at the location where the nerve emerges from underneath the muscles results in Cheiralgia Paresthetica. Entrapment of the superficial branch of the radial nerve occurs at the lateral boundary between the brachioradialis and extensor carpi radialis longus muscles. The brachioradialis muscles rotate the nerve while closing the gap between these two muscle tendons in a scissor-like manner, causing entrapment when the forearm is repeatedly pronated. Forced pronation and wrist ulnar deviation exacerbate the pain.
Anatomy
Anatomy of the superficial radial nerve:
The radial nerve splits in the proximal forearm, and the superficial sensory branch of the radial nerve emerges between the brachioradialis and extensor carpi radialis longus (ECRL) to become superficial after traveling deep to the brachioradialis in the forearm muscle’s undersurface, about 9 cm proximal to the radial styloid.
The subcutaneous tissues still include the superficial radial nerve (SRN). It is in charge of transporting afferent sensory information from the dorsum of the thumb, index, and middle fingers proximal to the proximal interphalangeal joints. It also provides branches to dorsal digital nerves.
Branches:
- The distance between the dorsal branch and Lister’s tubercle is 1-3 cm. It provides the first and second web spaces.
- The palmar branch nourishes the dorsolateral thumb and crosses the extensor pollicis longus within 2 cm of the first dorsal region.
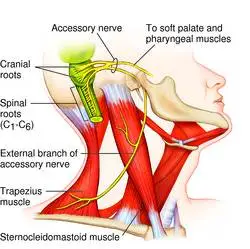
Roots of the radial nerves: T1, C5, C6, C7, and C8.
Pathophysiology:
Though the posterior border of the brachioradialis poses the greatest risk, the SRN can become stuck anywhere along its entire journey in the forearm. Trauma is also a common cause of superficial radial nerve compression, which can be caused by strain injuries to the nerve (e.g., closed reduction of a forearm fracture) or direct pressure on the nerve (e.g., by a bracelet or handcuff).
- Wartenberg’s symptoms and nerve injury are related to the force exerted on the nerve and the duration of its compression.
- Because of the compressive damage to the nerve’s myelin coating, microvasculature, or nerve itself.
- Axonal damage and ischemia may ensue from severe compression that obstructs blood flow.
Additionally, the length of compression has an alternative effect on the nerve:
1) Temporary reductions in blood flow may result from intermittent compression.
2) Prolonged compression causes blood flow to decline over time.
Demyelination, inflammation, scarring, fibrosis, and ultimately axonal degeneration can result from these long-term alterations. For a greater chance of healing, it must be removed before significant nerve damage has occurred. Recovery from nerve remyelination may take many weeks. Axonal regeneration is quite sluggish, though.
Cause of Cheiralgia Paresthetica:
Anywhere throughout its whole length, the radial nerve is squeezed. The nerve above the lateral wrist area may be compressed by tight handcuffs and wristwatches. Additionally, distal radius fracture pieces of soft tissue tumors (such as ganglion cysts or lipomas) might crush it. Iatrogenic injuries sustained during wrist arthroscopy surgery, external fixation implantation, internal fixation of distal radius fractures, and initial dorsal compartment release can also result in nerve damage.
Comparable techniques include radial arterial line removal, cannulation, cephalic venipuncture, and acupuncture. For de Quervain’s tenosynovitis, steroid injections are administered into the tendon sheath; however, this might harm the nerve itself by causing subcutaneous atrophy.
These two tendons run parallel to one another during forearm supination action, preventing compression of the nerve. However, the extensor carpi radialis longus compresses the nerve by crossing the brachioradialis muscle during pronation action.
Wartenberg’s syndrome also develops when diabetes mellitus is present in the body. In 20–50% of cases, this syndrome is also linked to De Quervain’s disease.
Signs and Symptoms of Cheiralgia Paresthetica:
- Both the dorsomedial hand and the proximal forearm are experiencing burning agony.
- Tingling sensation
- Numbness
- Hypoesthesia
- No, there is muscle weakness.
- Repetitive wrist flexion and ulnar deviation movements also aggravate the symptoms.
Signs:
- This usually happens when the intrinsic hand muscles weaken the ulnar nerve supply, namely the denervation of the nerve that supplies the palmar interosseus muscle to the little finger.
- Repeated wrist flexion, ulnar deviation, and pronation movement are tested provocatively.
Differential Diagnosis:
Although the pattern of symptoms may change due to anatomical variances, patients with SRN compression experience pain or dysesthesias on the dorsal radial forearm as well as pain spreading to the thumb and index finger.
Alternative diagnoses, such as a more proximal lesion or a tumor in the radial tunnel that affects both the PIN and SRN, may be considered by the doctor if the sensory problems occur concurrently with a weakening of the muscles that are supplied by the PIN. SRN entrapment symptoms might be mistaken for de Quervain’s tenosynovitis symptoms, such as wrist pain and ulnar deviation, as compression of the SRN frequently takes place in the first dorsal compartment region. The primary sign is whether or not there is SRN compression.
- De Quervain’s tenosynovitis:
- Unlike Wartenberg Syndrome, wrist pronation movement does not exacerbate pain in this disease.
- Lateral antebrachial cutaneous nerve (LACN) neuritis:
- Intersection syndrome:
- Dorsoradial forearm edema might be the result of this.
Exacerbation and “wet leather” crepitus during repetitive wrist flexion or extension movements are the symptoms. - Arthritis of the thumb carpometacarpal joint.
Diagnosis
Physical examination:
- provocative tests.
- Finkelstein test: The patient is instructed by the therapist to perform an ulnar deviation movement, which is a wrist movement that is upward, and to make a fist around the thumb. 96% of individuals had worsened symptoms according to this test.
- There are exterior compressions, scars, and masses.
- Skin changes.
Sensation:
- Light touch: This might not be typical.
- Two points Discrimination: In 80% of patients, this can be abnormal.
256 Hz vibration: This might be unusual.
Muscle Strength: There are no symptoms of atrophy or motor weakness. Perhaps there is less grip strength.
Special test:
- Hoffman Test: Determine the upper motor neuron dysfunction with the Hoffman Test.
- Dellon Test: Active, forceful forearm hyperpronation, wrist flexion, and ulnar deviation with the elbow out to the side.
- Wartenburg’s Compression Test for Neuritis.
- The Radial Nerve Compression Test’s Superficial Branch.
Optional Nerve Block Examination:
The superficial branch of the radial nerve is blocked by local anesthesia:
- The Finkelstein Test might turn out to be negative.
- Measured grip and pinch strength might be enhanced.
Imaging Examinations:
Radiography:
If the radial nerve becomes trapped in the arm, a radiographic examination should be done to look for any tumors, healed calluses, or fractures. Radiological studies provide proof for any ailment, including cancers, arthrosis, dislocations or instabilities, elbow or forearm fractures, and posterior interosseous nerve dysfunction.
Nerve Conduction Study:
It is employed to measure the affected nerve’s electrical activity and contrast it with typical levels.
It could be able to determine the location and kind of nerve damage in an inaccurate manner.
Ultrasonography:
It assists in determining the many reasons for wrist pain, such as de Quervain tenosynovitis, thumb joint arthritis, and cheiralgia paresthetica.
It can also be used to locate locations where nerves are compressed or trapped.
Plain Radiographs:
They aid in locating any orthopedic disorders or bony prominences.
Magnetic Resonance Imaging:
Any constriction or expansion of the bony portion can be seen in T1-weighted pictures.
Fat-suppressed density-weighted T2-weighted imaging can detect alterations in the nerve itself, such as augmentation and edema. Checking for aneurysms, ganglions, and lipomas is also beneficial.
Electromyography:
EMG aids in identifying the damaged region and tracking the time it takes for the nerves to heal. Three to six weeks following the injury, the EMG was negative. Nerve healing should be evident four months after the injury.
The abductor pollicis longus, extensor pollicis longus and brevis, and extensors indicis muscles will all exhibit abnormal function if just the lateral branch is squeezed. A localized compression site has normal function if the proximal portion is compressed, and abnormal function if the distal portion is compressed.
Treatment of Cheiralgia Paresthetica:
Medical Treatment:
Conservative Management:
- The primary treatment for this illness is conservative. Removing the tight item, like a bracelet or wristwatch, is a crucial part of nonsurgical treatment if external compression is the frequent underlying cause.
- Splinting,
- rest,
- Modification of nonsteroidal anti-inflammatory medication action.
In this disease, more individuals who receive nonoperative treatment have satisfactory to exceptional results.
Surgical management:
Surgical Decompression:
Between the brachioradialis and extensor carpi radialis longus, neurolysis and fascia band release occur:
Procedure:
To join the two muscles, draw a line. Determine the region of entrapment. Between the brachioradialis, which is located above, and the extensor carpi radialis longus, which is located below, the superficial branch of the radial nerve typically emerges.
A variety of adhesive barriers can be used to completely decompress the nerve. The barrier is cut to precisely fit the measured region of nerve compression. One might use the soft sterile dressing and continue with the multilayer closure.
Early range of motion should require postoperative care. Following surgery, physical rehabilitation should begin two weeks later. In order to lessen the creation of adhesions, desensitization, and scar massage around the scar region, it should support the early range of motion protocol and nerve gliding procedures. Following surgery, patients get treatment for four to six weeks and reach their full medical improvement sixty to ninety days later.
Physical therapy Treatment
- PNS, or peripheral nerve stimulation, is used to lessen pain.
- Electrical stimulation
- low-intensity infrared laser pulses.
- Ice massage
- Splint mobility exercises.
Peripheral nerve stimulation:
- applied to the pain location via TENS or nerve stimulation.
- Once a day, apply this stimulation for ten minutes.
Pulsed low-intensity infrared laser.
Splint:
- suggested that the patient wear a wrist splint to prevent jerky movements and to support their hand.
Electrical stimulation:
- Determine the muscle’s precise motor point first.
- given a galvanic current initially, followed by a gradually faradic current.
Mobility exercise:
- Less repetition is required for wrist ulnar and radial deviation as well as forearm pronation movement in this situation because the movement is limited or uncomfortable.
- The therapist encourages clients to sit comfortably in a chair with support for their forearms, create a fist, and twist their forearms back and forth. Do it five or seven times, then progressively more.
- The patient should next be instructed to do the wrist deviation action. Do it five or seven times, then progressively more.
- Perform this exercise without experiencing any pain.
Complications of Cheiralgia Paresthetica:
- Decompression surgery was unsuccessful.
- Chronic numbness and pain
- Dehiscence of wounds
- Infection
- Symptoms becoming worse
- damage to the suture’s surrounding tissue.
Prognosis
Cheiralgia paresthetica treatment results are encouraging. Patients frequently experience a spontaneous remission of their symptoms. According to estimates, up to 71% of patients who have nonoperative treatment experience satisfactory to exceptional results.
There have been conflicting findings on the effectiveness of surgical care following nonoperative therapeutic failure. While Calfee et al. report relatively moderate outcomes, with 55% of patients treated operatively still experiencing symptoms at a follow-up of 3.5 years, Lanzetta and Foucher observed a 74% success rate with surgical intervention.
According to Gaspar et al., a number of individuals who have basic nerve decompression treatment do not experience consistent outcomes. Compared to other peripheral neurolysis procedures, neurolysis for entrapment of the superficial branch of the radial nerve has worse results and higher recurrence rates.
FAQs
What is the radial nerve Wallenberg syndrome?
A particular mononeuropathy known as Wartenberg’s syndrome is caused by entrapment of the radial nerve’s superficial branch. Numbness, tingling, and weakness in the thumb’s back are among the symptoms. Cheiralgia paresthetica is another name for it.
In ENT, what is Wartenberg syndrome?
The most prevalent kind of autosomal dominant syndromic hearing loss is Waardenburg syndrome. It includes pigmentary anomalies of the skin, hair (white forelock), and eyes (heterochromia iridis) as well as sensorineural hearing loss.
For Wartenberg syndrome, what kind of splint is used?
At the initial post-operative visit, patients will be put in a detachable thumb spica splint. After two to three weeks of wearing this splint, patients will start treatment. Patients might anticipate returning to their regular activities in 4-6 weeks after therapy, which typically lasts 2-3 weeks.
What is Wartenberg syndrome known by another name?
“cheiralgia paraesthetica” is another name for it. because of compression caused by the extensor carpi radialis longus (ECRL) and brachioradialis relative motion during forearm rotation.
What distinguishes radial tunnel syndrome from Wartenberg syndrome?
Wartenberg’s syndrome, the most well-known kind of SRN compression, manifests as a painful feeling in the SRN-innervated area. The areas impacted and the compressed position of the radial nerve distinguish RTS from Wartenberg’s syndrome.
Wartenberg’s Syndrome: What causes it?
Wartenberg’s syndrome can have several causes, such as: having a fractured forearm and wearing a tight cast. wearing handcuffs, watches, or tight wristbands. suffering from a slight wrist injury.
Why does Wartenberg occur?
The brachioradialis and extensor carpi radialis tendons compress the superficial radial nerve in this situation, particularly when the forearm is pronating. Perform this exercise without experiencing any pain.
Wartenberg’s migrating sensory neuropathy: what is it?
Frequent bouts of scorching pain and loss of feeling in the distribution of one cutaneous nerve at a time are hallmarks of Wartenberg’s migrating sensory neuropathy. The skin of the face, chest, and limbs are frequently affected.
A good Wartenberg sign is what?
The observation of the fifth digit abduction movement and the incapacity to adduct the fifth finger while extended are good indicators of Wartenberg’s syndrome.
Cheiralgia: What is it?
It shows up as sensory abnormalities in the dorsal and radial parts of the hand and wrist, including paresthesias. Another name for it is Wartenberg’s syndrome.
References
- Physiotherapist, N. P.-. (2023e, December 13). Cheiralgia Paresthetica (Warternberg syndrome): Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/cheiralgia-paresthetica-warternberg-syndrome/
- Wikipedia contributors. (2023, August 25). Wartenberg’s syndrome. Wikipedia. https://en.wikipedia.org/wiki/Wartenberg%27s_syndrome
- Anthony, J. H., Hadeed, A., & Hoffler, C. E. (2023, June 5). Cheiralgia Paresthetica. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK545200/