Charcot Foot
Introduction
Charcot foot is the term for when you lose feeling in your ankles and feet. You might not be aware of the signs of an infection or injury that is causing your foot pain. These problems might cause more harm the longer they are left untreated. If you have diabetes, it’s crucial to have regular foot inspections performed by a healthcare professional.
The disorder known as Charcot neuropathic osteoarthropathy or “Charcot foot,” affects the soft tissues, joints, and bones of the foot and ankle and is initially characterized by inflammation. Diabetic neuropathy has emerged as the most prevalent cause of Charcot foot, while it has been reported to result from certain other peripheral neuropathies.
Diabetes, sensory-motor neuropathy, autonomic neuropathy, trauma, and metabolic abnormalities of bone all interact to cause an acute localized inflammatory condition that can cause bone destruction, subluxation, dislocation, and deformity in different degrees and patterns. Midfoot collapse, sometimes known as a “rocker-bottom” foot, is the characteristic deformity linked to this disorder, however it can also manifest in other joints and different ways. During the acute stage of this condition, pain may be present, although it may be much less severe than in people with normal sensitivity and comparable injury levels.
What is Charcot foot?
A rare consequence of diabetic neuropathy is Charcot foot. It can significantly worsen the condition or injuries. Nerve damage from diabetes-related neuropathy causes you to lose sensation in your feet and lower legs. This makes it difficult, if not impossible, to detect pain or other indications that your foot is hurting. Since you can’t feel or see the symptoms, Charcot foot occurs when a minor injury or infection leads to serious problems.
Charcot foot can cause your foot’s joints to collapse and impair your foot’s functionality permanently if treatment is delayed. Additionally, it may increase the likelihood that an infection in your foot may worsen or spread to other parts of your body. In extreme situations, this may result in life-threatening problems or the need to have your foot amputated.
Regularly consult a medical professional about controlling your blood sugar levels and diabetes. The best defense against Charcot foot is to see a doctor regularly and have your feet checked for changes or loss of touch, pressure, or pain.
Charcot foot is a disorder in which joints dislocate, fractures do not heal, and the foot may collapse. Some diabetics may develop the condition as a result of peripheral neuropathy. This is where the feeling is affected by high blood sugar levels because they make it more difficult for the nerves to transmit instructions from the brain to the foot (or other regions of the body).
As a result, nerves may become damaged or eventually disappear. You can begin to lose your foot’s sensation or feeling. You might not be aware that you need to see a doctor since you won’t be able to feel or see if your foot is damaged in any way, including by traumas or broken bones.
Other terms that medical professionals may use in place of Charcot foot include:
- Diabetes-related foot.
- Charcot arthropathy.
- Charcot neuropathy.
Stages of Charcot foot
Stage One: Fragmentation and destruction
- The foot and ankle will be red, swollen, and heated during this acute stage.
- Internally, little bone fractures and soft tissue edema are beginning to appear. The joints and surrounding bone are destroyed as a result. As a result, the joints become unstable and can dislocate. It is possible for the bones to completely soften and turn into a gel.
- Rocker bottom foot deformity
- Bony protrusions
- This stage may continue for up to a year if treatment is not provided.
Stage Two: Coalescence
The body makes an effort to repair the harm caused in the initial phase. There is less edema, redness, and warmth as the breakdown of the bones and joints slows down.
Stage Three: Reconstruction
- This is the last phase of the foot’s joint and bone healing process. Unfortunately, they cannot, on their own, revert to their original form or status. The foot is frequently left in a distorted, unstable state even when no additional harm is being done to it.
- Additionally, the foot may be more susceptible to the development of ulcers and sores, which can lead to further deformity or, in certain cases, require amputation.
Causes
Charcot foot occurs when you have an infection or injury to your foot but are unable to feel the pain. It is typically a foot disease associated with diabetes:
- Hyperglycemia, or High blood sugar, is more common in diabetics who struggle to control their blood sugar (blood glucose) levels.
- Long-term, regular hyperglycemia can lead to neuropathy, or damage to the nerves, particularly in the lower limbs. You have less feeling and sensation in the affected foot as a result of the nerve injury.
You’re more likely to overlook symptoms that require medical attention if you’re unable to detect pain or other indications that something is wrong with your ankle or foot. Problems that are easily resolved can worsen before you become aware that you are in pain.
People with Charcot foot, for instance, may continue to walk on an injured foot while being unable to perceive the pain that indicates injury to their bones, tendons, or ligaments. If you continue to walk on your foot without realizing it hurts, a typically mild ankle injury or bone fracture could go considerably worse. The additional strain over time may permanently alter the curvature of your ankle and foot.
Similarly, you may not notice signs of an infection until it has created serious consequences if you have Charcot foot and are unable to detect signals like pain or a warm feeling.
Symptoms
Early symptoms of Charcot foot include:
- Foot pain.
- Discoloration or redness.
- Swelling.
- A sensation of warmth or heat, particularly when one foot feels substantially warmer than the other.
Later on, the foot or ankle becomes malformed as a result of the foot’s bones breaking and shifting out of alignment.
- Rocker-bottom foot is a characteristic Charcot sign. When the bones in the center of the foot give way, this happens. As a result, the foot’s arch collapses and bends downward.
- Downward curling of the toes may occur.
- Foot ulcers and pressure sores can result from bones that protrude at strange angles.
- These ulcers and sores may deepen or widen before anyone notices them since the feet are numb.
Additionally, high blood sugar impairs the body’s ability to fight against illness. These foot sores could consequently get infected. As soon as you observe any changes in your feet, you should see a doctor. Serious problems are less likely to occur if your doctor diagnoses Charcot foot early.
The following are examples of more severe Charcot foot deformities that can alter the shape of your foot:
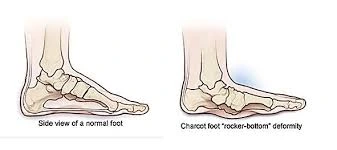
- A rocker-bottom foot. The collapse and disintegration of the bones in the center of your foot can result in a rocker-bottom foot. This causes your foot’s arch to collapse. The foot of a rocker is smoothed out rather than naturally curved upward. Where the arch formerly was, you may have a bulge in the center of your foot.
- Shape alterations of the toes: You might curl or curve your toes beneath. If your foot’s bones and other tissues shatter or collapse, your toes compensate by forming a claw-like grip to keep you steady.
- Changes in ankle shape: One side of your ankle may flex or curl, making it appear notably less stable and straight than the other.
- Foot ulcers: You may apply excessive pressure to certain parts of your foot if Charcot foot causes your ankle or foot to change form. Open sores or ulcers may result from this, raising your risk of infection.
Diagnosis
A physical examination and a few imaging tests are used by a medical professional to diagnose Charcot foot. If you have any symptoms, such as pain, swelling, a warm sensation, or a loss of sensation in your ankles, feet, or toes, let your healthcare professional know.
Your doctor will check your feet and ankles. They will examine both of your feet and compare them to check for any variations. By touching your ankles, feet, and toes, your healthcare practitioner will also assess your level of foot sensation.
To diagnose Charcot foot, your healthcare professional may employ several tests, such as:
Foot X-rays.
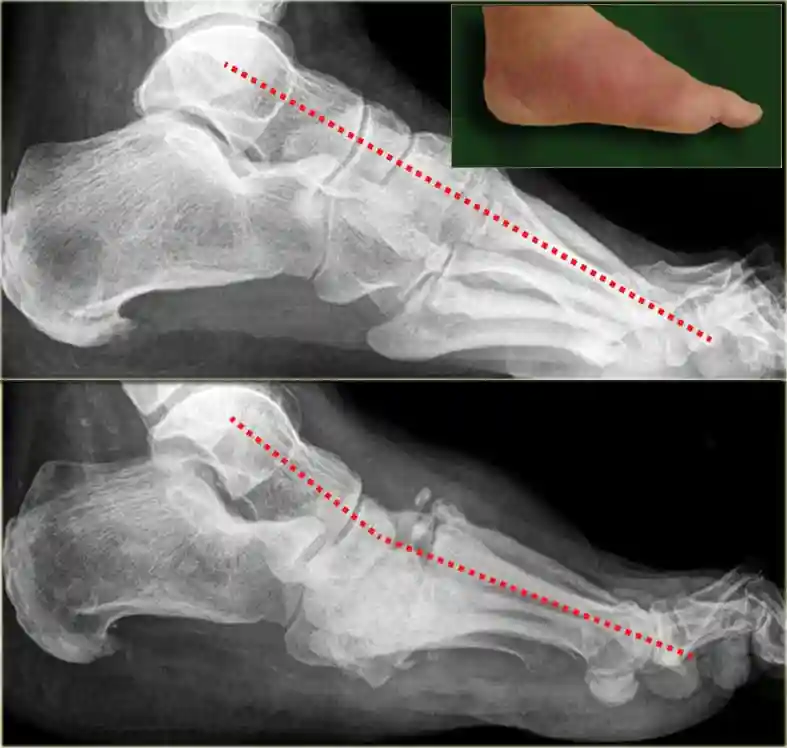
The main first imaging technique used to assess the foot in diabetes patients is radiography. They offer details on bone alignment, mineralization, and structure and are easily accessible and reasonably priced. A normal X-ray may show minor fractures and dislocations, or it may subsequently reveal more obvious fractures and subluxations. Later on, the talo-first metatarsal angle is broken and the calcaneal inclination angle is decreased. Most Charcot foot includes medial calcification of the arteries, which is a common secondary finding on radiographs. However, radiographic alterations of CN usually have low sensitivity and are delayed.
CT scan (computed tomography).
A CT scan can give an extremely detailed image of the bones since it can be compared to a three-dimensional X-ray. If your doctor thinks you require surgery for Charcot foot, they will probably order a CT scan. Planning the precise kind of operation you require might be made much easier with the help of the comprehensive CT scan.
MRI (Magnetic resonance imaging).
When X-rays may still be normal in the early stages of active CN, magnetic resonance imaging (MRI) enables the detection of minor alterations. MRI can provide a detailed picture of anatomy and pathology in both soft tissue and bone, mainly by imaging protons in fat and water. MRI has a high sensitivity and specificity for osteomyelitis due to its unique capacity to differentiate tissues with high precision. As a result, it has emerged as the preferred diagnostic for evaluating diabetes patients’ complex feet. MRI is particularly helpful in diagnosing Charcot bone and joint alterations at their early onset, before the changes show up on plain films, even though it is not necessary for diagnosis when X-rays are diagnostic.
Bone scan
One nuclear medicine test that may be useful in identifying the presence of a bone infection is a bone scan. Different bone scan kinds exist, and the doctor must decide which type or types are most appropriate for a certain issue. These tests can still be equivocal, but they are somewhat better than MRI in differentiating between a bone infection and Charcot. A marker is applied to white blood cells as part of a specialized test called an indium scan. After that, these cells are tracked to determine if they are traveling to the bone to combat an infection.
Only an infection will exhibit noticeably elevated activity on the indium scan, however, both Charcot foot and bone infection will result in a positive bone scan.
- Blood tests to check for signs of infection.
- Electromyography
- Nerve conduction velocity tests
- Nerve biopsy
Treatment
The most crucial aspect of treating Charcot foot is avoiding serious complications. Before any problems or injuries worsen (advance), you must stop walking on your foot. Your doctor will provide therapies to alleviate your symptoms and lessen the long-term impact Charcot foot has on your foot’s functionality.
Medical Treatment
- Diabetic Wound Care Management.
- All infected wounds should receive antibiotic treatment in addition to wound care until the infection is resolved.
- For infections that pose a threat to limbs or are out of control, hospitalization, immobilization, and intravenous antibiotics are recommended.
- Urgent surgery is indicated if the infection is accompanied by a deep abscess, extensive bone or joint involvement, crepitus, substantial necrosis or gangrene, or necrotizing fasciitis. They advise that the risk of significant amputation is likely to be reduced by surgical intervention for moderate or severe infections.
The overall objective of treating Charcot foot is to produce a plantigrade (able to rest flat on the floor) foot free of ulcers so that the patient can walk comfortably in a diabetic shoe that is sold commercially. Treatment seeks to do this by making sure the foot is:
- Stable: The patient’s foot and ankle are strong and shaped to sustain their weight and enable walking without developing new abnormalities.
- Plantigrade: The foot can lie flat on the ground as it should. Consider the foot as a three-legged stool made up of the big toe, the little toe, and the heel to grasp this idea. The foot is plantigrade if all three of these points can rest on the ground while the patient is standing normally.
- Braceable: Deformities and ulcers can probably be avoided if the foot can be rendered stable and plantigrade with the use of shoe inserts and braces, even if it is not in a normal posture on its own.
- Ulcer-free: The ultimate goal in Charcot treatment is to avoid ulcers. You can avoid infections and probably amputations if you can prevent ulcers. The secret to avoiding ulcers is to avoid or treat bony prominences beneath the epidermis. In addition to assisting the patient in walking normally, the aforementioned therapy objectives can be considered strategies to reduce the likelihood of an ulcer developing.
Nonsurgical Treatment
Immobilization
- You will be required to wear a complete contact cast by your healthcare practitioner. Your ankle and foot movement will be restricted as a result. You will probably need to use a wheelchair, crutches, or a knee-walker gadget to keep your weight off your foot completely. As the swelling subsides, new casts will be applied to your foot. It may take several months or longer to heal.
Casting
- To protect the foot and ankle in the early phases of Charcot, a cast or special boot is typically used. Castings are used to help the bones heal in a stable position and stop more abnormalities from forming. A cast works wonders for protecting the bones and minimizing edema.
- For Charcot foot, the most popular kind of cast is called a “total contact cast.” This covers the entire foot and is comparable to regular casts in many aspects. When wearing a cast, the patient must not bear weight on the foot until the bones have had time to mend. Typically, a wheelchair, knee scooter, or crutches are required. Sometimes it takes three months or longer to heal.
- To make sure the cast stays on the leg while the swelling goes down and to make sure ulcers don’t form, it is often replaced every week or two.
Patients are occasionally moved to a specialized heavy-duty boot that covers the entire foot similarly but is detachable once the edema has subsided. The advantage of removing the cast and putting on the boot is that it permits walking and may be removed to examine and clean the foot. The ultimate objective is to resume wearing regular shoes.
Taking weight off your foot
Reducing pressure and weight on your injured foot helps to minimize swelling and stop injuries like bone fractures from getting worse. You may require:
- A cast or brace.
- Crutches.
- A walker.
- A wheelchair.
Orthotics and footwear changes

Orthotics are shoe inserts that maintain the proper position of your toes and support your feet. You may require an ankle brace or specially manufactured insoles. To help relieve additional strain on your feet and support you when you walk, your healthcare physician may suggest orthotics or customized shoes with more depth.
Changes in activity: There is always a chance that Charcot foot will return or spread to your other foot. Therefore, to preserve your feet, your provider can suggest modifying your activities, such as minimizing how much you stand or walk. You might have to reduce your foot-based activities by using a wheelchair.
Surgical Treatment
Surgery might be the best course of action when casting and bespoke footwear alone are unable to accomplish the aforementioned Charcot therapy goals.
- If the abnormalities make it difficult for you to walk normally or increase your chance of developing ulcers, surgery can be advised.
- Surgery is also necessary for the healing of unstable fractures and dislocations.
A few surgical alternatives for the different issues that Charcot may cause are listed below. To address the unique demands of each patient, these procedures are frequently carried out in combination.
Debridement of ulcers.
Surgery may be necessary to help ulcers heal. Debridement is only the process of cleansing the ulcer and getting rid of any dead skin that won’t heal. After debridement, a cast may be applied to relieve pressure on the ulcer while it heals.
Lengthening the calf muscle or Achilles tendon.
The Achilles tendon or calf muscle may be tight, however, this is not always the result of an injury. This tightness may cause ulcers by creating pressure points on the sole, particularly in the ball, or front, of the foot. This pressure can be lessened by strengthening the Achilles or calf muscles.
Removal of bony prominences (Exostectomy).
Prominent bones beneath the skin can result from deformities, and ulcers can develop as a result of the pressure those bones put on the skin. Removing the bone fragment is the easiest method to stop an ulcer from developing from a bony prominence. The inside and bottom of the foot are particularly vulnerable to ulcers due to prominences.
Charcot deformity correction.

Plates, screws, and/or rods may be needed to correct abnormalities and get the bones to heal in the proper position when fractures and dislocations are unstable and/or the bones are noticeably out of place. Fractures in diabetics are usually more complicated because of low bone quality. As a result, procedures to correct them typically call for more hardware (plates and screws) than those required for people without diabetes. If any of these procedures are carried out, bone graft material might also be used to aid in bone healing.
- Dislocated bones can be made to heal into a single, solid piece of bone through a procedure called an arthrodesis, or joint fusion. A key component of Charcot treatment, joint fusions are effective procedures for reversing deformity and enhancing stability.
- It might be enough to just heal the shattered bones (open reduction and internal fixation) in cases of acute fractures without significant joint dislocations.
- To preserve stability in cases of severe abnormalities, especially those involving the heel or ankle, a substantial rod may need to be placed into the ankle.
- Amputation. It might not be possible to salvage all or part of the foot in severe cases of Charcot arthropathy, such as those that are exacerbated by severe deformity, deep bone infection, or the foot’s blood flow has been turned off. To help the patient stay mobile under these circumstances, the doctor might advise amputation above the disease’s level and then prosthetic device fitting.
Surgical Outcomes
Compared to standard foot and ankle fracture treatment, surgery for a Charcot foot has a higher risk of wound complications, infections, and amputation due to the underlying diabetes and the substantial deformities that are frequently present. The most effective strategies to lower risks are to:
- Maintain blood sugar control because the patient’s hemoglobin A1C level directly affects the likelihood of complications.
- After surgery, avoid bearing weight on the foot until the doctor gives the all-clear.
- In every situation, the advantages and disadvantages of surgery should be carefully considered. Specific success or complication rates vary because of the large range of issues and deformities being treated.
Surgery carries a significant risk of complications, but untreated Charcot foot frequently has an even greater chance of negative results. For example, if surgery is required to repair abnormalities and prevent ulcers, it is typically worth the risk because Charcot patients who have an ulcer have a 50% probability of having their limbs amputated.
Success chances are rather high (usually over 80%) if surgery is performed before an ulcer forms. However, the existence of an ulcer makes surgery much more difficult, mostly due to the higher risk of infection. Following surgery, the foot usually needs to be immobile for at least three months.
Complications from putting weight on the foot too soon and disregarding the doctor’s advice include:
- Difficulty healing the incisions
- New injuries
- Return or even worsening of the deformity
Prevention
Controlling your diabetes and general health is the best defense against Charcot foot. By controlling your blood sugar, you can lower your risk of neuropathy and avoid hyperglycemia. Find out from your doctor how frequently you should get your feet examined. Ask them if you ought to consult a podiatrist or a foot and ankle orthopedist, or another specialist in foot care.
Additionally, you can lower your chance of developing Charcot foot and other foot issues linked to diabetes by:
- Examining your feet daily for any alterations. Remember to keep an eye on your toes. If necessary, use a mirror or ask for assistance.
- Having your feet examined each time you see a medical professional.
- Maintaining the filing and trimming of your toenails. To avoid ingrown toenails, cut them straight across.
- Keeping your feet’s blood flowing. When you sit, keep your feet up high and frequently wriggle your toes.
- Putting on shoes (or slippers) and socks all day. Verify that your shoes fit correctly and that your socks are not too tight.
Doing daily foot washing. Make sure they are completely dry, including in between your toes. Lotion should be applied to the tops and bottoms, but not in between the toes.
Risk factors
People with diabetes are nearly always affected by Charcot foot. Neuropathy is more likely to occur in those with diabetes for more than seven years who smoke and drink alcohol often.
Additionally, having diabetes and other medical disorders increases your risk of developing neuropathy. These illnesses include:
- High blood pressure (hypertension).
- Obesity or overweight.
- High cholesterol.
- Kidney disease.
Prognosis
You should be able to prevent major consequences if a healthcare professional detects Charcot foot early. You will require follow-up sessions with your provider regularly. To look for any changes or new symptoms, they will take further X-rays of your feet.
You may need to utilize mobility aids or learn new ways to walk and move if Charcot foot produces significant symptoms or problems. You can learn more about what to anticipate from your physician. They will help you throughout the way and be available to answer any questions you may have.
Complications
The condition known as Charcot foot is a consequence of diabetic neuropathy. Other major problems could include the following if your foot is sufficiently damaged or you have a serious infection:
- The physical form of your foot may change irrevocably. Most shoes may be difficult to fit into because of this.
- If the physical changes are significant, you could need to have your affected foot amputated, or surgically removed. If an ulcer or wound on your foot or ankle becomes infected, you might have to have it amputated.
- If an infection spreads to other parts of your body or you develop other potentially catastrophic consequences from diabetes, Charcot foot can be fatal.
People with diabetes, a disorder that affects how the body controls blood sugar levels, frequently experience foot complications. Charcot foot, also known as Charcot neuroarthropathy, is one of the more severe disorders where the foot’s bones deteriorate and become more prone to fractures. The foot’s bones could become permanently misaligned if therapy is not received.
Why select an ankle and foot surgeon?
Today’s top specialists in foot and ankle treatment are foot and ankle surgeons. They are the board-certified surgical specialists in the podiatric field and are sometimes referred to as podiatrists, DPMs, or sometimes “foot and ankle doctors.” Compared to other healthcare professionals, foot and ankle surgeons possess the most education and training specifically focused on the foot and ankle.
Foot and ankle surgeons treat patients of all ages with simple to complex foot and ankle diseases, including Charcot foot. Foot and ankle surgeons are qualified to undertake a variety of procedures, including any that would be necessary for Charcot foot, thanks to their extensive education and training.
Conclusion
Prevention is the best way to treat diabetic foot issues. The following are important preventative factors:
- Tight blood glucose management
- Check your feet every day to make sure no cuts or ulcers are forming.
- Wearing full-coverage, sturdy, and supportive shoes is also crucial to avoiding cuts and injuries.
For additional advice on diabetic foot care, see: Taking Care of Diabetic Foot. See your doctor right away if you observe any changes in the foot’s appearance, such as swelling, redness, warmth, or a wound. The better the prognosis, the sooner Charcot arthropathy is identified and treated.
Getting the bones to recover in a stable posture that reduces the chance of ulcers is crucial to treatment once Charcot is diagnosed. Surgery is frequently the best method to avoid severe deformities and ulcers, but occasionally this can be accomplished without it.
To guarantee the greatest possible result from treatment:
- Regarding when it is safe to place weight on the wounded foot, the patient must adhere to the doctor’s advice.
- Patients must make a lifelong commitment to monitoring their blood sugar levels and closely examining their feet each day.
- To identify Charcot foot early and prevent long-term problems, both of these behaviors are crucial.
FAQs
Why does the diagnosis of Charcot foot often take longer than the beginning of symptoms?
Charcot foot’s early symptoms are non-specific and usually appear alongside other, more prevalent illnesses including rheumatologic disorders and infections. Many people either have no pain at all or suffer from pre-existing neuropathy. In contrast to other illnesses including septic arthritis, gout, rheumatoid arthritis, and other inflammatory arthropathies, doctors who are not specialists in orthopedic foot and ankle issues may see a Charcot foot only a few times during their careers.
Which four Charcot stages are there?
Inflammation, fragmentation, coalescence, and consolidation are the four distinct disease stages that define Charcot foot, which correspond to active and inactive disease phases. Typically, the illness only manifests once over these many stages.
What distinguishes Charcot foot from osteomyelitis?
Acute Charcot osteoarthropathy typically affects multiple joints and bones, whereas osteomyelitis typically affects a single focal area, such as the weight-bearing surfaces of the toes, metatarsal heads, or calcaneus.
What characteristics does Charcot have?
Charcot-Marie Tooth, the lesser muscles are the effect of tooth disease. Additionally, you can have trouble walking, muscle spasms, and loss of feeling. Foot abnormalities like high arches and hammertoes are also frequent. Though they may later spread to your hands and arms, symptoms typically start in the feet and legs.
Which imaging method works best for Charcot foot?
MRI scans provide digitized, three-dimensional images of the body’s soft tissues using radio waves and a magnetic field. Inflammation can be shown on MRI pictures, which could indicate an infection. Tiny bone fractures linked to Charcot foot may also be indicated by inflammation.
What kind of arthritis is Charcot?
Neuropathic arthritis, sometimes referred to as neurogenic arthropathy or Charcot’s joint, is a severe type of arthritis in which the joint has been badly injured by ongoing friction and the cartilage between the bones has entirely worn down.
What are Charcot’s early symptoms?
In the beginning, your foot and ankle may feel swollen, red, and warmer. Severe abnormalities, such as collapse of the midfoot arch (often referred to as rocker bottom foot) or instability of the ankle and hindfoot, may develop later when fractures and dislocations take place.
Which four Charcot stages are there?
Inflammation, fragmentation, coalescence, and consolidation are the four distinct disease stages that define Charcot foot, which correspond to active and inactive disease phases. Typically, the illness only manifests once over these many stages.
Does Charcot foot cause recovery?
Patients with Charcot foot are frequently confined to wheelchairs and, in extreme situations, may need to have their limbs amputated. An orthopedic surgeon at Loyola University Medical Center, treats patients with Charcot foot from all over the nation. Ninety-one percent of his patients can walk normally again after the procedure.
Reference
- Charcot foot. (2024, December 19). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15836-charcot-foot
- Rogers, L. C., Frykberg, R. G., Armstrong, D. G., Boulton, A. J., Edmonds, M., Van, G. H., Hartemann, A., Game, F., Jeffcoate, W., Jirkovska, A., Jude, E., Morbach, S., Morrison, W. B., Pinzur, M., Pitocco, D., Sanders, L., Wukich, D. K., & Uccioli, L. (2011). The Charcot foot in diabetes. Diabetes Care, 34(9), 2123–2129. https://doi.org/10.2337/dc11-0844
- Charcot foot: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/007748.htm
- Charcot Foot – Rocker-Bottom foot deformity | Foot Health Facts – Foot Health Facts. (n.d.). https://www.foothealthfacts.org/conditions/charcot-foot#:~:text=Charcot%20foot%20is%20a%20condition,tendency%20to%20develop%20Charcot%20foot.
- Isobel.Sims. (n.d.). Charcot foot and diabetes. Diabetes UK. https://www.diabetes.org.uk/about-diabetes/complications/feet/charcot-foot#:~:text=with%20Charcot%20foot-,What%20is%20Charcot%20foot?,foot%2C%20and%20help%20avoid%20amputations.
- Charcot arthropathy (Neuroarthropathy) symptoms & causes. (n.d.). FootCareMD. https://www.footcaremd.org/conditions-treatments/the-diabetic-foot/charcot-arthropathy#:~:text=Charcot%20foot%20occurs%20in%20patients,with%20extensive%20fragmentation%20and%20deformity.
- Charcot foot. (n.d.). NYU Langone Health. https://nyulangone.org/conditions/charcot-foot#:~:text=Specialists%20in%20orthopedic%20surgery%2C%20vascular,prevent%20Charcot%20foot%20from%20recurring.
- Diabetic (Charcot) foot – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/diabetic-charcot-foot/