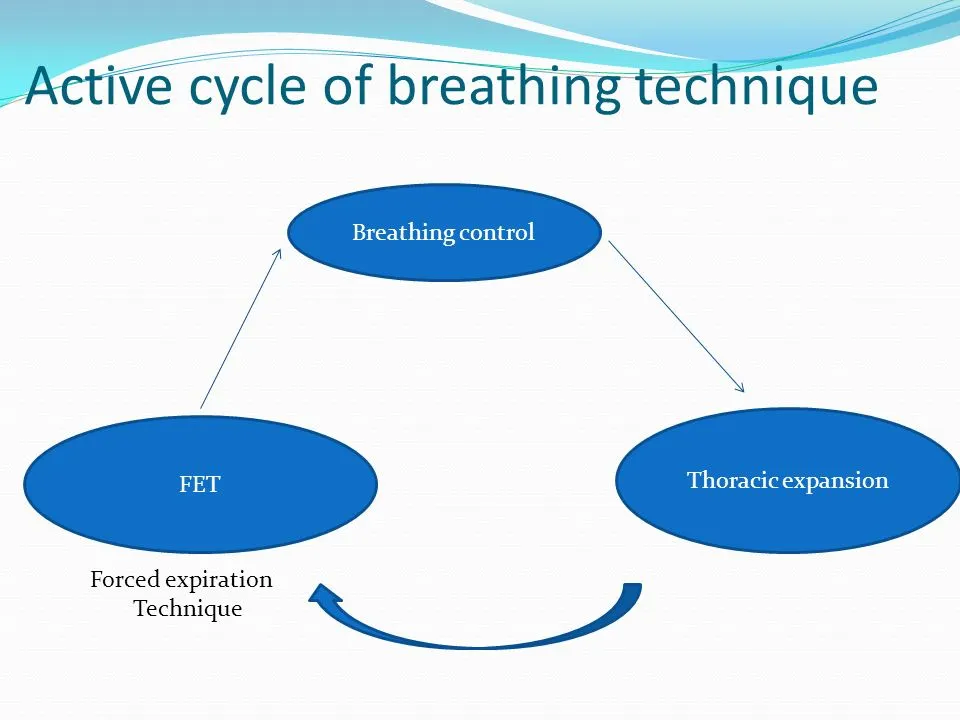
Active Cycle of Breathing Technique (ACBT)
What is a Active cycle of Breathing Technique (ACBT)?
The Active Cycle of Breathing Technique (ACBT) is a physiotherapy technique used to clear mucus from the lungs, commonly for individuals with respiratory conditions like COPD or bronchiectasis.
It consists of three main phases: breathing control, deep breathing exercises, and forced expiratory technique (huffing) to improve airflow and facilitate mucus clearance.
Techniques for clearing the airways include
- Autogenic drainage
- Active cycle of breathing technique (ACBT).
- Manual percussion is another name for chest percussion treatment (CPT).
- Exercise.
- High-frequency chest wall oscillation vest.
- Coughing with a huff.
- Positive expiratory pressure(PEP)
Introduction
The Active Cycle of Breathing Techniques (ACBT) is a patient-performed active breathing technique that can be utilized to improve lung function in general as well as mobilize and remove excessive pulmonary secretions.
It is a dynamic therapy approach that may be modified for use by the majority of patients and combined with placement. Depending on the problem facing the patient, each element can be applied alone or as a part of the ACBT cycle.
After learning ACBT, the patient can be encouraged to utilize it on their own without a physical therapist’s guidance. No specialized equipment is needed for this activity.
It is used for:
- Clear or loose pulmonary secretions. This lowers the chance of developing a chest infection.
- Increase the lung’s airflow.
- Increase a cough’s effectiveness.
Three Stages of ACBT:
- Breathing Control
- Thoracic Expansion or Deep Breathing Exercise
- Forced Expiratory Technique (FET) or Huffing
The method can be changed according on the patient’s condition. Additionally, if necessary, a manual technique (MT) or positive pressure can be used to produce a more complex cycle that will help in the better removal of secretions from the lungs. This could involve expiratory vibrations or percussion.
Active cycle of breathing combined with regular chest physical therapy improved arterial oxygenation, heart rate, and pain perception after Coronary Artery Bypass Surgery (CABG), according to a randomized control experiment.
Breathing Control
In order to relax the airways and relieve the tightness and wheezing that typically follow coughing or dyspnea, breathing control is used. Between the technique’s more complex parts, there is a resting interval.
It can also help to create calmness if the patient is encouraged to close their eyes while doing breathing control. Breathing control is crucial because it helps the airways to relax in between the more intensive ACBT activities.
Additionally, breathing control can be helpful when someone is suffering from anxiety, panic attacks, bronchospasm symptoms, shortness of breath, or fear. Depending on the patient’s level of dyspnea, the duration of breathing control may change.
The patient may typically be told to take six breaths when this method is used with them as part of ACBT.
Instruction to patients:
- As it is possible, softly inhale and exhale through your nose. If you can’t, use your mouth to breathe (the patient breathes at his own pace).
- It is suggested to utilize breathing control with pursed lips breathing if you exhale through your mouth.
- With each exhale, try to release any stress in your body and maintain a relaxed posture.
- Try to slow down your breathing gradually.
- To help you relax and concentrate on your breathing, try closing your eyes.
- Until the person feels and able to go on to the other phases of the cycle, breathing control should be maintained.
- Be careful that the person practicing the ACBT is not using the accessory muscles for breathing or performing trick movements like neck extension or trunk bending forward.
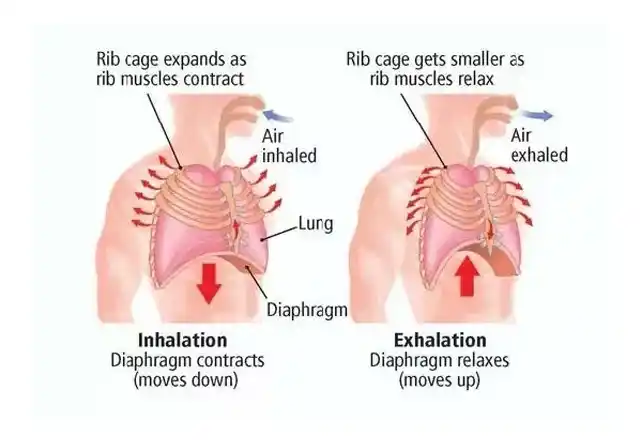
Thoracic Expansion or Deep Breathing Exercise
Exercises involving deep breathing and thoracic expansion concentrate on inspiration and help in the release of secretions that have been accumulated in the lungs. Before a relaxed, comfortable, and unforced expiration, active inspiration is typically followed by a three-second end-inspiratory hold.
Instructions to patient:
- Keep your shoulders and chest relaxed.
- Take a calm, deep breath through your nose if you can.
- Hold the air in your lungs for two to three seconds after you’ve finished breathing in, then exhale (this is called an inspiratory hold).
- Exhale in a relaxed, gentle manner. Don’t expel the air.
- Do this three to five times. It is important that the patient return to the breathing control phase of the cycle if they experience dizziness.
- Proprioceptive input, in which the patient or therapist places their hands on the thoracic cage, can help to promote a maximal inspiration. This has been related to better ventilation and more mobility of the chest wall.
- To make up for asymmetrical ventilation, which can occur in some respiratory disorders because of sputum retention and/or atelectasis, a breath hold can be added to the deep breath.
Forced Expiratory Technique or Huffing

This method is utilized to move secretions that have been mobilized by thoracic expansion exercises or deep breathing down towards the mouth so that they can be coughed up or removed by suction.
Rather of coughing, a huff is an exhalation through an open mouth and throat. Sputum cannot be eliminated from small airways by coughing alone, thus huffing helps transfer it from the small airways to the bigger airways where it may be coughed out.
The patient is first taught to inhale mediumly and exhale with mild to moderate effort and prolonged expiratory flow while keeping the glottis open.
To maximize air movement and the removal of secretions, the huff’s duration and the force with which the muscles of expiration contract should be changed.
Two varieties of huff exist:
- Medium Volume Huff
- High Volume Huff
Medium Volume huff
This facilitates the movement of lower-level secretions through your airways.
Breathe in normally, then exhale vigorously and for a long time until your lungs feel completely empty. Consider that you are attempting to heat up your spectacles or a mirror.
High-Volume Huff
- In the upper airways, this facilitates the movement of secretions.
- Inhale deeply, then swiftly exhale by opening your mouth wide.
- Huffing frequently might cause your chest to tighten, so only do one or two at a time.
- You may need to cough and clear secretions; try spitting them out into a tissue or a sputum bowl if you hear crackles when you huff. Try to return from coughing if it is too much as this could make the procedure less effective and too exhausting.
- For roughly ten minutes, or until the chest feels light, repeat the entire cycle.
- Don’t use this huff before it feels ready to come out. Huffs function by dynamic compression, and small, long huffs move sputum from low down into the chest while huge, short huffs move sputum from higher up into the chest.
Coughing
If huffing doesn’t remove your sputum, you should cough as well. You might not need to cough, though, if it does remove your sputum.
Long coughing episodes should be avoided since they can be exhausting, cause dyspnea, or cause tightness or soreness in the chest or throat. Coughing should only be done if the sputum is easily cleared; otherwise, start the cycle again.
Indication
- Post-injury/pain (ICC/rib fracture).
- Sputum output is chronically elevated, as in cases of cystic fibrosis and chronic bronchitis.
- Acute sputum output.
- Inadequate growth.
- Sputum Retention.
- SOBAR/SOBOE.
- Cystic fibrosis.
- Bronchiectasis.
- Atelectasis.
- Weakening of the respiratory muscles.
- Mechanical ventilation.
- Asthma.
- Increased effort or pace of breathing.
- Airway rumbling that can be heard.
- Palpable secretions.
Precaution
Throughout ACBT, it’s critical to continuously check for increased dyspnea or dizziness. Reduce the number of deep breaths a patient takes throughout each cycle and go back to breathing control if they experience dizziness.
- Insufficient pain management when required.
- bronchospasm.
- surgery on the head, neck, or spine that is sudden and unstable.
Contraindications
- Patients are not breathing on their own.
- Unconscious patient.
- Individuals who have trouble following instruction.
- Confused or agitated.
Positioning
ACBT positioning can be done while sitting or in a position that promotes postural drainage. You could begin by sitting for a while until you feel secure enough to explore other positions. Its effectiveness in sitting or gravity-assisted positions is well-supported by examinations.
Your medical condition and how effectively the ACBT works for you will determine the optimal position for you to perform it. Maintaining a healthy breathing pattern when seated with your shoulders relaxed, neck relaxed, and back supported helps the diaphragm work better and lessens the strain on your musculoskeletal system.
Make sure you are relaxed, comfortable, and well-supported in whatever posture you choose.
The ACBT can be carried out with or without a helper who provides shaking, percussion, and vibration. The patient may involve compression or self-percussion.
It has been demonstrated that people prefer the straight, side-lying position, which is equally as effective as the head-down position.
Time and Frequency
The recommended duration for ACBT is ten minutes or so, or until your chest feels free of sputum.
When you’re feeling good, you might only need to perform ACBT once or twice day. You might need to do it more frequently if you have more sputum. Shorter and/or more frequent sessions may be necessary when you are ill or have more sputum.
Side effects
- Hyper-reactive airways and bronchospasm.
- Decreased oxygen saturation and dyspnea.
- Cardiac irregularities.
- Atelectasis.
- Fatigue.
FAQs
What is the active cycle of breathing?
Technique for Active Cycle of Breathing (ACBT) Three steps of the Active Cycle Breathing Technique (ACBT) integrate several breathing strategies to help remove mucus from the lungs. The first stage facilitates airway relaxation. The second stage aids in clearing mucus and allowing air to pass behind it.
What is the active cycle of breathing techniques for bronchiectasis?
It involves repeating a cycle composed of several distinct steps. These consist of breathing normally for a while, then taking deep breaths to force the mucus up and loosen it, and finally coughing it out. After 20 to 30 minutes, the procedure is repeated.
Is it passive or active to exhale?
Breathing is supported by the intercostal and neck muscles, which move the rib cage. Breathing out occasionally involves the use of abdominal muscles. In the absence of exercise, exhalation, also known as expiration, is typically a passive process.
What is an asthmatic’s active breathing cycle?
A series of breathing techniques called ACBT helps clear your airways of mucus. A physical therapist is the ideal person to teach ACBT. The ACBT exercises include deep breathing, puffing, and breathing control. You do these in a cycle until your chest feels clear.
What breathing method is used in FET?
A huff is a technique used to transfer secretions that have been mobilized by thoracic expansion exercises down towards the mouth. When used in combination with breathing control, it is also known as the forced expiration technique [FET]. Although it can be used alone, it should always be a part of any practice for clearing the airways.
What is the breathing cycle?
The action of breathing in and out is known as the respiratory cycle. The respiratory cycle’s primary goals are to eliminate carbon dioxide and introduce new oxygen into the body.
References
- Active Cycle of Breathing Technique (ACBT). (n.d.). Cystic Fibrosis Foundation. https://www.cff.org/managing-cf/active-cycle-breathing-technique-acbt
- Bronchiectasis. (2022, October 19). The active cycle of breathing technique – Bronchiectasis. https://bronchiectasis.com.au/physical therapy/techniques/the-active-cycle-of-breathing-technique





One Comment