Sciatica
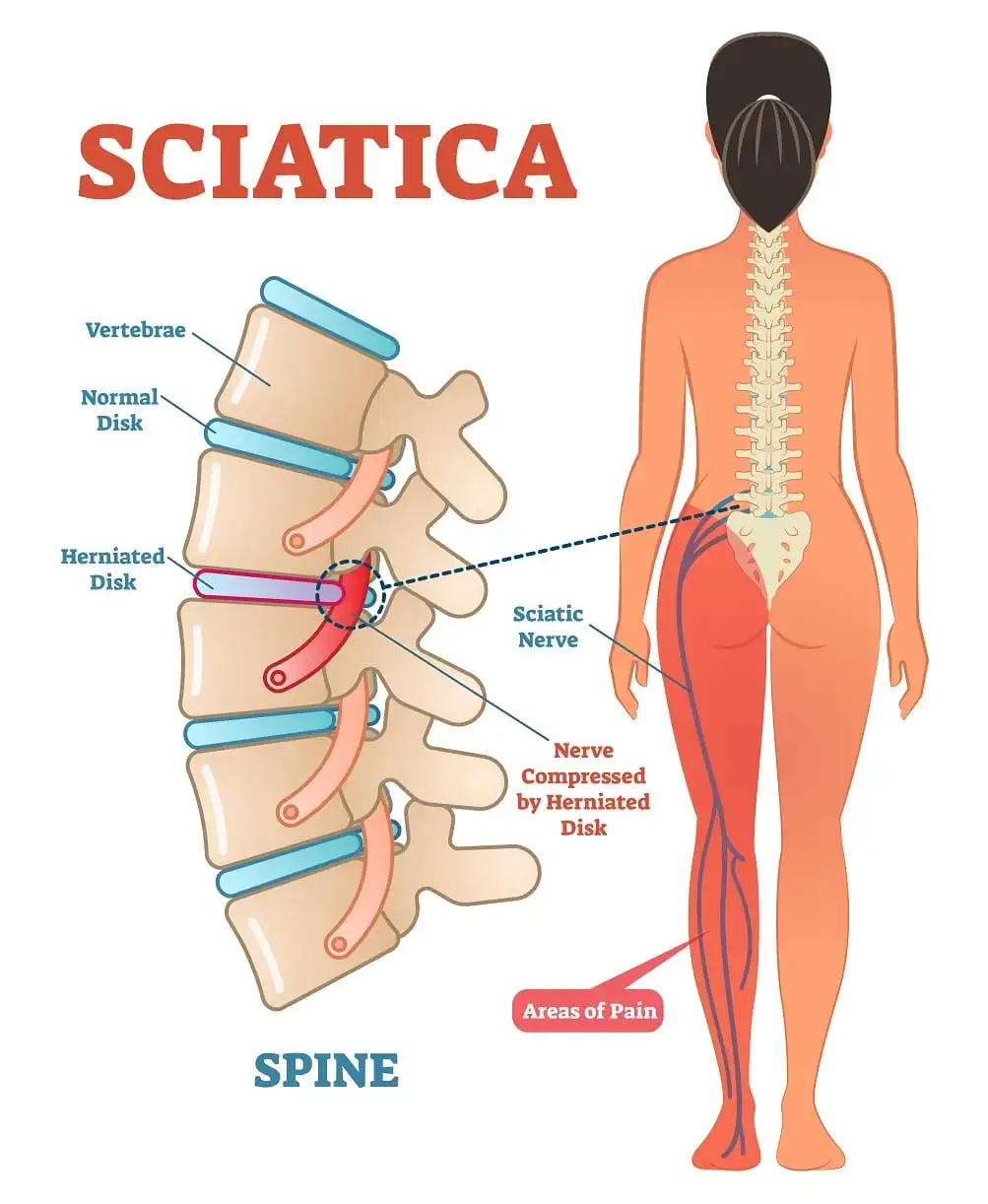
Sciatica is caused by irritation, inflammation, compression, or pinching of one or more nerves that run down your legs and down your lower back.
The sciatic nerve is located in the rear of the leg. It supplies the back of the knee and the muscles of the lower leg. The sciatic nerve also senses the sole, the back of the thigh, and a section of the lower leg.
A partial nerve injury can result in weakness in the flexion (bending) of the knee, weakness in the foot movements, and difficulty bending the foot inwards (inversion) or downwards (plantar flexion). An individual may have abnormal reflexes if their ankle-jerk reflex is weak or nonexistent. Multiple tests can be performed to determine the cause of sciatic nerve dysfunction.
With time and self-care techniques, the majority of sciatica sufferers recover on their own, and the condition is typically neither dangerous nor serious. However, surgery can be required in extreme circumstances.
What is a Sciatic Nerve? Anatomy and its Function
- The sciatic nerve is the lengthiest and broadest nerve in the human body. Since it’s a paired nerve, the body has one on each side. It extends from the sacral area and lumbar spine in the lower back through the legs and buttocks to the feet.
- Being a mixed nerve, the sciatic nerve consists of both motor and sensory fibers. The brain receives sensory data from the leg and foot through the sensory fibers. The brain sends instructions to the muscles through the motor fibers, instructing them to contract and move.
Sciatic Nerve Functions
The sciatic nerve has two primary purposes:
- Sensory: The skin and muscles of the lower leg and foot, including the sole, calf, ankle, and back of the thigh, are sensed by the sciatic nerve.
- Motor: The muscles in the back of the leg that are in charge of flexing the hip and bending the knee are controlled by the sciatic nerve. Additionally, it regulates a portion of the lower limb and foot muscles that are in charge of plantar flexion, which is the downward pointing of the toes, and foot inversion, which is the inward twisting of the sole.
Branches of the sciatic nerve
Just before it reaches the knee, the sciatic nerve splits into two smaller nerves:
- The tibial nerve: The tibial nerve innervates the muscles on the back of the lower leg and foot, as well as the skin on the bottom of the foot and the back of the ankle.
- The common peroneal nerve: The common peroneal nerve innervates the muscles of the front of the lower leg, as well as the skin on the outside of the lower leg and the top of the foot.
What is the Sciatica?
- Sciatica can cause pain, numbness, tingling, or paralysis in one or both legs. The sciatic nerve, the longest and biggest nerve in the body, is what’s irritating. Coming from the lower back, the sciatic nerve passes down the legs and buttocks before splitting off to supply sensation and control the muscles in the foot and legs.
- Sciatica pain can range in severity from a little hurting to a burning pain that prevents movement or standing. It may also be accompanied by tingling or numbness in the leg or foot.
- The most common cause of sciatica is a herniated disc, a condition in which the sciatic nerve is compressed by the soft inner section of a spinal disc protruding outward. Other causes of sciatica include piriformis syndrome, spinal stenosis, and pregnancy.
- Conservative methods, including rest, ice, heat, and over-the-counter painkillers, are typically effective in treating sciatica.
- In addition to decreasing inflammation, physical therapy can help strengthen the muscles that support the spine. In certain cases, surgery may be necessary to relieve pressure on the sciatic nerve.
Causes of the Sciatica
Sciatica arises from compression or injury to the sciatic nerve. The following are the main reasons sciatica occurs:
- Sciatica is primarily triggered by a herniated disc. When the soft interior of a spinal disc protrudes and presses against the sciatic nerve, it results in a herniated disc.
- Spinal stenosis: A constriction of the spinal canal known as spinal stenosis can exert pressure on the spinal cord and other nerves, particularly the sciatic nerve.
- Piriformis syndrome: A disorder known as piriformis syndrome occurs when the sciatic nerve is compressed by the spasms of the piriformis muscle, which is situated deep in the buttock.
- Spondylolisthesis: A disorder known as spondylolisthesis occurs when one vertebra slides forward over the other. Both the spinal cord and the sciatic nerve may be compressed as a result of this.
- Pregnancy: During pregnancy, especially in the later stages, the uterus may press against the sciatic nerve.
The following are some of the less common causes of sciatica:
- Cancers
- Infections
- strained muscles
- Bone spurs
Symptoms of the Sciatica
Pain from sciatica can vary greatly. There may be a slight burning, stinging, or tingling sensation. Sometimes the pain is so bad that it prevents the sufferer from moving. The pain usually occurs on one side. Some individuals have extreme pain in some parts of their leg or hip, and numbness in others.
The sole or the back of the calf may also experience discomfort or numbness. It could feel like one leg is weaker than the other. Walking might occasionally cause your foot to become caught in the ground.
Although each person’s experience of the pain is unique, the following are some typical descriptions:
- Sharp, stabbing pains
- A burning ache
- Aching pain
- Sensation of pins and needles (paresthesia)
- Numbness
The pain can begin gradually. Things could worsen:
- Following a position of standing or sitting
- During particular hours of the day, such as at night
- When laughing, coughing, or sneezing—particularly if a herniated disc is the cause.
- When walking more than a few yards or meters or leaning backward, particularly if spinal stenosis is the cause.
- When you’re holding your breath or straining, like when having a bowel movement.
Risk factors of the Sciatica
Risk factors for sciatica can be roughly divided into two categories: changeable and non-changeable variables. Risk factors that are not changeable include things like:
- Age: The discs in your spine naturally deteriorate and thin with age. They may become more prone to compressing and herniating the sciatic nerve as a result.
- Genetics: Some people are just genetically more likely to experience sciatic nerve issues.
- Gender: Sciatica is significantly more common in men than in women.
- Height: Due to the additional strain on the spine, taller persons may be marginally more vulnerable.
You can alter or control changeable risk factors to lower your chance of acquiring sciatica. Among them are:
- Obesity: Carrying too much weight strains your spine and raises the possibility of a herniated disc.
- Smoking: Smoking can worsen inflammation and delay healing by lowering blood flow to the spine.
- Work: You run a higher chance of developing sciatica if your job involves a lot of lifting, twisting, or extended sitting.
- Diabetes: The sciatic nerve is one of the nerves in the body that can be harmed by diabetes.
- Weak core muscles: Weak core muscles can put strain on your lower back and increase your risk of sciatica since they are unable to provide enough support for your spine.
- Bad posture: Hunching over or slouching over might put additional strain on your spine.
Diagnosis of the Sciatica
A medical practitioner will usually use a mix of physical examination, medical history, and occasionally imaging testing to diagnose sciatica.
Medical History: When gathering your medical history, the doctor will ask about your symptoms, including:
- The site and intensity of your discomfort
- Whether your leg hurts all the way down
- Any leg weakness, tingling, or numbness
- Any actions that either worsen or improve your discomfort.
- Your medical record and general state of health
Physical examination: Your legs, spine, and reflexes will be the main areas of attention for this assessment. The physician will look for:
- Your legs’ sense and strength of muscles. Having trouble staying on your toes.
- Your ankles and knees’ reflexes.
- weakness in the knee’s bending motion.
- The flexibility of your hips and spine. Inability to flex the foot downward or inward.Having trouble bending backward or forward.
- Sensory loss or numbness.
- Soreness when you lift your leg straight up while lying on the examination table.
Typical physical examinations for sciatica diagnosis include the following Special tests:
- Straight leg raise test: While lying on your back, slowly raise one leg straight up while keeping the other leg flat. During this test, pain that travels down your leg could be a sign of sciatica.
- Slump test: You sit up straight, place your hands behind your back, and slowly bend forward at the hips while maintaining a straight back and a tucked-in neck. When you lean forward, pain or weakness in your leg could indicate sciatica.
Imaging testing: While they are not typically required to diagnose sciatica, imaging tests might be beneficial if your doctor thinks you have an underlying, more serious illness or if your symptoms are not improving with medication. The following are a few typical imaging studies used to identify sciatica:
- X-rays: Although they are typically unable to display soft tissues like herniated discs, X-rays can reveal bone spurs or spinal canal narrowing.
- MRI scans: An MRI scan can provide you with a detailed picture of your spine as well as the tissues that surround it, including the sciatic nerve. This may assist in determining the origin of your sciatica.
- CT scans: Although CT scans are not as effective as MRIs at displaying soft tissues, they can nonetheless produce detailed images of your spine.
- Neurconduction studies (NCS) and Electromyography (EMG): Your muscles’ and nerves’ electrical activity can be measured by these tests. They can assist in determining whether sciatica has resulted in nerve damage.
- It’s crucial to remember that diagnosing sciatica should preferably be made based on the distinctive symptoms rather than just imaging examinations. Imaging studies can reveal anomalies that aren’t the source of the patient’s discomfort.
Differential Diagnosis of the Sciatica
A differential diagnosis is essential to determine the exact cause of your pain because sciatica symptoms might resemble those of other illnesses. When making a sciatica diagnosis, a physician would take into account the following important conditions:
Spinal Disorders:
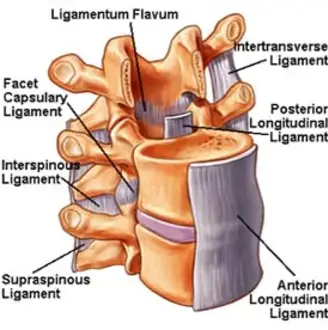
- Herniated disc: The primary root cause of sciatica is a herniated disc, which occurs when the soft interior of a spinal disc bulges and compresses the sciatic nerve.
- Spinal stenosis: A narrowing of the spinal canal that can put pressure on the sciatic nerve and other nerves, including the spinal cord, is known as spinal stenosis.
- Spondylolisthesis: A condition in which one vertebra slides past another, possibly causing the sciatic nerve to be compressed.
- Degenerative disc disease: The progressive degeneration of the spinal discs, which may be a factor in the development of sciatica.
Musculoskeletal disorders:
- Piriformis syndrome: The sciatic nerve may be compressed by a spasm in the piriformis muscle, which is situated deep in the buttock.
- Muscle strain or spasm: Pain can be caused by strained lower back or buttock muscles that irritate the sciatic nerve.
- Facet joint arthritis: An inflammation of the spine’s facet joints can resemble sciatica and cause discomfort that travels down the leg.
Other Disorders:
- Cauda equina syndrome: Multiple nerve roots in the lower spine become crushed in cauda equina syndrome, an uncommon but dangerous disorder that results in weakness in both legs and loss of control over one’s bowels or bladder. A medical emergency has occurred.
- Infection: The sciatic nerve can become irritated and painful when there is an infection in the spine or surrounding tissues.
- Tumour: The sciatic nerve can be compressed by tumors in the pelvis or spine, which can be painful.
- Vascular conditions: Rarely, sciatica-like discomfort can be brought on by issues with blood flow to the buttocks’ nerves.
Non-Musculoskeletal Disorders:
- Shingles: This viral infection can sometimes create a searing sensation that travels along a nerve’s route and resembles sciatica.
- Peripheral neuropathy: Diabetes-related damage to nerves beyond the spine can result in pain, numbness, and weakness that may mimic sciatica.
To distinguish sciatica from these other illnesses, a physician will take into account your medical history, symptoms, and results of a physical examination. For a more conclusive diagnosis, imaging studies such as MRIs, X-rays, or EMG/NCS may be employed.
Treatment and Management of the Sciatica
The good news is that with conservative treatment, sciatica frequently goes away on its own in a few weeks. The many methods of treating sciatica are broken down as follows:
Conservative Treatment:
- Rest: You may help your body heal by allowing inflammation to reduce and by taking a break from physically demanding activities that make you feel worse. Prolonged bed rest is generally not advised, though.
- Heat and ice treatment: Early on in the healing process, using cold packs to the painful area for 15 to 20 minutes at a time, several times a day, can help reduce inflammation. Afterward, utilizing a heated pad or warm compress for heat therapy can enhance blood circulation and accelerate the healing process.
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil) and naproxen (Aleve) are examples of NSAIDs that can be used to treat pain and inflammation, as well as acetaminophen (Tylenol).
- Physical therapy: A key component of treating sciatica is physical therapy. A physical therapist can create a customized training plan to enhance posture, increase flexibility, and strengthen the core muscles that support the spine. These exercises can help enhance general function, lessen discomfort, and stop episodes in the future.
Additional Therapies:
- Prescription drugs: To treat extreme pain, your doctor may occasionally recommend harsher drugs such as muscle relaxants or prescription painkillers. Antidepressants and anticonvulsants are two types of medications that can be used to treat chronic or nerve-based sciatica pain.
- Spinal injections: By reducing inflammation surrounding the injured nerve root, corticosteroid injections can temporarily relieve pain that may continue for several weeks or months.
- Alternative therapies: Acupuncture, massage treatment, yoga, and chiropractic adjustments can provide relief for certain individuals. Nevertheless, conflicting data is supporting the efficacy of various treatments for sciatica.
- Acupuncture: This ancient Chinese medical procedure entails the insertion of tiny needles into specific body locations. Research has provided some support for its efficacy in the treatment of pain.
- Massage therapy: Massage has the potential to reduce sciatic pain by relaxing muscles and enhancing blood flow.
- Pilates and yoga are two types of exercise that can help with sciatica since they strengthen the core, improve flexibility, and encourage good posture.
Surgical Treatment
Surgery is often reserved for patients who have growing weakening or loss of bladder or bowel control, or who have not responded to conservative therapy after a fair trial period. Sciatica surgery options include the following:
- Microdiscectomy: A microdiscectomy is a minimally invasive procedure used to remove a small amount of the sciatic nerve-compressing herniated disc debris.
- Laminectomy: To make more room for the spinal cord and nerves, a little portion of the bone (lamina) near the rear of the vertebra is removed during this procedure.
- Spinal fusion: To stabilize the spine, bone grafts or implants may occasionally be utilized to fuse vertebrae.
Your overall health, the underlying cause of your sciatica, and its intensity will all influence which course of treatment is best. To choose the best course of action for you, it’s crucial to go over all of your treatment options with your doctor.
Physical Therapy for the Sciatica
A vital component of treating sciatica is physical therapy. A physical therapist can create a customized workout plan to address the underlying cause of your discomfort and stop it from coming again. The objectives of physical therapy for sciatica are as follows:
- Reduce pain and inflammation: Using manual therapy techniques such as massage, stretching, and focused exercises, physical therapists can help reduce inflammation and muscle tension around the sciatic nerve. This will result in pain relief.
- Increase your range of motion and flexibility. Sciatica can be exacerbated by tight hamstring and buttock muscles. Stretches to increase flexibility in these regions are part of physical therapy, and they can relieve pressure on the sciatic nerve and enhance your lower back and leg range of motion.
- Strengthen strong core muscles: Strong core muscles stabilize the pelvis and lumbar region, releasing pressure from the lower back and reducing the risk of sciatic nerve compression. Your core muscles will be strengthened with workouts designed by physical therapists, improving your stability and posture.
- Boost your balance and coordination: Avoiding falls and other injuries that might exacerbate sciatica requires good balance and coordination. Your balance and coordination will improve with physical therapy exercises, enabling you to move securely and effectively.
- Educate on good posture and body mechanics: To reduce strain on your spine and sciatic nerve during daily activities, physical therapists can teach you these skills. This may assist in avoiding further occurrences of sciatic discomfort.
The following are a few typical physical therapy treatments for sciatica:
- Manual therapy: This hands-on method uses manipulation, mobilization, and massage techniques to increase the range of motion, lessen tense muscles, and accelerate recovery.
- Therapeutic exercises: A physical therapist will create a personalized exercise plan for you that focuses on strengthening your core, stretching, and targeting the muscles that support your pelvis and spine.
- Aerobic exercises: Walking and swimming are examples of low-impact aerobic exercises that can increase blood flow and general fitness, both of which can help with pain relief and recovery.
- Education: You can learn about sciatica, good body mechanics, and ways to avoid flare-ups in the future from physical therapists.
These are a few typical sciatica physical therapy exercises:
Knee to chest stretch:
Stretching from the knee to the chest will assist in lengthening the tense hamstrings, which may be a contributing factor to sciatica pain.
- Lying on your back, rest your feet flat on the base, and pull your legs.
- Take one knee and bring it softly up to your chest with your hands around it.
- As much of your lower back as possible should be in contact with the ground. If it feels comfortable, you can slightly arch your back; nevertheless, do not force it.
- After holding for 15 to 30 seconds, carefully bring your leg back down.
- Continue with the opposite leg.
Lumbar flexion stretch:
Increasing lower back flexibility and reducing sciatic pain can be achieved by gently stretching the lumbar region.
- To finish the exercise, you need to lie on your back, curve your knees, and gradually bring them up to your chest.
- With your hands, grab your knees and gently pull.
- After a brief moment of holding the pose, release your knees and take a step back to the beginning.
Nerve flossing:
This method of flossing the sciatic nerve may lessen discomfort by using light glide strokes.
Sciatic nerve glides: These stretches may increase flexibility, lessen pain, and help mobilize the sciatic nerve.
- For a more intensive sciatic nerve stretch, try the standing sciatic nerve glide, an exercise from the McKenzie Method. To carry it out: With your leg in a lunge position, place one foot on a chair or step. Till your standing leg stretches, gradually bend forward.
Exercises for strengthening the core: Your core muscles support your spine and relieve strain on the sciatic nerve. You can develop them by performing exercises like planks, bird dogs, and bridges.
Glute bridges: By strengthening the gluteal muscles, this exercise helps lessen pain and assist in stabilizing the pelvis.
- Lying comfortably on your back, position your feet approximately hip-width apart and flex your knees.
- Use your abdominal muscles to brace your core.
- Apply pressure with your heels to raise your hips off the floor so that your body creates a straight line from your knees to your shoulders.
- Tighten your glutes at the peak of the movement.
- Hold for a brief moment before lowering your hips gradually to the beginning position.
Complications of Sciatica
Sciatica is a condition that can result from several underlying conditions rather than always being a complication. Nevertheless, problems might arise from sciatica if it is not managed. Below is an explanation of each:
Untreated sciatica complications include:
- Chronic pain: If sciatic nerve irritation is left untreated, it can persist and lead to chronic pain. This could have a significant influence on your daily life because it could make it harder for you to sleep and move around.
- Muscle weakness: Prolonged nerve compression can weaken the leg muscles, making it challenging to walk, climb stairs, or stand for long periods.
- Permanent nerve damage: In severe cases, prolonged sciatic nerve compression can cause irreversible nerve damage. This might result in permanent numbness, paralysis, or even loss of control over the bladder or intestines.
- Spinal deformity: If sciatica brought on by disorders such as spinal stenosis is left untreated, it may deteriorate over time and result in deformities of the spine.
Treatment-related complications: As was previously mentioned, there are differing levels of risk associated with various sciatica treatment approaches. Let’s quickly review:
- Non-surgical interventions: These are normally harmless, although they may have adverse consequences such as upset stomach from medication, strained muscles from incorrect form during exercise, or burns on the skin from incorrect use of heat or ice therapy.
- Surgical interventions: Microdiscectomy and other minimally invasive procedures are generally safe, although there is a chance of infection, bleeding, nerve injury, or recurring disc herniation. Complications from more involved procedures, such as laminectomy or fusion, are more likely to include pseudoarthrosis (incorrect bone fusion), longer recovery, and spinal instability.
Keep in mind that these complications are possible, and how likely they are to occur depends on your particular health and the course of treatment. Maintaining open lines of communication with your physician and doing as they advise are essential to reducing risks and getting the best possible result.
Prevention of the Sciatica
You can assist avoid sciatica by taking a few precautions before it even arises. The following are some crucial strategies to avoid sciatica:
- When standing, sitting, or even sleeping, maintain proper posture. When standing, maintain your core engaged, your shoulders back and aligned, and your eyes forward. Prevent slouching or bending over.
- Use a chair that supports your lower back well when you’re seated, and make sure your feet are flat on the floor and your knees are bent 90 degrees. Avoid of prolonged sitting; take a few minutes every thirty minutes to stand and walk about.
- A firm mattress and well-aligned pillows are essential for sound sleep. If you sleep on your side, place a pillow between your knees, or lie on your back with a pillow under your knees.
- Keep yourself active and engage in regular exercise. This will help you maintain a healthy weight, increase flexibility, and strengthen the core muscles that support your spine. Excellent forms of exercise include swimming, Pilates, yoga, and walking.
- Keep a healthy weight: Being overweight puts additional strain on your lower back and raises the possibility of disc issues, which can exacerbate sciatica.
- Use safe lifting techniques: Bend your knees and maintain a straight back when lifting objects. Avoid twisting your spine when lifting. If the thing is weighty, request others for help.
- Give up smoking: Smoking lowers blood flow to the spine, which can impede healing and increase inflammation, two factors that can lead to sciatica.
- Handle chronic conditions: Taking good care of your diabetes or obesity might help lower your chance of developing sciatica.
- Regular stretching increases flexibility and lowers the risk of sciatic nerve compression in the hamstrings, calves, and lower back.
- Strengthen your core muscles: Planks and bridges are two exercises that focus on your core muscles and can help stabilize your spine, preventing lower back pain that may result in sciatica.
- Pay attention to your body. Steer clear of painful tasks and take breaks as needed.
- You can lower your risk of sciatica and preserve the health of your spine by adopting these preventive steps into your daily life. Recall that seeking individualized advice from a healthcare professional is always advised.
FAQs
What is sciatica’s primary cause?
A pinched nerve that supplies the sciatic nerve might result in sciatica. Typically, an overgrowth of bone, commonly referred to as bone spurs, on the spinal bones or a herniated disc in the spine are the causes. Tumor pressure on the nerve is less common.
Which treatment for sciatica is most effective?
Additional self-care practices that could be beneficial are:
cool packets. Apply a cold compress to the sore spot many times a day for up to 20 minutes at a time.
Warm packets. Apply heat to the affected regions after two to three days.
stretching. Low back stretches may help relieve some of the pain.
Medications.
Does sciatica disappear?
Many sciatica cases resolve on their own in four to six weeks without the need for medical attention from a specialist. In addition, more severe cases could take weeks or months to recover, particularly if the symptoms are more severe.
Is sciatica a serious condition?
Even though it’s rare, sciatica symptoms and indicators could be warning signs for a variety of serious problems that need to be treated right away, such as surgery or medicine.
How can I naturally treat sciatica?
Many sciatica treatment methods necessitate mobility and general physical activity. To begin with, take quick steps outside in between times when you sit or lie down. Make it your mission to walk a greater distance each time. Also, remember to maintain proper posture whether you’re at work or home.
References
- Professional, C. C. M. (n.d.-h). Sciatica. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12792-sciatica
- Sciatica – Symptoms and causes – Mayo Clinic. (2024, January 31). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435
- Hochschuler, S., MD. (n.d.). What you need to know about Sciatica. Spine-health. https://www.spine-health.com/conditions/sciatica/what-you-need-know-about-sciatica
- What is sciatica? (2016, November 29). WebMD. https://www.webmd.com/back-pain/what-is-sciatica
- Gillott, C. (2023, December 21). What you need to know about sciatica. https://www.medicalnewstoday.com/articles/7619
- Sciatica – Diagnosis and treatment – Mayo Clinic. (2024, January 31). https://www.mayoclinic.org/diseases-conditions/sciatica/diagnosis-treatment/drc-20377441
- Sciatica – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/sciatica/
- Wiginton, K. (2005, February 21). Sciatica. WebMD. https://www.webmd.com/back-pain/sciatica-symptoms




23 Comments