Cervical Plexus
Introduction
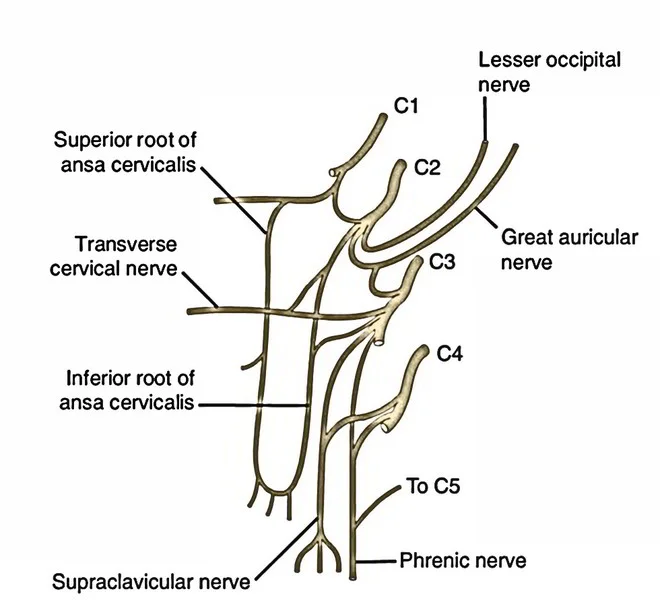
The cervical plexus is a collection of cervical nerves created by the anterior (ventral) rami of spinal nerves C1-C4 (sometimes known as the first through fourth cervical nerves). The cervical plexus’ roots (limbs) are shown here.
The 5th cervical nerve (the anterior ramus of spinal nerve C5) may also be regarded as a member of the plexus since it helps to produce one of the cervical plexus’ motor branches, the phrenic nerve. As a result, the cervical plexus may alternatively be characterized as a network of nerves created by the anterior rami of spinal nerves C1-C5, which produces both motor (deep) and sensory (superficial) branches.
Course
Sensory branches
Lesser occipital nerve: This branch is created only by the second cervical nerve (C2) and serves to feed the skin of the neck and scalp posterosuperior to the collarbone.
Great auricular nerve: This sensory branch is derived from the C2 and C3 nerves. It travels diagonally upwards, crossing the sternocleidomastoid muscle and ending at the parotid gland. It then separates and innervates the skin around the parotid gland, the posterior side of the auricle, and a region of skin that stretches from the mandibular angle to the mastoid process.
Transverse cervical nerve: The transverse cervical nerve is composed of axons from the second and third cervical nerves. It provides the skin that covers the front triangle of the neck. This branch curls around the center of the sternocleidomastoid muscle’s posterior border before crossing deep into the platysma muscle.
Supraclavicular nerves: These branches are produced from the C3 and C4 spinal neurons and emerge as a single trunk behind the sternocleidomastoid muscle. This separates into three smaller branches (medial, middle, and lateral) that reach the skin of the neck. Some branches cross the clavicle to supply skin on the shoulder.
Motor branches
The ansa cervicalis: The five motor branches of the ansa cervicalis loop mentioned above arise from the C1 to C3 nerves. The ansa cervicalis is made up of two roots, superior and inferior, created by fibers from the cervical spinal neurons’ anterior rami. They feed the infrahyoid muscles in the anterior cervical triangle.
The phrenic nerve: The phrenic nerve is primarily derived from the 4th cervical nerve (C4), with contributions from the 3rd and 5th cervical nerves (C3 and C5). It develops in the superior section of the lateral border of the anterior scalene muscle, near the superior border of the thyroid cartilage. The phrenic nerve has motor, sensory, and sympathetic nerve fibers. It supplies the diaphragm’s only motor supply as well as feeling in its middle region.
The phrenic nerve in the thorax innervates the mediastinal pleura and pericardium of the heart. The phrenic nerve descends obliquely across the anterior scalenus muscle, passing through the prevertebral layer of deep cervical fascia and the transverse cervical and suprascapular arteries. As it reaches the thorax, it passes anterior to the internal thoracic artery and posterior to the subclavian vein.
Function
The cervical plexus provides a network of branches that supply sensory and muscular innervation to regions in the head, neck, and trunk. Some branches also get input from cranial nerves, which innervate their respective tissues. The cervical plexus is two distinct plexuses, one superficial and the other deep.
The superficial plexus is made up of lateral terminal branches that form loops that give rise to the sensory branches of the cervical plexus, which include the great auricular nerve, the external auditory meatus, the transverse cervical nerve, and the lesser occipital and supraclavicular nerves. The deep plexus then divides into muscle branches, which include the ansa cervicalis, phrenic nerve, and other segmental branches.
Branches
Sensory
Motor branches feed muscles, whereas cutaneous branches innervate the skin of the anterolateral neck, the upper region of the thorax (superolateral thoracic wall), and the scalp between the auricle (pinna) and the external occipital protuberance.
The sensory (posterior or cutaneous) branches of the plexus arise around midway along the posterior edge of the sternocleidomastoid muscle. This location is clinically significant and recognized as the neck’s nerve point.
Four sensory branches emerge from the two loops created by the anterior rami of spinal nerves C2 and C3, and C3 and C4. They are:
Branches of the loop between C2 and C3:
- Lesser occipital nerve (formed by C2)
- Great auricular nerve (C2 and C3)
- Transverse cervical nerve (formed by C2 and C3)
Branches of the loop between C3 and C4:
Supraclavicular nerves (formed by C3 and C4)
The bolded letters in the names of the four sensory branches can be used to create a mnemonic for memorizing them. Thus, the mnemonic for the sensory branches is Let’s Go To Sleep.
Motor
On the other hand, the motor branches of the cervical plexus create the ansa cervicalis (C1-C3), a nerve loop that innervates the infrahyoid muscles in the anterior cervical triangle.
They also create the phrenic nerve (C3-5), which nourishes the diaphragm and pericardium of the heart. Additional muscular branches are also formed to supply innervation to the prevertebral, sternocleidomastoid, and trapezius muscles.
Susan Saw from Game of Thrones is a mnemonic for Ansa cervicalis.
- Sternohyoid nerve (C1 – C3)
- Sternothyroid nerve (C1 – C3)
- Geniohyoid nerve (via hypoglossal nerve) (C1)
- Omohyoid nerve (C1 – C3)
- Thyrohyoid nerve (via hypoglossal nerve) (C1)
Phrenic nerve (contributed mostly by C4, with minor contributions from C3 and C5)
Muscular branches for the prevertebral, sternocleidomastoid, and levator scapulae muscles
The mnemonic MAP (Muscular branches, Ansa cervicalis, Phrenic nerve) helps you recall the motor branches of the cervical plexus.
Embryology
The ventral roots of the spinal nerves originate in the mantle layer of the neural tube. In this mantle layer, neuroblast processes form rootlets that emerge in a continuous longitudinal series on the ventrolateral boundary of the neural tube.
The direction in which the ventral root fibers emerge from the tube varies depending on the size and position of the ganglion crest. The superficial cervical plexus is formed by the anterior branch fusion of C2 and C3, which produces the descendens cervicalis; this then connects in a loop with the hypoglossal nerve and, together with the first cervical nerve, forms the plexus. The deep plexus is composed of the lateral terminal branches. While the cervical plexus develops in a complicated manner, one important branch of the deep cervical plexus, the phrenic nerve, has been precisely documented throughout development.
During development, the diaphragm grows around the newly formed nerves. Some origins mention the phrenic nerve growing immediately ventral to the diaphragm during development. As the fetus grows, the locations of origin and insertion of the phrenic nerve gradually move apart due to the diaphragm’s drop and the elevation of the cervical nerves as other tissues in the neck develop.
Clinical Importance
Phrenic nerve severance
The phrenic nerve is severed (injured), resulting in diaphragmatic paralysis. A phrenic nerve block can cause temporary diaphragmatic paralysis. In this instance, an anesthetic is injected around the nerve, which is situated on the anterior surface of the anterior scalene muscle’s middle section. A surgical phrenic nerve crush will result in a prolonged duration of paralysis.
Cervical plexus block
A nerve block is a technique for inhibiting nerve impulse conductance, typically for regional anesthesia before surgical procedures. A cervical plexus block involves injecting an anesthetic substance at numerous sites along the posterior border of the sternocleidomastoid muscle, primarily at the intersection of its superior and middle thirds, which is the neck’s nerve point. Because the cervical plexus block paralyzes the phrenic nerve that supplies the diaphragm and pericardium, this technique is not performed on patients with pulmonary or cardiac illnesses.
Surgical Importance
Cervical plexus blocks are often used in this location to enhance anesthesia and as a regional pain block during neck surgeries. These operations include cervical fat pad biopsy, lymph node biopsy, and other superficial neck surgeries.
If performed appropriately, this sort of block provides anesthesia to the neck, occipital area, shoulder region, and upper pectoral region. To begin, to properly do this nerve block, an analgesic solution must be injected subcutaneously at the midpoint of the sternocleidomastoid’s posterior border. Anesthetized skin should be used to infiltrate the regions lateral to the transverse processes of the second, third, and fourth cervical vertebrae. It is critical to avoid intrathecal and intravascular injections while using this method. One case study also revealed injections into the phrenic and vagus nerves, while another demonstrated Horner syndrome as a result of this technique.
If more extreme surgical treatments are necessary, such as neck dissections, mass excision, thyroglossal cysts, trachea and laryngeal surgeries, and even carotid endarterectomy, local anesthetic must be supplied through the carotid sheath. This injection must be administered underneath the adventitia of the carotid bifurcation and into the superior angle of the incision. Unfortunately, thyroidectomies are seldom performed with this procedure since the bilateral blockage causes the patient to choke and increases the risk of bilateral phrenic blockade.
FAQs
What is the difference between the cervical plexus and the brachial plexus?
The cervical plexus sends nerves to the posterior head and neck, as well as the diaphragm. The brachial plexus sends nerves to the arm. The lumbar plexus provides nerves to the anterior leg.
What are the 4 major plexuses?
Cervical Plexus—Serves the Head, Neck, and Shoulders.
The brachial plexus connects the chest, shoulders, arms, and hands.
The Lumbar Plexus serves the back, belly, groin, thighs, knees, and calves.
The sacral plexus connects the pelvis, buttocks, genitals, thighs, calves, and feet.
What are the two types of cervical plexus?
The cervical plexus contains two branches, cutaneous and muscular. Cutaneous (4 branches): Lesser occipital nerve – innervates the skin and the scalp posterosuperior to the auricle (C2) Great auricular nerve – innervates skin near concha auricle (outer ear) and external acoustic meatus (ear canal) (C2-C3)
Does the phrenic nerve form part of the cervical plexus?
The phrenic nerve originates in the cervical spinal roots C3, C4, and C5. This may be recalled using the limerick, “C3, 4, and 5 keep the diaphragm alive”. The primary contribution comes from the spinal root C4, with minor contributions from C3 and C5, as well as some connecting fibers from the cervical plexus.
What is the neck muscle called?
Sternocleidomastoid muscle
The sternocleidomastoid is a big, two-headed muscle in the neck. The clavicular head develops from the medial portion of the clavicle, while the sternal head develops from the sternum’s manubrium.
References
- Cervical plexus. (2023, June 15). Kenhub. https://www.kenhub.com/en/library/anatomy/cervical-plexus
- Cervical plexus. (2023, July 24).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK538514/