Glanohumeral Ligament
Introduction:
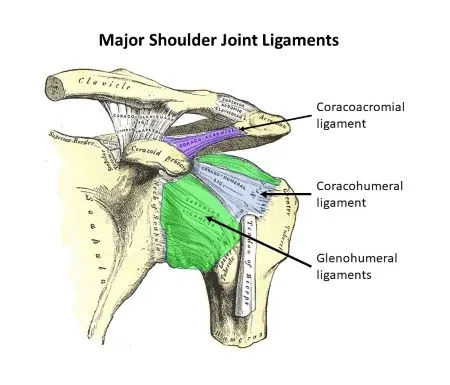
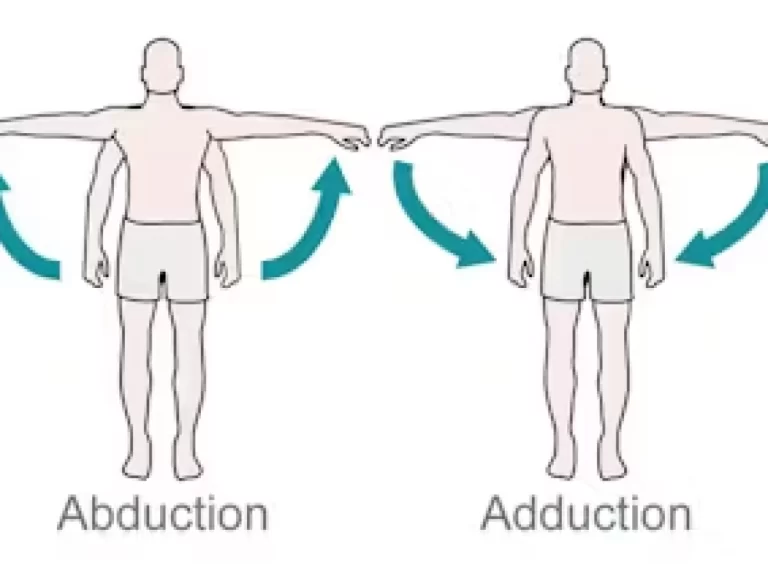
The glenohumeral ligaments are a group of three ligaments (superior, middle, and inferior) that reinforce the shoulder joint, connecting the humerus to the glenoid cavity of the scapula. They provide stability by limiting excessive movement and preventing dislocation, particularly during shoulder rotation and abduction.
They are also in charge of preventing the humerus bone from moving too much within the joint. Glenohumeral ligament injuries can cause shoulder instability and dislocation, which can be severe painfull and restrict range of motion. To address such injuries, physical therapy, rehabilitation activities, and surgery can be necessary.
Structure of the Glanohumeral Ligament:
The superior, middle, and inferior glenohumeral ligaments are the three separate ligaments that make up the complex glenohumeral ligament. These ligaments are found in the shoulder joint, a ball-and-socket joint that joins the scapula (shoulder blade) and humerus (upper arm) bones.
The apex of the shoulder joint is home to the smallest of the three ligaments, the superior glenohumeral ligament. It extends from the greater tubercle of the humerus, a bony protrusion on the upper portion of the bone, to the top of the glenoid fossa, a shallow dip on the scapula that serves as the socket for the humerus bone. The humerus bone’s excessive upward mobility within the joint is limited by the superior glenohumeral ligament.
The glenoid fossa and the lesser tubercle of the humerus a tiny bony protuberance on the top portion of the bone are connected by the middle glenohumeral ligament, which is situated in the middle of the shoulder joint. In order to keep the humerus bone from anteriorly dislocating that is, moving forward out of its socket the middle glenohumeral ligament is essential.
The largest and strongest of the three ligaments, the inferior glenohumeral ligament is situated near the base of the shoulder joint. The axillary pouch, posterior band, and anterior band are its three separate bands. The anterior band extends from the glenoid fossa’s front to the humerus bone’s front, while the posterior band extends from the glenoid fossa’s rear to the humerus bone’s rear. Between the two bands is a little structure that resembles a pocket called the axillary pouch. The humerus bone can slip rearward out of its socket, a condition known as posterior dislocation, which is prevented in part by the inferior glenohumeral ligament.
Thus, we may conclude that the glenohumeral ligament is an important component that aids in shoulder joint stability and dislocation prevention. Glenohumeral ligament injuries can cause severe pain and severely restrict movement. Surgery, physical therapy, and rehabilitation activities may be used to treat these diseases.
Functions of the Glanohumeral Ligament:
One of the most important parts of the shoulder joint, the glenohumeral ligament serves a number of vital purposes. Among these are the following:
- Shoulder Joint Stabilization: The glenohumeral ligament’s main works is to keep the shoulder joint stable. The ligament restricts the humerus’s excessive mobility in all directions by acting as a restraining force. This is particularly crucial for overhead activities that put a lot of stress and strain on the shoulder joint, such throwing a ball or lifting weights.
- Preventing Dislocation: The glenohumeral ligament is essential for keeping the shoulder joint from dislocating. The glenoid fossa, a tiny indentation in the scapula or shoulder blade, is where the ligament connects the humerus. The humerus is kept firmly in place and doesn’t slip out of the socket thanks to this connection.
- Force Distribution: The glenohumeral ligament aids in the distribution of forces across the shoulder joint. Forces produced during exercise have the potential to put stress and strain on the joint. By distributing these stresses uniformly throughout the joint, the ligament lowers the chance of damage and encourages effective mobility.
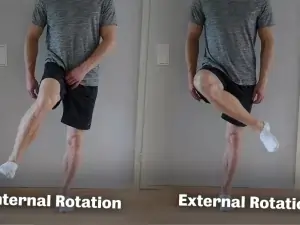
- Restricting Excessive Movement: The three components of the glenohumeral ligament each play a distinct work in preventing the humerus from moving too much. While the intermediate ligament restricts outward rotation, the superior ligament stops the humerus from moving too much upward. The humerus cannot move downward because of the inferior ligament, which is the strongest and thickest of the three.
Ultimately, the glenohumeral ligament plays a critical role in preserving the shoulder joint’s stability and functionality. Its duties include minimizing excessive humeral movement, distributing pressures throughout the joint, stabilizing the joint, and preventing dislocation. The shoulder joint would be brittle and vulnerable to damage without this ligament.
Blood supply of the Glanohumeral Ligament:
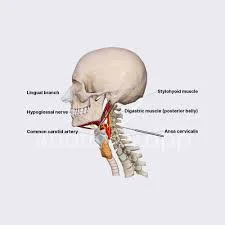
Attaching the humerus bone to the glenoid fossa of the scapula bone in the shoulder joint is the glenohumeral ligament, a complex of three ligaments. The circumflex scapular artery and the suprascapular artery are the two primary blood vessels that give blood to the glenohumeral ligament.
The subscapular artery, a branch of the axillary artery, gives birth to the circumflex scapular artery. It supplies the muscles and soft tissues surrounding the shoulder joint by a number of branches as it follows the lateral border of the scapula. The upper portion of the glenohumeral ligament is supplied by the ascending branch, one of these branches.
The thyrocervical trunk, a branch of the subclavian artery, is where the suprascapular artery originates. It passes through the scapula’s suprascapular notch and splits into multiple branches that nourish the soft tissues and muscles surrounding the shoulder joint. The lower portion of the glenohumeral ligament is supplied by the ascending branch, one of these branches.
Smaller arteries also contribute to the glenohumeral ligament’s blood flow in addition to these two primary sources. Among these are branches from the anterior humeral circumflex artery, a branch of the axillary artery, and the posterior circumflex humeral artery, a branch of the axillary artery.
In summary, the glenohumeral ligament has a deep and wide-ranging blood supply that supplies enough oxygen and nutrients to sustain its structure and ability to support the shoulder joint.
Injuries of the Glanohumeral Ligament:
Glenohumeral ligament damage can result from a number of activities, such as:
- Sports injuries: Overhead sports like tennis, baseball, and volleyball, as well as contact sports like football, hockey, and rugby, can strain the shoulder joint and raise the risk of ligament damage.
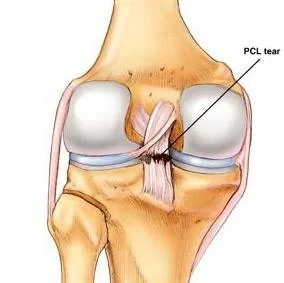
- Falls: The humerus bone may dislocate from the glenoid fossa if a person falls onto their shoulder or an outstretched arm, damaging the ligaments.
- Car accidents: Ligament damage may result from the shoulder joint dislocating or subluxating due to the abrupt impact of an automobile accident.
- Repetitive strain: The glenohumeral ligament can get injured over time due to wear and tear from repeated overhead movements, such as those needed for swimming, painting, or construction.
- Degenerative diseases: Rheumatoid arthritis and osteoarthritis can erode the shoulder joint’s ligaments, making injuries more likely.
- Poor lifting technique: Poor lifting technique increases the risk of ligament injury and puts undue strain on the shoulder joint.
If you experience any of the signs of a glenohumeral ligament injury, including shoulder pain, weakness, instability, or a noticeable deformity in the joint, it is imperative that you get medical attention. Depending on the extent of the damage, treatment options may include physical therapy, medication, surgery, or rest.
Symptoms of the Glanohumeral Ligament:
Depending on the extent and location of the injury, glenohumeral ligament symptoms can change. Typical symptoms include the following:
- Shoulder Pain: The most typical sign of a glenohumeral ligament damage is pain. The pain might be mild to severe and can come on suddenly or gradually. Usually located in the front or rear of the shoulder, the pain may get greater when you move.
- Swelling: Another typical sign of a glenohumeral ligament injury is swelling around the shoulder joint. It could be hard to move the arm because of the mild or severe edema.
- Another common sign of a glenohumeral ligament injury is stiffness in the shoulder joint. In addition to making it difficult to move the arm, the rigidity may cause pain.
- Weakness: Another typical sign of a glenohumeral ligament damage is weakness in the shoulder joint. It could be challenging to lift things or carry out regular tasks because of the weakness.
- Instability: Another typical sign of a glenohumeral ligament injury is instability in the shoulder joint. It can be quite painful if the shoulder seems loose or dislocated due to the instability.
- Clicking or popping sounds: A glenohumeral ligament injury may also result in clicking or popping sounds in the shoulder joint. Pain may accompany these sounds, which may happen when you move.
It’s critical that you get medical help from a qualified practitioner who can accurately evaluate and treat your injuries if you encounter any of these symptoms. Depending on the extent of the damage, treatment options may include medication, physical therapy, surgery, or rest.
Risk factors of the Glanohumeral Ligament:
A collection of ligaments called the glenohumeral ligament joins the scapula and humerus bones in the shoulder joint. These ligaments give the joint stability and guard against injuries like dislocation. However, the chance of suffering a glenohumeral ligament injury can be raised by a number of risk factors. These consist of:
- Trauma: The glenohumeral ligament may sustain damage as a result of trauma to the shoulder joint, such as a fall or sports injury.
- Swimming and throwing a ball are two examples of activities that can cause repetitive overhead motions, which over time can strain the glenohumeral ligament.
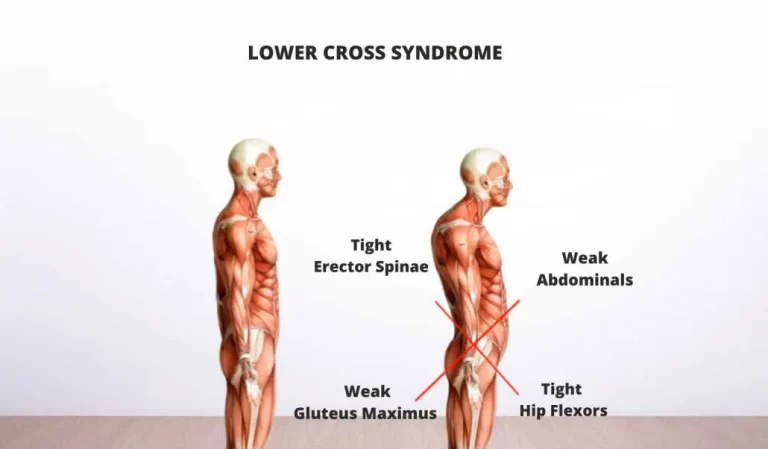
- An increased risk of glenohumeral ligament damage can result from poor posture, which can lead to imbalances in the muscles surrounding the shoulder joint.
- Muscle weakness or tightness: The glenohumeral ligament is more susceptible to injury if the muscles surrounding the shoulder joint are weak or tight.
- Aging: As we age, the shoulder joint’s ligaments and other tissues may deteriorate and become more vulnerable to damage.
- Genetics: Some people may be more susceptible to glenohumeral ligament problems due to their genetic makeup.
- Prior injuries: People with a history of shoulder joint injuries may be more susceptible to glenohumeral ligament issues in the future.
All things considered, lowering these risk factors is crucial to avoiding glenohumeral ligament damage and preserving the best possible shoulder joint health. This can entail maintaining proper posture, adding strengthening and stretching exercises to your regimen, and steering clear of activities that overstress the shoulder joint.
Diagnosis of the Glanohumeral Ligament:
Examination test:
The sulcus test:
- The glenohumeral ligament, which joins the humerus bone to the glenoid fossa of the scapula in the shoulder joint, is evaluated for integrity using the sulcus test, a physical examination procedure. The patient sits with their arm relaxed at their side, and the test is conducted by providing downward traction on the arm.
- The examiner uses one hand to grasp the patient’s elbow and the other to hold the patient’s wrist in order to do the sulcus test. After that, the examiner pushes the arm downward to separate the glenoid fossa from the humeral head. The skin covering the lateral aspect of the shoulder joint develops a noticeable sulcus or depression as a result of this gap.
- The sulcus’s width and depth are noted by the examiner, along with any pain or suffering the patient may have expressed during the test. Greater laxity or instability of the glenohumeral joint is indicated by a deeper and wider sulcus, which could be a sign of a glenohumeral ligament tear or injury.
- To evaluate shoulder instability and choose the best course of action, the sulcus test is frequently combined with additional physical examination methods like the relocation and apprehension tests.
The anterior drawer test:
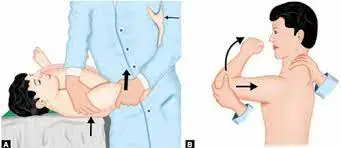
- A unique test for determining anterior glenohumeral ligament laxity is the anterior drawer test. It is frequently carried out on patients who have had shoulder dislocations or who exhibit signs of shoulder joint instability.
- The patient’s arm is relaxed at their side while they are seated or in a supine position for the examination. Standing in front of the patient, the examiner uses one hand to stabilize the scapula and the other to hold the patient’s elbow. In order to check for excessive movement or “drawer” motion, the examiner then applies a forward push to the humeral head.
- Anterior glenohumeral ligament damage may be indicated if the humeral head’s anterior translation is greater than that of the contralateral side. Instability and a higher chance of shoulder dislocation may result from this.
- To check for various glenohumeral ligament injuries, the anterior drawer test is frequently used in combination with other specialized tests. Depending on the kind and degree of the injury, treatment options may involve bracing, physical therapy, or surgery.
The posterior drawer test:

- A unique test for determining posterior glenohumeral ligament flexibility is the posterior drawer test. It is frequently done on individuals who have had shoulder trauma or who exhibit signs of shoulder joint instability.
- The patient’s arm is relaxed at their side while they are seated or in a supine position for the examination. Standing behind the patient, the examiner uses one hand to stabilize the scapula and the other to hold the patient’s elbow. After that, the examiner pushes the humeral head back while looking for any “drawer” or excessive movement.
- The posterior glenohumeral ligament may be damaged if the humeral head’s posterior translation is greater than that of the contralateral side. Instability and a higher chance of shoulder dislocation may result from this.
- To check for various glenohumeral ligament injuries, the posterior drawer test is frequently used in combination with other specialized tests. Depending on the kind and degree of the injury, treatment options may involve bracing, physical therapy, or surgery.
- It is crucial to remember that only a qualified healthcare practitioner who is conversant with the methodology and result interpretation should conduct the posterior drawer exam.
Treatment of the Glanohumeral Ligament:
Medical Treatment:
- The ligament that joins the humerus bone to the scapula’s glenoid fossa in the shoulder joint is called the glenohumeral ligament. Shoulder pain and instability can be caused by damage to this ligament. Glenohumeral ligament injuries may be treated conservatively using the following options:
- Rest and immobilization: You can lessen inflammation and speed up recovery by resting the injured shoulder and avoiding activities that make it worse. To stop more damage, immobilization with a brace or sling might also be required.
- Physical therapy: Physical therapy can assist increase shoulder joint stability, strength, and range of motion. To enhance balance and coordination, exercises can involve proprioception training, strengthening, and stretching.
- Non-steroidal anti-inflammatory medicines (NSAIDs): Ibuprofen and naproxen are two examples of over-the-counter NSAIDs that can help lessen the pain and inflammation caused by glenohumeral ligament injuries.
- Injections of corticosteroids: Corticosteroid injections directly into the shoulder joint can help lessen pain and inflammation.
- In order to encourage healing, platelet-rich plasma (PRP) therapy entails injecting platelet-rich plasma which is made from the patient’s own blood—into the injured area.
- It is crucial to remember that not all glenohumeral ligament injuries may be successfully treated with conservative measures. In certain cases, reconstructing or repairing the injured ligament may need surgery. Speaking with a medical expert is essential when determining the best course of action for a given situation.
Physical Therapy Treatment:
Exercises and manual therapy methods are commonly used in physical therapy to address glenohumeral ligament problems. Reducing pain and inflammation, increasing strength and range of motion, and stabilizing the shoulder joint are the main objectives of physical therapy.
- Evaluation: A comprehensive evaluation of the shoulder joint is the initial stage in physical therapy treatment for a glenohumeral ligament injury. This could involve a thorough history of the injuries, imaging studies like MRIs or X-rays, and a physical examination.
- Rest and immobilization: To stop additional damage and give the ligament time to heal, the affected shoulder may need to be immobilized with a brace or sling.
- Shoulder joint pain and stiffness can be lessened with manual therapy techniques such massage, joint mobilization, and soft tissue mobilization.
- Range of motion activities: The purpose of range of motion exercises is to increase shoulder joint mobility and flexibility. These workouts could involve passive range-of-motion exercises, pendulum exercises, and stretching.
- Strengthening exercises: The purpose of strengthening exercises is to increase the shoulder joint’s stability and strength. Weightlifting, isometric exercises, and resistance band exercises are a few examples of these workouts.
- Enhancing balance and coordination in the shoulder joint is the goal of proprioception training. Exercises like standing on one leg or using a wobble board may be part of this.
- Functional training: To assist patients in returning to their regular activities, functional training entails workouts that replicate everyday tasks and motions unique to sports.
- Education: Patients may also be given instruction on how to avoid future injuries, good body mechanics, and right posture.
As a result, physical therapy for glenohumeral ligament injuries is ultimately customized to meet the demands of each patient. To create a customized treatment plan that targets the patient’s unique symptoms and objectives, a physical therapist will collaborate closely with the patient.
How to Prevent Glenohumeral ligament Injuries:
Maintaining ideal shoulder joint health and preventing pain and discomfort require preventing glenohumeral ligament injuries. The following actions can help you avoid glenohumeral ligament injuries:
- Maintaining proper posture can assist to avoid imbalances in the muscles surrounding the shoulder joint, which lowers the chance of glenohumeral ligament damage. Keep your shoulders back and down when standing or sitting, and never slouch.
- Include stretching and strengthening exercises: These can help increase the strength and flexibility of the muscles surrounding the shoulder joint, lowering the chance of glenohumeral ligament damage. Shoulder stretches, shoulder rolls, and rotator cuff strengthening exercises are a few beneficial activities.
- Keep away of recurrent overhead motions: Over time, repetitive overhead motions, such swimming or throwing a ball, can strain the glenohumeral ligament. To lower your chance of injury, make sure to stretch frequently and take pauses if you engage in these activities.
- Use appropriate technique: To lower the chance of injury, use appropriate technique when playing sports or engaging in other activities that need the shoulder joint. For instance, utilize good form and refrain from exerting oneself too much when tossing a ball.
- Keep your weight within a healthy range because carrying too much weight might strain your shoulder joint and increase your risk of glenohumeral ligament damage. One way to lower this risk is to keep your weight in check.
- Prevent past injuries: Take precautions to avoid further injuries if you have already suffered a shoulder joint injury. This can entail staying away from activities that overstress the shoulder joint or using protective gear when playing sports or engaging in other activities.
All things considered, preventing glenohumeral ligament injuries can assist to preserve the best possible health of the shoulder joint and lower the likelihood of pain and discomfort. To avoid such injuries, make sure to get medical help if you feel any pain or discomfort in your shoulder joint.
FAQs
For stability, which glenohumeral ligament is most crucial?
While the inferior glenohumeral ligament complex is the most crucial stabilizer against anteroinferior shoulder dislocation, the middle glenohumeral ligament offers anterior support at 45 and 60 degrees abduction. As a result, this part of the capsule sustains injuries the most often.
How is a sprained glenohumeral ligament treated?
Injections, physical or occupational therapy, immobilization, and rest are among possible treatments for shoulder sprains and strains. If a shoulder sprain or strain is serious, our specialists might suggest surgery. A shoulder sprain or strain may be less painful with rest, ice, immobilization, or injections.
What motion is inhibited by the glenohumeral ligament?
Internal rotation and anterior translation of the humeral head (posterior portion) are restricted by the inferior glenohumeral ligament, which also restricts external rotation and superior and anterior translation of the humeral head (anterior portion).
What is the strongest glenohumeral ligament?
The inferior glenohumeral ligament is the most significant and robust. Constant, the superior band extends outward and downward beneath the middle glenohumeral ligament.
Which muscles provide glenohumeral joint protection?
The rotator cuff muscles are the main muscle group responsible for supporting the shoulder joint. The teres minor, subscapularis, supraspinatus, and infraspinatus are the four rotator cuff muscles.
Which four glenohumeral ligaments are there?
Ligaments of the glenohumerus The glenohumeral joint capsule, which connects the glenoid fossa to the humerus, is made up of the superior, middle, and inferior ligaments.
How are the glenohumeral ligaments strengthened?
Slide for the wall
Lean forward until one arm hangs straight down, supported by a table or chair. For support, rest your other hand on the chair or table.
As though painting a circle with your hand, slowly rotate your free arm clockwise, changing direction occasionally. Increase the circle’s size gradually.
What is the glenohumeral ligament’s biomechanics?
The main static stabilizers are the glenohumeral ligaments, which thicken the joint capsule. They merely tighten at the end ranges of motion to permit a high degree of shoulder mobility.
How is a damaged glenohumeral ligament treated?
In addition to the foregoing treatment methods, a sling may be worn for three to four weeks in cases of a partially torn shoulder ligament tear (Grade 2) to allow the shoulder ligament to mend properly. Shoulder ligament tears that are entirely torn (Grade 3) may need to be repaired surgically in order to rejoin the ligament.
How is an injury to the glenohumeral ligament treated?
Rest, ice, physical therapy, anti-inflammatory drugs, and in extreme situations, surgery, are all possible treatments for glenohumeral ligament injuries.
How may an injury to the glenohumeral ligament be identified?
A physical examination, imaging tests like MRIs or X-rays, and maybe an arthroscopy can all be used to accurately identify a glenohumeral ligament injury.
What signs of a glenohumeral ligament damage are present?
Injuries to the glenohumeral ligament can cause shoulder pain, edema, stiffness, weakness, and instability.
What may result in glenohumeral ligament damage?
A glenohumeral ligament injury may result from repetitive strain, trauma, or overuse. Shoulder joint subluxation or dislocation may also be the reason.
What is the glenohumeral ligament’s primary purpose?
The glenohumeral ligament keeps the humerus bone from moving too much and stabilizes the shoulder joint.
The glenohumeral ligament: what is it?
A collection of ligaments known as the glenohumeral ligament connects the humerus bone to the scapula’s glenoid fossa at the shoulder joint.
References
- Patel, D. (2023c, August 11). Glanohumeral ligament – Anatomy, structure, function. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/glanohumral-ligament/