Pyogenic Flexor Tenosynovitis
Introduction
Pyogenic Flexor Tenosynovitis (PFT) is a bacterial infection of the flexor tendon sheath in the hand, typically caused by Staphylococcus aureus. It results from penetrating trauma, bites, or hematogenous spread.
The condition is characterized by Kanavel’s four cardinal signs: finger flexion at rest, fusiform swelling, tenderness along the tendon sheath, and pain with passive extension. PFT is a surgical emergency requiring prompt antibiotic therapy and, often, surgical drainage to prevent tendon necrosis and hand dysfunction.
A closed-space infection of the hand’s flexor tendon sheath, pyrogenic flexor tenosynovitis (PFT), often referred to as septic or suppurative flexor tenosynovitis, continues to be a difficult issue in the field of hand surgery. PFT is still a prevalent issue, accounting for 2.5 to 9.4% of all hand infections, according to research.
PFT can result in tendon necrosis and finger devitalization, and is responsible for 2.5% to 9.5% of hand infections. This infection causes adhesions within the flexor tendon sheath and changes the gliding mechanism, significantly impairing finger movement.
Although bloodstream infections can induce PFT, penetrating finger injuries involving the flexor tendon sheath are typically the culprit. The three main symptoms of pyogenic flexor tenosynovitis were identified in 1912: painful passive digital extension, flexor sheath soreness, and a flexed posture of the affected finger. Fusiform swelling of the digit was then included as a fourth sign, making the four cardinal signs.
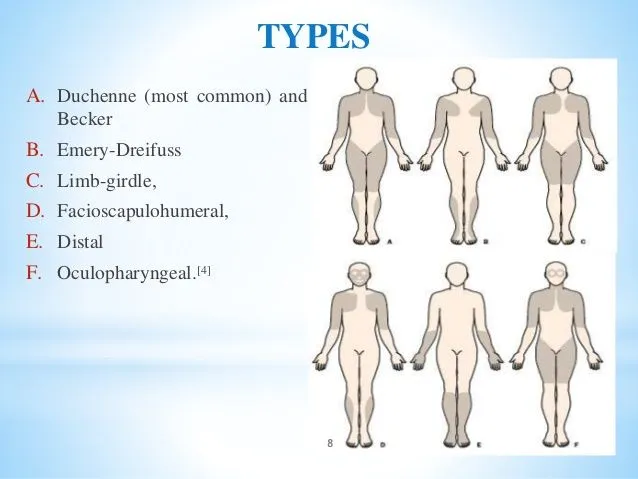
Anatomy
- Although the anatomy of the flexor tendon sheath varies greatly, there are certain commonalities.
- The distal sheaths in the fingers end at the FDP insertion, which is close to the DIP joint.
- The sheath in the thumb ends where the FPL is inserted, which is close to the IP joint.
- The sheaths often reach only proximal to the A1 pulley (close to the MCP joint). Usually, the sheaths of the thumb and small finger connect to the radial and ulnar bursae.
- A horseshoe abscess may emerge from an infection that travels from the little finger to the thumb or the other way around.
Pathogenesis
The pathogenesis of pyogenic flexor tenosynovitis (PFT) involves a bacterial infection within the closed space of the hand’s flexor tendon sheath. This is usually caused by a penetrating injury that allows bacteria to enter the sheath directly, resulting in inflammation, pus accumulation, and possibly tendon damage.
If treatment is delayed, the infection can spread quickly because the hand’s tendon sheaths are interconnected, and the most common causative bacteria are Staphylococcus aureus and other skin flora.
Stages of pyogenic flexor tenosynovitis
Michonne divided PFT into three phases according to the infection’s severity:
- Stage 1: The flexor sheath begins to fill with serous exudate
- Stage 2: Purulent fluid fills the sheath.
- Stage 3: Necrosis is evident in the flexor tendon, flexor sheath, and pulley system.
Causes
Although bacteria are typically the source of both infections, the infection pathway may vary. While osteomyelitis can be caused by a direct wound, hematogenous spread (via the circulation), or contiguous transmission from an adjacent infection, pyogenic flexor tenosynovitis frequently results from a penetrating lesion to the hand.
- Penetrating trauma: PFT can result from bites, puncture wounds, and lacerations to the finger.
- Bits: PFT can be caused by Pasteurella multocida from an animal bite and Eike Nella corrodes from a human bite.
- Bloodstream infection: Hematogenous spread may be the cause of PFT.
Signs and Symptoms
Kanavel’s signs:
Clinicians often use the classic “Kanavel signs” to diagnose pyogenic flexor tenosynovitis, including:
- Fusiform swelling of the finger
- Tenderness along the flexor tendon sheath
- Pain with passive extension of the finger
- Flexed posture of the affected digit
- Loss of motion
- Tendon rupture
- Soft tissue necrosis
- Amputation
Risk factor
Found that the following risk factors, particularly the amputation rate and its impact on total active motion, were associated with deteriorating clinical outcomes in a sample of 75 PFT patients:
- Diabetes
- Peripheral vascular disease
- Renal failure
- Age over 43 years
- Subcutaneous purulence
- Digital ischemia
- Polymicrobial infection
- IV drug use
- Immunocompromised patients
Diagnosis
- X-ray

To rule out any retained foreign body, x-rays of the hand taken in the anteroposterior, lateral, and oblique views should be acquired. The acquired x-rays show evidence of osteomyelitis, which points to a persistent infection. Uniform finger swelling did not differentiate PFT from other hand infections, according to a retrospective analysis of adult finger infections. Additionally, they stated that at the level of the proximal phalanx, PFT is distinguished by a difference in radiographic soft tissue thickness between the volar and dorsal aspects.
- Hand ultrasonography
Hand ultrasonography is a low-cost, noninvasive technique for confirming the diagnosis of PFT. Ultrasonography can see the flexor tendon and identify any fluid buildup inside the flexor sheath. In addition to assisting the clinical examination in identifying finger infections, ultrasound offers an excellent negative predictive value and specificity for diagnosing PFT. Nevertheless, the ultrasound depends on the operator and cannot distinguish between blood and pus.
- Magnetic resonance imaging (MRI)
PFT is infrequently diagnosed with magnetic resonance imaging (MRI). While MRI can determine the degree of the infection, it is unable to distinguish PFT from other inflammatory diseases.
Because the ratio of tendon sheath to tendon width in the coronal and sagittal planes was shown to increase objectivity, contrast-enhanced computed tomography of the hand has also been claimed to be useful in detecting PFT.
- Laboratory test
Patients with PFT typically have higher levels of inflammatory indicators, such as erythrocyte sedimentation rate, C-reactive protein, and white blood cell count. Although these tests cannot specifically diagnose PFT, they can be useful in tracking infection and treatment response.
To determine the causal organism and guide antibiotic therapy based on sensitivity, pus and necrotic tissue cultures are highly helpful. To isolate the causal organism, get a blood culture if there are indications of sepsis or hematogenous infection spread.
Differential Diagnosis
Felon (Distal Pulp Space Infection)
The thumb or index finger are frequently affected by felon, a closed space infection of the distal finger pulp. Staphylococcus aureus infections resulting from penetrating injury to the fingertip pulp are typically the cause of felon or pulp space infections. However, in immunocompromised people, this illness may be caused by gram-negative bacteria or a variety of species.
When infected, the fibrous septa, which run from the distal phalanx periosteum to the skin from a confined area, produce excruciating throbbing pain. A surgical incisional drainage is necessary for a felon who presents with a severe, throbbing abscess over the distal finger phalanx.
Interphalangeal Joint or Metacarpophalangeal Joint Septic Arthritis
Signs of infection specific to the affected joint are typically evident in these two arthritic diseases. Because of joint effusion and capsular distention, the affected joint’s range of motion is typically limited and painful. Usually lacking are the other cardinal Kanavel symptoms of PFT, such as flexor sheath pain and finger fusiform edema.
Herpes simplex virus (HSV)
The herpes simplex virus is the source of this uncommon viral infection of the fingertips. Herpetic whitlow is characterized by painful blisters that may eventually develop bullae and are filled with a clear fluid. Antiviral drugs like acyclovir are necessary for treating herpes whitlow; surgery is not necessary.
Bacterial infection
Diffuse hand inflammation without underlying pus accumulation is called hand cellulitis. Hand cellulitis manifests as erythema and widespread swelling without the development of an abscess. Depending on the causative organism, high arm elevation and intravenous antibiotics can be used to treat hand cellulitis.
Treatment
Medical treatment
Cultures and antibiotic treatment beginning initially with a cephalosporin are also required. A cephalosporin should be replaced by trimethoprim/sulfamethoxazole, clindamycin, doxycycline, or linezolid in regions where methicillin-resistant Staphylococcus aureus (MRSA) is common.
In the end, microbiology and, if available, susceptibility data should inform the antibiotic selection. If a mycobacterial or fungal infection is suspected, the microbiology lab should be notified.
- Amoxicillin + clavulanic acid: This is often the preferred oral antibiotic for PFT.
- Cephalosporins: These are often the initial antibiotic used to treat PFT.
- Trimethoprim: This is sometimes used in areas where methicillin-resistant Staphylococcus aureus (MRSA) is common.
- Following surgery, oral antibiotics are administered for two to six weeks.
- To lessen stiffness and adhesion formation, supervised therapy is initiated.
Physical therapy treatment
To restore hand function while minimizing additional inflammation and pain, physical therapy treatment for pyogenic flexor tenosynovitis primarily consists of gentle range-of-motion exercises after the acute infection has been controlled with antibiotics and surgical drainage. This often involves splinting to rest the affected tendons and gradually increasing the exercises as tolerated.
It is important to remember that pyogenic flexor tenosynovitis is a medical emergency that requires immediate surgical intervention and antibiotic treatment; physical therapy should only be started after the acute infection has been managed by a healthcare professional.
Rest and splinting
To limit movement and aid in healing, the injured hand will first be immobilized with a splint; the splint may be adjusted as tolerated to permit greater range of motion.
- Elevation: Swelling can be lessened by keeping the injured hand up above the level of the heart.
- Ice application: Using ice packs can aid in the management of inflammation and pain.
Gentle active range-of-motion exercises
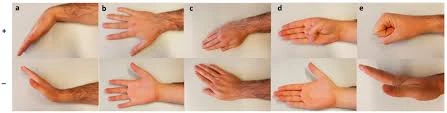
With an emphasis on flexion and extension movements, the physical therapist will gradually increase the range of motion in the fingers and hand by introducing mild active exercises once the acute irritation has subsided.
Tendon gliding exercises
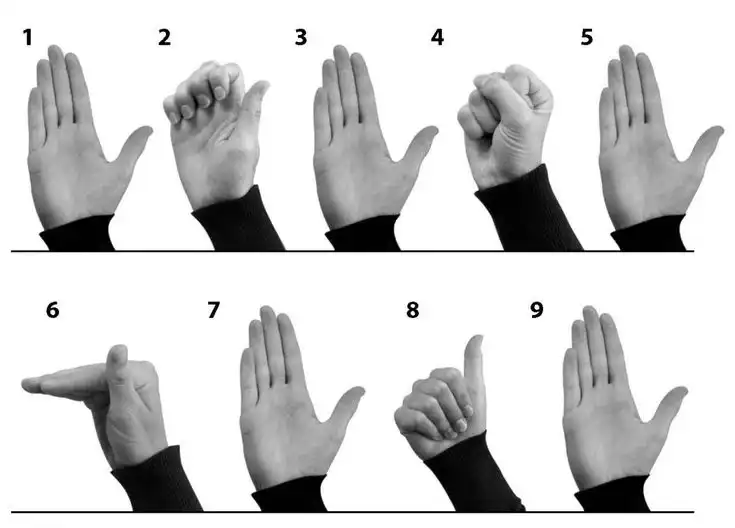
By gently moving the tendons back and forth within their sheath, these workouts seek to reduce friction within the tendon sheath.
Phase 1 (Early stage):
- Gentle finger extensions and flexions within a pain-free range.
- Tabletop position with slight finger spread.
- Hook position with minimal finger flexion.
Phase 2 (Moderate stage):
- Full range of motion in tabletop, hook, and fist positions.
- Adding wrist flexion and extension movements.
Phase 3 (Advanced stage):
- Incorporating light resistance exercises using hand therapy tools.
- Functional activities like picking up small objects or gripping a soft ball.
Isometric exercises
In the early phases of rehabilitation, isometric workouts can assist in minimizing joint movement and preserve muscle strength.
Soft tissue mobilization
Soft tissue limitations can be addressed and blood flow to the area improved with the use of gentle massage techniques.
Surgical treatment
Open Irrigation
The flexor sheath is exposed and washed out during open surgery for pyogenic flexor tenosynovitis (PFT). Open flexor sheath irrigation and debridement is the term for this process. It is used to treat persistent tenosynovial infections and advanced infection cases.
Procedure
- Cut through the injured finger’s palm or mid-axial region.
- Determine and safeguard the affected finger’s neurovascular bundle.
- Cut the flexor sheath’s A1 and A5 pulleys.
- Use saline to debride and rinse the sheath.
- Prevent the flexor tendon from bowstringing by protecting the A2 to A4 pulleys.
Closed Tendon Sheath Irrigation
A cut is performed above the metacarpal neck in the proximal direction. The proximal border of the A1 pulley is where the tendon sheath is transversely sliced. An angiocatheter is placed into the flexor tendon sheath 1–2 cm antegrade.
Next, on the radial aspect of the thumb or the ulnar aspect of the finger, a distal midfacial incision is made dorsal to the neurovascular bundle at the level of the distal interphalangeal joint.
Distal to the distalmost pulley, the flexor sheath’s distal edge is exposed and resected. To keep the wound open and for fluid drainage, a Penrose drain can be inserted into the tendon sheath underneath the A4 pulley. It is possible to maintain intermittent bedside irrigation on the floor following surgery.
Catheter irrigation
Pyogenic flexor tenosynovitis can be surgically treated using catheter irrigation, which involves flushing the tendon sheath with fluid infused with antibiotics. This serves as a substitute for open surgical drainage.
Procedure
- The flexor sheath is accessed through a little incision.
- The sheath is filled with a catheter.
- Fluid infused with antibiotics is used to irrigate the sheath.
- A solution of antibiotics is used to wash the tendons.
- The wounds are sealed.
Benefits
- Not as painful as open surgical drainage
- Reduces scarring and produces smaller wounds.
- It could facilitate a quicker return to normal.
Prognosis
If proper treatment is not started as soon as possible, PFT may lead to severe outcomes with finger amputation and spread infection. The full active range of motion may not be regained by 10% to 25% of the affected patients. Following PFT, patients with peripheral vascular disease, diabetes mellitus, and renal failure are more likely to have their fingers amputated.
Complications
Fingers Stiffness and Restricted Range of Motion
Flexor tendon adhesions, larger joint capsules, and damaged pulleys can all be consequences of PFT’s inflammatory process. To reduce the chance of stiffness, suggest early physical workouts for the injured finger. After the inflammatory process has completely subsided, flexor tenolysis of the affected digit could be necessary to restore range of motion.
Flexor Tendon Scarring and Subsequent Rupture
Blood flow and nutrients to the flexor tendon are hampered by the high pressure inside the flexor sheath. Scarred, unhealthy flexor tendons become less elastic and can burst with more exercise.
Soft Tissue Necrosis and Finger Ischemia
The affected finger may experience critical ischemia as a result of arterial thrombosis caused by the inflammatory process or as a result of the blood flow being interrupted by the high pressure in the finger.
Hand Horseshoe Abscess
In patients with communicating ulnar and radial bursae, the infection from PFT of the thumb or little finger may spread, leading to the formation of a horseshoe-shaped abscess.
Finger Amputation
A severe infection, extensive soft tissue damage, or a stiff, functionless finger may necessitate amputation at different levels.
Stiffness
A bacterial infection known as pyogenic flexor tenosynovitis (PFT) can result in stiffness and decreased finger movement. If treatment is not received, this serious infection may result in amputation.
Spread of infection
Because the flexor tendon sheaths are interconnected, pyogenic flexor tenosynovitis (PFT) can spread quickly inside the hand. If treatment is not received, the infection may spread to the palm, forearm, and potentially additional digits.
Loss of soft tissue
This illness has the potential to cause severe soft tissue loss as a result of tissue necrosis caused by the infection. If treatment is delayed, this could result in decreased hand function or possibly the amputation of a finger.
- Tendon necrosis: The flexor tendons may sustain direct harm from the infection, rupturing or losing their ability to function.
- Adhesions: When scar tissue forms inside the tendon sheath, it can limit the tendon’s range of motion and cause stiffness.
- Loss of skin: In extreme situations, the infection may spread to the skin, leading to tissue damage and possible skin loss.
Osteomyelitis
Both conditions are serious, but pyogenic flexor tenosynovitis mainly affects the tendons and surrounding tissue in the hand, whereas osteomyelitis directly affects the bone structure. Pyogenic flexor tenosynovitis is a bacterial infection within the hand’s flexor tendon sheath, which is regarded as a closed-space infection. Osteomyelitis can infect any bone in the body, whereas pyogenic flexor tenosynovitis affects the tendon sheath in the fingers and hand.
Conclusion
A frequent hand infection that can have serious consequences is PFT. The use of intravenous antibiotics or, in more severe cases, surgical irrigation and debridement are necessary for early therapy. But even with quick and careful care, a serious infection may result in permanent function impairment or even amputation of the affected digit.
It can be difficult to diagnose PFT quickly, but to prevent negative effects and maintain hand function, early detection and treatment are crucial. Broad-spectrum intravenous antibiotics, as well as surgical irrigation and debridement when necessary, are essential components of early treatment. However, a serious infection can still result in decreased function or even amputation of the affected digit even with prompt and comprehensive treatment.
FAQs
How is pyogenic flexor tenosynovitis treated?
It can be difficult to diagnose PFT quickly, but to prevent negative effects and maintain hand function, early detection and treatment are crucial. Broad-spectrum intravenous antibiotics, as well as surgical irrigation and debridement when necessary, are essential components of early treatment.
Flexor tenosynovitis: what causes it?
Although bloodstream infections can induce PFT, penetrating finger injuries involving the flexor tendon sheath are typically the culprit. For fingers to remain viable and functional, urgent care techniques are essential, with a focus on surgical washout.
How does pyogenic flexor tenosynovitis manifest itself?
The Ka navel symptoms of FTS include symmetrical swelling of the affected finger, holding the affected finger flexed, pain when passive digit extension is attempted, and tenderness along the flexor tendon sheath.
How can flexor tenosynovitis be managed at home?
Rest: for two to three days, try not to move the tendon.
Ice: apply a tea towel-wrapped ice pack (or a bag of frozen peas) on the tendon for up to 20 minutes every two to three hours.
Support options include using a soft brace, a tube bandage, or an elastic bandage across the affected area.
Is it possible to heal a flexor tendon without surgery?
It is unlikely that a cut tendon will mend without surgery because the cut ends typically split after an injury. When a flexor tendon is cut, your doctor will advise you on when surgery is necessary. A cut tendon can be repaired in a variety of methods, and some cuts require a particular kind of healing.
How long does tenosynovitis treatment last?
Reducing inflammation, maintaining thumb mobility, and avoiding recurrence are the goals of treatment for de Quervain’s tenosynovitis. Your symptoms should go away in four to six weeks if you begin treatment early.
Is surgery necessary to treat flexor tenosynovitis?
To cleanse the tendon sheath, incisions will be made on the front of the hand and finger during surgery if the ailment has progressed past its very early stages. More than one surgery is typically needed in moderate and severe instances.
Which therapy is most effective for tenosynovitis?
Treatment options for tenosynovitis include rest and cessation of the activity that triggered the condition.
Putting on a splint or brace to lessen tendon stress.
To lessen pain or inflammation, apply heat or ice to the affected area.
Steroid injections or oral steroids to reduce inflammation.
Can tendinitis be completely recovered from?
Following rest and therapy, the majority of patients with tendinitis have quite good prognoses. Depending on the extent of your injury, recovering from tendinitis could take a few weeks to several months. Hold off on starting your usual physical activity until your doctor gives you the “all clear.”
Reference
- Sarpatwari, R. (2018, July 2). Getting a hand on pyogenic flexor tenosynovitis — BROWN EMERGENCY MEDICINE BLOG. BROWN EMERGENCY MEDICINE BLOG. https://brownemblog.com/blogposts/2018/6/20/pyogenic-flexor-tenosynovitis
- Yoon, R., MD. (n.d.). Pyogenic flexor tenosynovitis – hand – orthobullets. https://www.orthobullets.com/hand/6105/pyogenic-flexor-tenosynovitis
- Chan, E., Robertson, B. F., & Johnson, S. M. (2019). Kanavel signs of flexor sheath infection: a cautionary tale. British Journal of General Practice, 69(683), 315–316. https://doi.org/10.3399/bjgp19x704081
- Crowe, C. S., MD. (n.d.). Tenosynovitis: Practice essentials, pathophysiology, etiology. https://emedicine.medscape.com/article/2189339-overview