Sural Nerve
Introduction
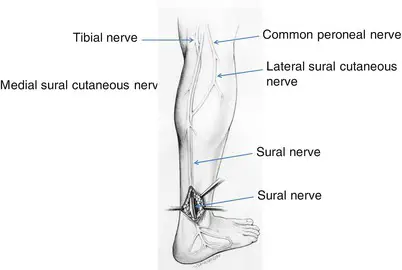
The sural nerve is a sensory nerve in the lower leg, originating from the tibial and common fibular (peroneal) nerves. It runs along the posterior aspect of the calf and provides sensation to the lateral side of the foot and ankle.
The sural nerve is often used as a donor nerve for grafting procedures due to its accessible location and sensory role.
Structure
The medial sural cutaneous nerve and the lateral sural cutaneous nerve, two smaller sensory nerves, combine to produce the sural nerve. The common peroneal nerve has a terminal branch called the lateral sural cutaneous nerve, while the tibial nerve has a terminal branch called the medial sural cutaneous nerve.
Aside from the small saphenous vein, the nerve passes posterolaterally between the two gastrocnemius heads after union in the distal third of the posterior leg, becoming superficial about the mid-calf. Before continuing deep to the fibularis tendon sheath and arriving at the lateral tuberosity of the fifth toe, it passes 2.5 cm posteriorly via the lateral malleolus to the Achilles tendon. The tiny saphenous vein and sural nerve pass posteriorly between the calcaneus and lateral malleolus at ankle level.
Function
The lower lateral leg, lateral heel, ankle, and dorsal lateral foot are all sensed by the sole sensory sural nerve.
Your sural nerve gives the following people skin sensations:
- beneath your knee, towards the rear of your leg.
- your foot’s outside.
- outside heel.
- Ankle.
Muscle Supply
The sural nerve merely innervates the skin’s sensory receptors; it does not innervate any muscle groups. Nonetheless, it passes subcutaneously between the gastrocnemius’s two heads.
Course
The medial sural cutaneous nerve and the lateral sural cutaneous nerve, two smaller nerves, combine to form the sural nerve (S1, S2)in the posterior leg. The tibial nerve (L4-S3) gives rise to the medial sural cutaneous nerve, which descends between the two gastrocnemius muscle heads in the posterior leg compartment. A branch of the common fibular (peroneal) nerve (L4-S2), the lateral sural cutaneous nerve crosses the lateral head of the gastrocnemius muscle. These nerves combine to create the sural nerve when it reaches the distal part of the leg. It is crucial to remember that the union’s level can vary widely, ranging from the popliteal fossa to the ankle’s level where the sural nerve enters the foot.
The sural nerve lowers between the gastrocnemius muscle heads when it rises. After there, it runs parallel to the little saphenous vein till it reaches the ankle, passing close to the calcaneal tendon’s lateral edge. The sural nerve then enters the foot through the space between the calcaneus and the lateral malleolus. The nerve ends as the lateral dorsal cutaneous nerve when it reaches the lateral portion of the foot.
Branches
The skin over the posterolateral side of the distal part of the leg is directly innervated by the sural nerve.
The sural nerve produces two terminal branches when it enters the foot:
The skin across the lateral part of the heel is innervated by the sural nerve’s lateral calcaneal branch. The lateral dorsal cutaneous nerve supplies blood to the lateral side of the foot’s dorsum. For the sensory supply of the lateral side of the fifth toe, this nerve terminates as a dorsal digital nerve.
Anatomical Variantions
The lateral sural cutaneous nerve and the lateral sural cutaneous nerve fuse in different ways and locations, the fibular and tibial branches contribute (since it can form from only one of these), and variations in each lower extremity within a single person are the sources of the sural nerve’s variability.
Embryology
The neural tube and neural crest cells are produced by the neural plate, which develops in the third week following fertilization. The sural nerve is one of the peripheral nerves that develop from neural crest cells. Schwann cells, which improve electrical signal conduction, are also derived from myelinate neurons and neural crest cells in the peripheral nervous system.
Examination
The clinical examination may demonstrate discomfort with palpation posterior and lateral to the Achilles myotendinous junction (at the region of the fibrous arcade) in the event of neural irritation.
Good dependability has also been demonstrated via monofilament testing.
Clinical Importance
Sural Nerve Entrapment
The most common cause of sural nerve entrapment is fascial thickening at the superficial sural aponeurosis, which is where the nerve becomes superficial to the gastrocnemius. In the region that the nerve innervates, a patient with sural nerve entrapment will have sensory abnormalities. In the area of the postero-lateral distal leg and lateral foot to the fifth digit, there may be searing pain, hyperaesthesia, dysaesthesia, or paraesthesia.
Upon examination, the entrapment site could also be sensitive. It must be separated from sciatica coming from sacral roots, exertional compartment syndrome, piriformis syndrome, and popliteal artery entrapment since all would appear similarly. By surgically removing the fascia that is compressing the nerve, decompression can be accomplished.
Sural Nerve Biopsy
A biopsy of the sural nerve may be used to determine the histological etiology of peripheral neuropathy in individuals with no apparent underlying cause. Because of the development of less intrusive technologies like genetic and electrophysiological testing, it is not frequently utilized in modern medicine.
In situations like vasculitic neuropathy, amyloid neuropathy, and multifocal leprosy, a biopsy may still be helpful if these more recent techniques yield no clear solution or a confusing image. Because it is superficial, easily located physically, solely sensory, and persistent anesthesia to its distribution is unlikely to cause long-term patient injury, the sural nerve is an excellent choice for biopsy.
Allodynia, infection, and inflammation of the surgical incision are potential side effects. The extent of sensory loss and recovery from the sensory deficit is closely correlated with the quantity of nerve removed. By 18 months, however, 91% of patients who had a nerve section had recovered from their sensory loss, according to research by Bevilacqua et al.
Sural Nerve Graft
By replacing or bridging a portion of an injured or resected nerve, nerve grafts provide a kind of “track” for the damaged nerve axons to follow as they grow to the desired location. Because it is sensory-only, simple to harvest and capable of producing a respectable amount of graft tissue, the sural nerve is a great option.
Research by Butler et al. revealed that patients had a minor functional impairment and low postoperative discomfort following endoscopic excision of the nerve, even though sensory deficits were fairly substantial following grafting. The results of the study provide credence to the sural nerve’s ongoing usage as a frequent nerve transplant source.
Surgical Importance
A sural nerve block may be used by the surgeon in addition to general anesthesia for foot and ankle procedures. Although ultrasound guidance is a possibility, it is rather simple to do since the nerve is located using anatomical landmarks and is quite superficial at the ankle. As with any nerve block, there are risks, such as injection discomfort, hemorrhage, infection, and adverse response to the anesthetic.
Procedures involving the ankle, calcaneal tendon, or small saphenous vein may cause damage to the sural nerve. Because of its closeness to the sural nerve, the saphenous vein is frequently harvested during coronary artery bypass surgeries, making it vulnerable to damage during the harvesting process.
The anatomical variety of the nerve has been the subject of several investigations by researchers, some of which may have implications for the clinical and surgical results of treatments performed near the nerve. The nerve is frequently utilized for nerve grafting or nerve biopsy since it is not a motor nerve and only provides sensation to a limited portion of the leg and foot. As a result, damage is generally tolerated.
FAQs
Where does the sural nerve come from?
The sural nerve originates within the sciatic nerve, coming from terminal branches of the tibial and common fibular nerves.
How to diagnose a sural nerve?
Your podiatrist will perform a physical exam and a nerve conduction test to ensure an accurate diagnosis. The information gathered will include your foot’s range of motion, your ability to move your toes, and the strength and function of your sural nerve.
What is the problem with the sural nerve?
Indications Your Sural Nerve May Be Having Issues
Common signs of a sural nerve injury include a lack of sensation or numbness, tingling or burning, and sharp or throbbing pain.
What exercises are good for spinal nerve pain?
Nerve gliding, foot and ankle exercises, and aerobic exercise may help relieve severe nerve pain.
Which medicine is best for foot drop?
Amitriptyline, nortriptyline, duloxextine, pregabalin, and gabapentin are substitute therapies. Transdermal capsaicin or diclofenac used locally might also lessen symptoms. Narcotic drugs should be used sparingly, even in cases of severe pain.
References
- Sural nerve. (2022, December 5). Kenhub. https://www.kenhub.com/en/library/anatomy/sural-nerve
- Professional, C. C. M. (2024h, December 19). Sural nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22323-sural-nerve
- Sural nerve. (2023 July 24).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK551640/