Finger Dislocation
Introduction
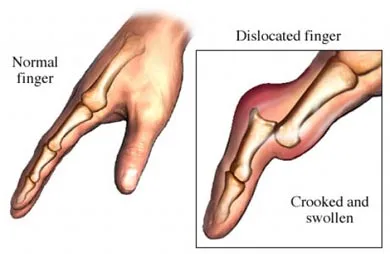
A finger dislocation occurs when the bones of a finger are forced out of their normal position, often due to a sudden impact, fall, or sports injury. It typically causes pain, swelling, deformity, and difficulty moving the finger. Prompt medical attention is crucial to realign the joint and prevent complications.
A common hand injury is finger dislocation, which can happen in the dorsal, volar, or lateral planes as well as at the proximal interphalangeal (PIP), distal interphalangeal (DIP), or metacarpophalangeal (MCP) joints. The fingers are most susceptible to dislocation from high-impact activities and forceful overstretching because they have several articulated joints that link several tiny bones.
Sports, particularly full-contact sports like football, basketball, and rugby, are where these forces are most frequently encountered. However, the joints may get weaker due to repeated, gradual tension from daily activities, which increases the risk of dislocation.
The most common cause of a dislocated finger is excessive force applied to the joint beyond the tensile strength of the connective tissue. The joint’s bony surfaces slip far apart as a result of the tissue (often ligaments) rupturing partially or completely. This movement can impinge on the residual connective tissue, tendons, nerves, and blood vessels, resulting in severe pain. In addition to the injury sustained during the dislocation, the displaced bone may also injure the surrounding tissues, depending on how severe the dislocation was.
The proximal interphalangeal joint (PIPJ) of the finger’s middle joint is the most frequently displaced. One or more of the fingers’ tiny bones may “pop out” of their natural position when the stresses involved are excessive and more than what the supporting muscles and connective tissue can bear. This is referred to as a “dislocated finger” and can occur in one or more IP or MCP joints. The direction of dislocation will determine the forces used at the time of the injury. There is a chance of long-term instability when certain dislocations are linked to a fracture or injury to the ligament supporting the joint’s front and sides.
What is it?
A finger dislocation is a type of joint injury where the finger bones shift sideways or apart, causing the ends to no longer line up appropriately. When a finger is bent backward past its natural range of motion, it typically dislocates.
The medical words “phalanges” and “metacarpal bones” refer to the bones that comprise the finger joints. In an injury, any of these joints could dislocate:
- Distal interphalangeal joints are located closest to the fingernails in the finger joints. Trauma is the primary cause of most dislocations in these joints, and the site of the dislocation frequently has an open wound.
- Proximal interphalangeal joints are the fingers’ middle joints. Coach’s finger or jammed finger are other names for a dislocation in one of these joints. Sportsmen who play ball-handling sports like football, basketball, and water polo are particularly susceptible to this hand injury, which is the most common among all sportsmen. When an athlete tries to block a shot or catch a ball, their fingers are typically bent backward, which causes the dislocation. An athlete’s fingers being bent or twisted by an opponent can also result in proximal interphalangeal joint dislocations, particularly when two athletes struggle or grab for control of a ball.
- Metacarpophalangeal joints are found where the fingers join the rest of the hand, in the knuckles. These joints attach the first row of phalanges in the finger to the metacarpal bones in the palm. Compared to the other two categories, metacarpophalangeal joint dislocations are less frequent because of how solid these joints are. When metacarpophalangeal dislocations do happen, they typically affect the little finger (pinky) or index finger.
Relevant Anatomy
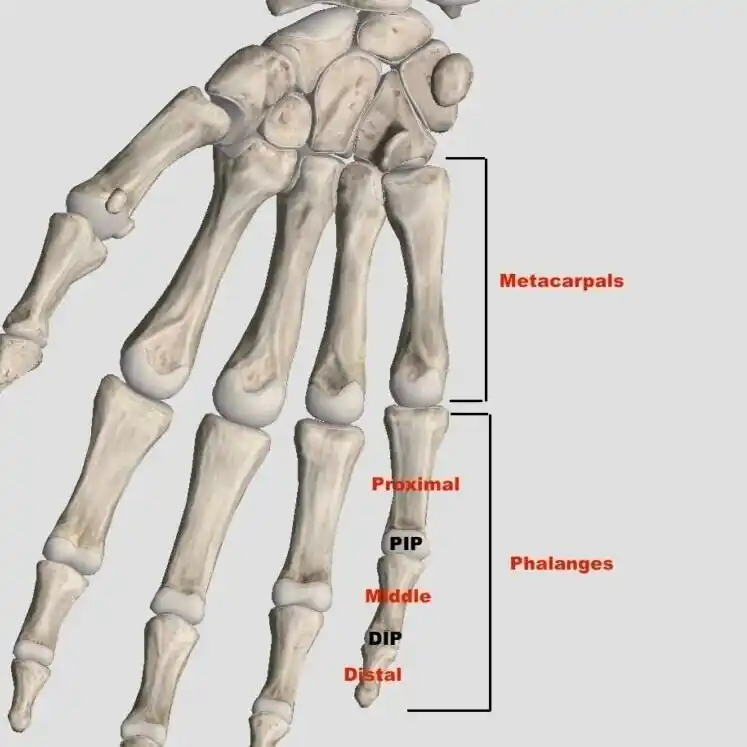
The three joints that make up the finger are the distal interphalangeal (DIP), proximal interphalangeal (PIP), and metacarpophalangeal (MCP) joints. The proximal phalanges and metacarpals are separated by the MCP joint. The PIP and DIP joints are hinge joints that connect the middle and proximal phalanges, respectively, and the middle and distal phalanges. Flexibility and extension are made possible by these PIP and DIP joints, which aid in grabbing, pinching, and clawing or reaching actions. The flexion of the fingertip during gripping is explained by the 105° ± 5° middle phalanx range of motion accessible at the PIP joint. Although the metacarpophalangeal joint can also flex and extend the digit, the MCP joint is responsible for flexion, extension, adduction, abduction, and circumduction.
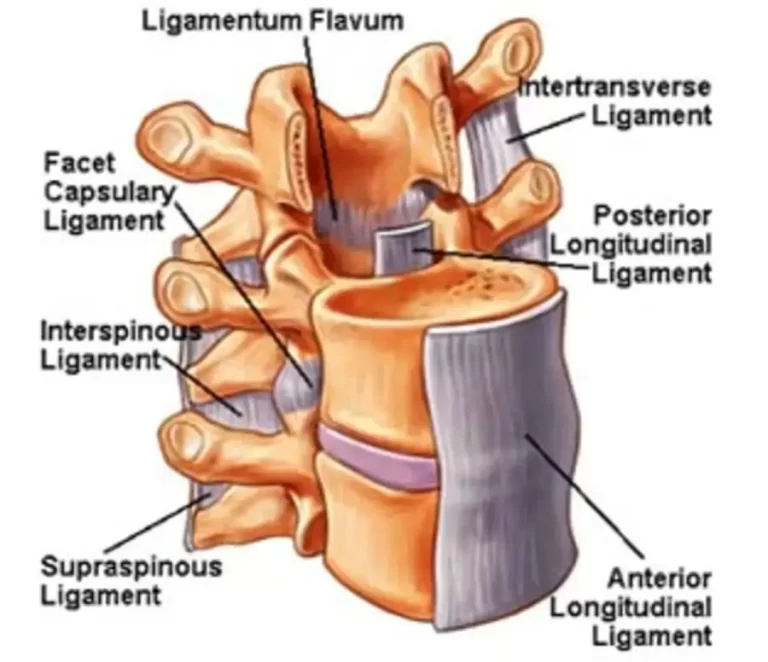
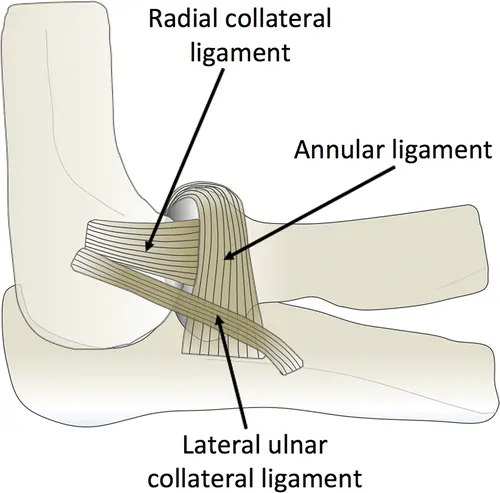
Supporting the phalangeal joints while they move are stabilizers. Both dynamic and static joint stabilizers are available. The ulnar and radial collateral ligaments, volar plates, dorsal capsules, sagittal bands, non-contractile tissue, and collateral ligaments are all examples of static stabilizers. Because it maintains stability and supports the volar side of the joint capsule, the volar plate is a crucial stabilizer that helps keep the finger joints from being overextended. The IP joints are stabilized by the collateral ligaments against radial and ulnar deviation. To prevent bowstringing, sagittal bands encircle the metacarpophalangeal joint, keeping the extensor tendon centered. Among the extrinsic and intrinsic muscles and tendons are dynamic stabilizers.
Lateral bands and central slips are two important dynamic stabilizers. The lateral bands offer a DIP joint extension, whereas the central slip tendon, which is positioned dorsally, produces a PIP joint extension. Last but not least, the volar aspect contains digital arteries and nerves that show up on the radial and ulnar sides of the fingers.
Types Of Dislocation
Depending on which finger joint is involved, there are three different kinds of finger dislocation. They are as follows:
- The joints nearest to the fingertip experience dislocation of the distal interphalangeal (DIP) joint.
- “Jammed finger” is another name for proximal interphalangeal joint dislocation, which is the most common sports injury and affects the joints in the middle of the finger.
- Dislocation of the metacarpophalangeal (MCP) joint takes place at the base of the finger.
Additionally, finger dislocations can be divided into three categories according to how the bones are displaced:
- Dorsal dislocation: The phalanx near the fingertip is displaced toward the back of the hand.
- A volar dislocation occurs when the phalanx at the fingertip shifts in the direction of the palm.
- Lateral dislocation is the sideways displacement of the phalanx closest to the fingertip.
DIP Joint Dislocation
A fingertip deformity is the typical presentation of DIP joint dislocations. DIP joint dislocations can occur dorsally, laterally, or volarly. The most frequent dislocations of the dorsal DIP joint are caused by fractures and skin injuries. They may have an intervening volar plate that results in a non-reducible dislocation, but they are not usually connected to flexor tendon avulsions.
Both dorsal PIP joint dislocations and volar DIP joint dislocations are linked to extensor tendon injuries. Compared to volar or dorsal dislocations, post-reduction instability is more common in the lateral DIP joint. In emergency rooms, isolated DIP joint dislocation without associated soft tissue or fracture injuries is uncommon and is often treated with closed reduction and splinting.
PIP Joint Dislocation
PIP joint dislocation, sometimes referred to as “coach’s finger,” is a highly common dislocation caused by athletic activity. Pain, decreased range of motion, and deformity are the typical indications of PIP joint dislocation. Dorsal, volar, and lateral dislocations are the three types of PIP joint dislocations. While dorsal dislocations are frequent, volar dislocation is associated with a higher risk of comorbidities and frequently challenging reductions.
Injuries to the volar plate, collateral ligament, and dorsal joint capsule are linked to dorsal PIP joint dislocation, which most frequently happens at the middle finger. A ball striking the tip of the finger frequently causes dorsal dislocation, which is caused by longitudinal compression and hyperextension. Dorsal dislocations are the most common cause of Swan neck deformity, which is caused by volar plate damage. The volar plate can become trapped inside the joint, leading to malalignment and oblique rotation, which can make reductions difficult.
Both rotation of the intermediate phalanx and volar dislocation of the PIP joint are possible outcomes. Although it is uncommon, it can happen in conjunction with damage to the extensor tendon’s central slip. Rupture of the central slip following PIP joint dislocation is frequently linked to pseudo-boutonniere PIP flexion contracture if treatment is not received. (A persistent PIP flexion without a DIP extension is called a pseudo-boutonniere.)
The collateral ligaments may be disrupted, leading to lateral PIP dislocation. The patient exhibits joint instability and an x-ray shows a widening of the joint space. Last but not least, rotary volar dislocations can happen when the proximal phalanx wedges itself between the lateral band and extensor tendon by rotating around one of the collateral ligaments. It has been referred to as the “Chinese finger-trap” in the traditional lateral radiography findings.
Metacarpophalangeal Joint Dislocation
Dislocation may occur at the metacarpophalangeal joint as a result of hyperextension or high-energy axial stresses. Because the volar plate protects against hyperextension and the collateral ligaments prevent radial and ulnar deviation, MCP joint dislocation is rare. The index finger is the most frequently dislocated MCP joint.
When the middle finger experiences ulnar stress during hyperextension, the MCP joint dislocates. Dorsally, the common MCP joints typically dislocate. The IP joint is in flexion and the MCP joint is in extension when an MCP joint dislocation occurs. Volar plate interposition is demonstrated by a nonreducible dislocation with dimpling on the volar surface.
Causes
Thumbs have two joints, while fingers have three. A joint is the location where two bones unite. Short strands of fibrous substance called ligaments support the joint and keep the bones together. When a large force weakens the ligaments and the bone slides out of the joint, a dislocation may result.
Dislocated fingers are frequently caused by sports injuries. A 2015 research found that the fingers are impacted by around half of all hand injuries sustained in sports. Sports having the highest rates of hand injuries include football, wrestling, basketball, lacrosse, and gymnastics.
Other causes of a dislocated finger include the following:
- Overextending the finger
- Slamming or harsh force contact to the fingertip
- Falling on an outstretched arm
Individuals who suffer from illnesses that can weaken their ligaments and joints may be more susceptible to dislocations.
Sports injuries, particularly those involving a ball, like football, basketball, and volleyball, are the primary cause of many dislocated fingers. Other major causes include accidents and falls.
Sports injuries
PIP dislocations accounted for 17% of upper extremity injuries among National Football League (NFL) players, according to one study. This is because a finger can quickly become “jammed” when attempting to block or catch a ball. An outstretched finger is hyperextended backward when struck by a ball with such energy that the bones are forced away from the joint.
Fall
Additionally, extending your hand to break a fall can result in a dislocated finger. Your fingers may be forced out of their joints and beyond their typical range of motion by the force of the fall.
Accident
Bones can also separate from the joint when a finger is crushed, such as when a door is closed on the finger.
Genetics
Some people have weak ligaments from birth. Tissues called ligaments offer structural support and connect bones at joints.
Symptoms
The surface skin of a dislocated finger may be sliced, scraped, or bruised, and it is crooked, uncomfortable, and swollen. A dislocated finger may feel unusually loose, weak, or unstable after being straightened on the field.
Excruciating finger pain frequently strikes patients with a dislocated finger suddenly during the acute episode or causal activity. Because of the displacement of the finger bones, this is frequently linked to a noticeable lump or deformity of the finger. At the moment of injury, there is an “audible pop” or tearing sound.
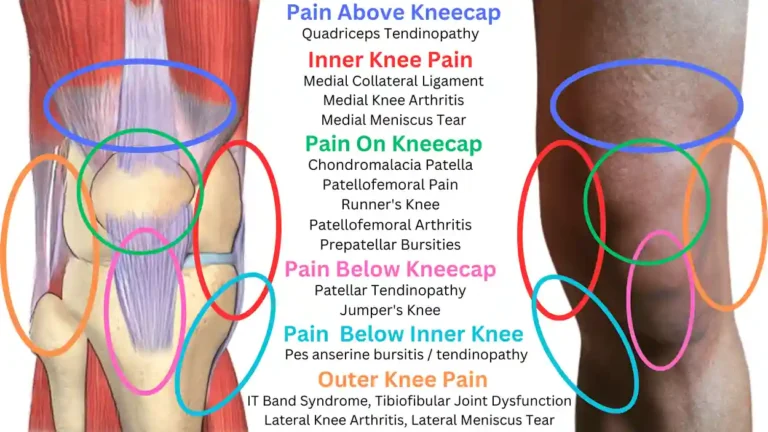
The affected finger joint may be painful in the front, back, or sides. On occasion, pain may also radiate into the hand on the affected side or farther down the finger. After an accident, swelling may start right away or build gradually over a few hours. The patient will be unable to straighten or bend their finger. The dislocation may occasionally be accompanied by a bone break, which calls for immediate medical intervention.
The patient may have some of the following symptoms if the misplaced finger impinges on or damages the nerve:
- Referred pain into adjacent fingers, palms, or even in the arm.
- Particularly distant from the dislocation site, numbness is experienced.
- It is possible to see altered feelings like heat sensitivity or pins and needles.
- The injured finger can appear pale.
The effects of dislocation will cause the patient to continue experiencing pain after the finger joints have been moved. Among these symptoms could be:
- Pain and stiffness may be experienced by the patient, and these symptoms may worsen with certain activities or with rest, especially in the morning.
- Activities that require the use of the hand and fingers, such as opening doors or jars, writing, typing, lifting heavy things, simple gripping, cooking, housework, or transferring weight via the affected hand and fingers, may also make symptoms worse.
- Patients may also feel weak or “unstable” and have soreness around the affected area, which makes it easy for the finger to “pop out” again.
- After an injury, bruises can also form, though they may not show up for a few days.
Diagnosis
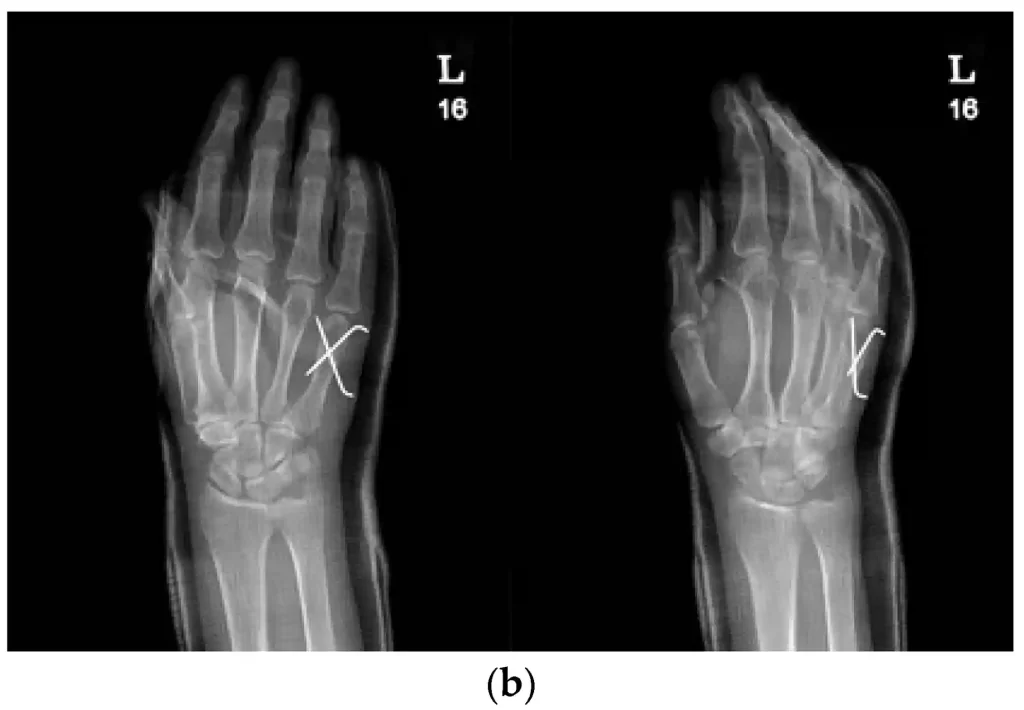
If, following an injury, your finger looks distorted, your doctor will think that it is dislocated. To check for a fracture, your doctor might occasionally prescribe an X-ray of your finger. Avulsion fractures, which occur when a finger bone is wrenched away from attached tendons, are characterized by a bone fragment that separates from the main bone and remains with the tendon. Finger dislocations are frequently accompanied by such fractures.
Physical Examination
A thorough history must be taken by the examiner, taking into account risk factors such as Ehlers-Danlos syndrome, the source of injury, the timing and progression of symptoms, hand dominance, prior finger injuries, occupation, and hobbies. When evaluating finger injuries, a physical examination is essential. Local edema, erythema, pain, deformity, and soreness to the touch are the most typical indications of damage. Joint range of motion, neurovascular health, ligament integrity, and finger alignment should also be evaluated. The proper treatment of displaced joints depends on the stability assessment. A methodical evaluation of the wounded finger helps to prevent bad results, missed diagnoses, and other complications. If a fracture or dislocation is suspected, radiographic assessment using at least three views—oblique, true lateral, and anteroposterior—is necessary.
Examining the hand for bone deformities, ecchymosis, edema, or skin integrity requires adequate lighting. If a laceration or abrasion compromises the integrity of the skin, the examiner should try to assess the patient without using blood. The entire active and passive range of the finger must be examined. In patients with adequate circulation, the examiner may apply finger tourniquets or administer an epinephrine-containing anesthesia.
It is crucial to perform a comprehensive neurovascular assessment on the injured hand. To identify any possible damage to the digital nerve, the injured digit should be examined using the same digit of the unaffected hand for light touch, pinprick, and 2-point discrimination. A capillary refill can be used to assess the digital artery by comparing it to the opposite hand’s unaffected finger. The examiner should additionally check for rotation or angulation if they observe a malformation. The patient is instructed to create a fist, if at all feasible, with each fingertip pointing in the direction of the scaphoid, to test for rotation or angulation. Overlapping or “scissoring” indicates that the injury has a rotational component. The finger joint’s lateral stress is used to examine the collateral ligaments, and hyperextension should be examined to evaluate the volar plate’s competency. The Elson test is used to evaluate the extensor tendon complex’s central band/slip integrity. The location of the greatest tenderness can also be found by palpation.

- X-ray. X-rays use electromagnetic radiation to create images of the body’s internal structures. Doctors use X-ray images to confirm dislocations and to check for fractures or breaks.
- MRI scan. Strong magnetic fields and radio waves are used in an MRI scan to provide finely detailed images of the body’s inside tissues. If a physician suspects substantial tissue damage close to the displaced joint, they might suggest an MRI scan.
Differential Diagnosis
- Fracture-dislocation for example a distal phalanx fracture (tuft fracture)
- Collateral ligament injuries- commonly referred to as “finger sprains”
- Tendon avulsion, such as mallet fingers, avulsion fractures of the flexor digitorum profundus, etc.
Treatment
It is possible to treat a dislocated finger without administering local anesthetic. If the displaced bone is stuck against the side of the joint, the doctor will use pressure to release it to rectify the dislocation. To return the bone to its proper place, the physician can draw outward when the end of the bone is released. We refer to this as closed reduction. Depending on the type of dislocation, you will need to tape the finger to another finger or wear a splint for three to six weeks after your finger joint returns to its usual position.
Your dislocated finger might require surgical surgery if your doctor is unable to straighten it with closed reduction or if the damaged joint remains unstable following closed reduction. Finger dislocations exacerbated by major fractures or joint-related fractures are also treated surgically.
Do not pop the finger back into the joint right after a dislocation. You might cause irreversible harm to underlying structures, such as:
- Blood vessels
- Tendons
- Nerves
- Ligaments
- Instead, keep your wounded finger motionless by applying ice. Use an ice pack or wrap ice in a towel to ice. Avoid putting ice on your skin directly. If surgery is required, avoid eating or drinking anything.
Medical treatment
Before surgical or conservative methods can be used to treat MCP, PIP, and DIP joint dislocations, depending on the volar plate or other supporting structures’ involvement, post-reduction stability, and ease of reduction. An instantaneous anesthetic can be achieved before any reduction by administering a digital nerve block at the dorsal base of the damaged dislocated finger using lidocaine, bupivacaine, or tetracaine. The majority of the dislocations are straightforward and quickly repositioned.
Metacarpophalangeal (MCP) Joint Dislocation
Depending on how severe the injury is, both surgical and non-operative options may be used to treat it.
Non-Operative Management
This includes splinting and a closed reduction. To glide the proximal phalanx into place, the doctor provides axial compression and relocating pressure over the phalangeal base while performing closed reduction by extension. The traction technique utilized in PIP joint dislocation is not the same as this method. Avoid making more than one attempt at reduction since failure to decrease could be a sign of volar plate interposition and could result in the volar plate being displaced between flexor tendons, lumbricals, or articular surfaces. For three to six weeks, the injured finger should be splinted with the wrist extended to 30° and the MCP joint slightly flexed between 30° and 60° to avoid terminal extension. Two more weeks of buddy taping should then be used.
You should seek medical attention immediately. A qualified medical practitioner may do the following:
Reduction
- Treating a dislocated finger or thumb usually starts with carefully repositioning the bone in the joint. We call this process reduction.
- The Doctor may apply a local anesthecia to the patient’s hand to numb the affected area before executing a reduction.
- To verify that the bone inside the joint is aligned, the medical practitioner may arrange an X-ray test once the reduction operation is finished.
Immobilization

- To protect and immobilize the wounded finger while it heals, a splint is typically required after reduction. A stiff metal strip called a splint is used to stabilize a fractured or dislocated bone. A person who is immobilized is unable to move their finger, preventing them from dislocating or hurting it again.
- Additionally, a medical expert can advise “buddy taping” the splinted finger to a nearby finger. Buddy taping allows for a greater range of motion while supporting the damaged finger.
- For a few weeks, a person with a dislocated finger might have to wear the splint. On the other hand, prolonged usage of a splint might result in persistent stiffness and decreased finger movement.
Operative Management
This is recommended for non-reducible MCP joint dislocations since volar plate involvement is likely to occur in these situations. Both dorsal and volar approaches can be used to openly reduce MCP joint dislocation, but the dorsal technique is better since it reduces the danger of neurovascular damage. To avoid terminal extension, the wrist is splinted in a 30° extension position with a minor flexion of the MCP joint for two weeks following surgery. Avoiding immobilization of the PIP and DIP joints is advised. It usually takes 4–6 weeks to return to a pre-injury range of motion.
- Proximal Interphalangeal Joint Dislocation
In contrast to MCP joint dislocations, PIP joint dislocations can also be managed with both surgical and nonoperative methods. However, practitioners must identify if the dislocation is dorsal, volar, lateral, or rotational because the therapy may vary.
Closed Dorsal PIP Reduction To move the misplaced finger, one hand can apply pressure to the dorsal surface of the proximal phalanx while the other hand performs a small extension and longitudinal traction. Following reduction, the examiner needs to get an x-ray and check for joint instability in all planes. On lateral radiographs, the dorsal PIP joint typically has a “C” shape. This contour may indicate persistent dorsal subluxation, which causes extreme stiffness if it assumes a “V” form following reduction. Dorsal splinting at 30° flexion is used to treat PIP joint dislocation, which is largely stable following reduction.
Despite being the least frequent, volar PIP joint dislocations are typically successfully reduced. The PIP and MCP joints are subjected to mild traction and modest flexion to achieve the decrease. The wounded digit is splinted for six weeks following the reduction.
Operative intervention is frequently necessary for lateral dislocations. For closed reduction, the middle phalanx must be gently rotated back into place once the extensor tendon and lateral bands have been relaxed by wrist extension and MCP flexion, respectively. The joint is not extremely unstable if reduction allows for a full range of motion without subluxation; in these situations, splinting and reevaluation in two or three weeks are advised. An orthopedic referral is necessary for evaluation and potential open repair of all unstable dislocations. Joint instability, severe ligament, soft tissue, tendon damage, or non-reducible dislocations are among the conditions that call for surgery.
The cornerstone of emergency care after reduction is still splinting. There was no difference in strength, pain, or function at three weeks between aluminum orthoses and buddy taping when treating Eaton grades I and II hyperextension-type injuries. Buddy tape did, however, demonstrate reduced edema and increased range of motion.
- Distal Interphalangeal Joint Dislocation
Compared to PIP joint dislocation, DIP joint dislocation therapy is simpler. Longitudinal traction reduces dorsal DIP joint dislocation, which shifts dorsal pressure on the distal phalanx when the DIP joint flexes. After a simple open reduction in the emergency room, DIP is splinted for two to three weeks in flexion of 10 to 20 degrees. After concentric reduction, 4-6 weeks of K-wire fixation are frequently used to address chronic DIP joint instability, such as those more frequently observed in lateral dislocation. Surgery is required for irreversible dislocation, which is typically caused by volar plate interposition.
- K-wire fixation
Some patients who have a dislocated finger may also have a bone fracture, depending on the kind or extent of the accident. A fracture happens when a bone is struck with enough force that it splinters or splits into two or more pieces.
Splinting and reduction are also necessary for finger fractures. K-wire fixation may be necessary for certain individuals who have fractured fingers. Surgeons can assist in stabilizing bone fragments by implanting K-wires, which are thin metal rods.
Physical therapy
Most patients recover well after moving if they receive the right PT care. Patient compliance has a significant impact on the intervention’s effectiveness rate. To allow the damaged connective tissue to recover and develop “scar tissues,” treatment typically entails an initial phase of immobilization in a buddy splint for a few weeks. Ice therapy can be used to minimize pain and swelling during the first phase, and elevating the injured hand can assist reduce swelling even further. Gentle workouts to preserve strength and mobility may be allowed throughout this immobilization time.
The physiotherapist can start the injured finger’s rehabilitation after the splint is taken off. To preserve muscular strength and flexibility and hasten the healing process, this will first entail mild mobilizations.
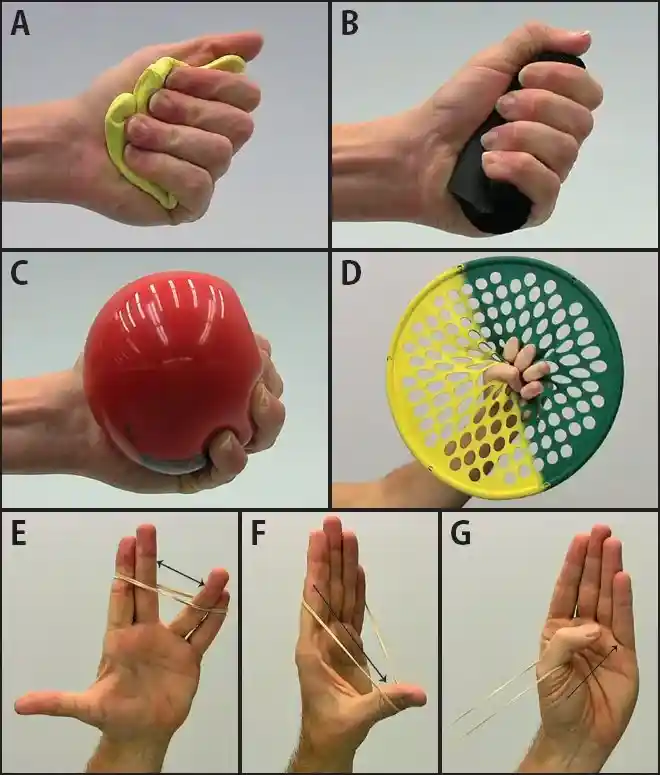
A physiotherapy session could include:
- To lessen pain and swelling, use elevation and ice therapy.
- Finger bracing or splinting.
- To lessen joint pain and stiffness, soft tissue release and mild joint mobilization are used.
- Active-assisted range-of-motion exercises for healing fingers: Using the other hands, gently help the injured finger flex and extend within a pain-free range.
- Suggestions for adjusting daily activities to avoid re-injury.
After the splint is taken off Increase your hand and wrist strength by moving on to moderately intense workouts. The following exercises are part of this:
- Finger lift: Lift each finger separately and hold it for a few seconds while keeping your palm flat on a table and your fingers straight.
- Fist making: Make a fist. Assist with an uninjured hand and try to help it bend into the fist and hold it for 5-10 seconds.
- Object pick-up: Use the damaged finger and thumb to pick up small items such as buttons, marbles, pins, or coins.
- Passive stretching to lengthen tight muscles.
- Exercises for dexterity to increase mobility and functional strength.
- Strengthening of the hand’s intrinsic and lumbrical muscles.
- Eccentric training with a resistance band for the wrist and hand to improve stability.
To achieve the best possible result, patients must then engage in pain-free mobility and strengthening exercises as part of their rehabilitation. To increase the stability of the affected joint, special attention must be paid to strengthening the hand and finger muscles.
A gradual return to activity or sports participation is advised in the latter phases of therapy, under the supervision of a physiotherapist, as long as symptoms do not worsen. This frequently involves applying protective tape, especially when ball sports or contact sports are resumed.
Factors that affect recovery time can include:
- The severity and location of the dislocation
- Damage to ligaments and tendons
- Bone fractures
- Requiring surgery
Some patients may additionally need physical or occupational therapy after reduction and splinting. Exercises that strengthen the finger and increase the range of motion will be demonstrated by a physical or occupational therapist.
After your injury, you can typically resume your regular activities, including sports, in a few weeks. But it can take up to six months for your finger to fully recover. In many situations, pain and stiffness may be chronic or even irreversible, particularly if the dislocation is followed by a severe break or if medical attention is delayed.
As symptoms subside and you receive protection (buddy tape, splint), you may be able to resume your regular activities, including sports, in a few weeks. Until radiographs indicate that the wounded finger is healing, keep an eye out for any indications of malrotation or loss of reduction. However, it could take up to six months for the body to fully recover. Pain and stiffness may be chronic or even permanent in certain circumstances, especially if the dislocation is followed by a fracture or if medical attention is delayed.
For example
Initial Exercises
- When you first start these, have your friend strap on. Work through the following exercises in order; the range of motion will be limited, but the goal is to comfortably bend and straighten the fingers. Don’t push this. At first, mobility will be limited by pain, swelling, and bruises.
Stage 1 exercises
- The goal is to make a fist, but don’t push yourself too hard and only do what your pain and swelling will allow. To help you restore complete movement, do the exercises slowly and consistently each day. Movement will first be restricted by pain and swelling; this is typical at this point. Go through the following order. These workouts can be performed while wearing straps.
- Repeat five times a day, touching each finger to your thumb.
Stage 2 exercises
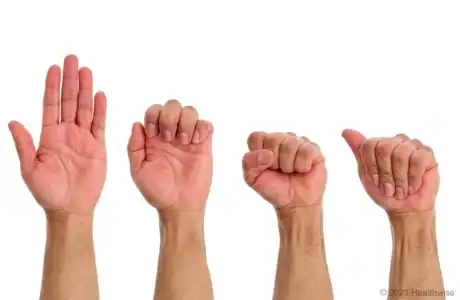
- At two weeks, the goal is to maintain fully bending your finger while also straightening it as much as pain permits. Bend and straighten the joints in all of your fingers using your other hand to support the joint to be manipulated and keep your finger steady. Should your finger joints become rigid when bent, use your other hand to hold them straighter. For ten seconds, maintain the position. Five times over
From 4-6 weeks
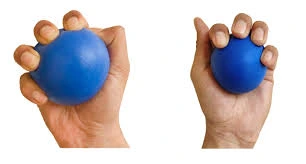
- Squeezing a light sponge, a pair of socks, soft putty, or Play-Doh are examples of extremely minor resistance exercises that you can add to your fingers when pain permits. Heavy lifting, grasping, and contact sports should be avoided for at least six weeks while the finger heals.
Return to Work or Driving
- When you feel capable of doing the physical duties necessary for your employment, you can resume work. When you are comfortable driving, have good grip strength, can safely stop in an emergency, and are not experiencing severe hand pain, you can resume driving. If you have straps, tape, or a splint on your hand, it is not recommended that you drive. If you have any questions about your fitness to drive, please contact your insurance provider or the DVLA website.
Home care
You should
- Until you are instructed to take it off, keep the strapping or splint in place.
- To lessen swelling, raise your hand and apply ice.
- With the strapping and splint in place, move your finger as comfortably as possible.
- When necessary, take simple over-the-counter pain relievers.
- Take off any jewelry or rings from the affected hand.
You should not
- Unless otherwise advised, participate in any contact or physical sports for a minimum of six weeks.
- If a specialist appointment has been requested, do not miss it.
While their finger recovers, folks can perform the following at home:
- Keeping their splint clean and dry.
- To lessen swelling, they should keep their finger up above their heart.
- Letting their finger rest and not moving it while it heals.
- Using ice packs or cold compresses to lessen pain and inflammation.
- Using over-the-counter drugs to aid with pain and swelling, like acetaminophen or ibuprofen.
- Completing any finger exercises prescribed by a therapist regularly.
A dislocated finger may be more susceptible to other injuries after recuperation. One can lessen the possibility of relocating the finger by:
- Strengthening ligaments, tendons, and muscles using hand and finger workouts.
- Using buddy tape or a splint when participating in sports.
- Avoid wearing rings while playing sports.
Complications
- Following DIP dislocation therapy, chronic stiffness is frequently observed.
- Overtreatment, such as prolonged splinting and multiple attempts at reduction of volar PIP joint dislocations, increases the chances of volar plate scarring and flexion contractures.
- Chronic pain.
- Delays or missed volar plate injuries are frequently linked to:
- boutonniere deformity
- swan neck deformity, laxity
- contractures.
- Swan neck deformity, PIP flexion contracture, and mallet finger deformity can also occur if the dislocations of the finger are chronically undiagnosed.
Prevention
For most people, a dislocated finger recovers without any lasting effects. However, it’s crucial to take preventative measures because the fingers can be susceptible to dislocation in the future.
- When participating in sports, always use the appropriate gear and splint your fingers to prevent further injuries.
- To increase mobility, do the hand exercises regularly.
- To reduce the chance of falls, remove any tripping hazards from your floors.
- Try to keep your fingertips away from items like football helmets, basketball nets, and sports shirts.
- Put on safety gloves.
- Before taking part in gaming events, take off any jewelry, including rings.
Following treatment for a dislocated finger, the use of a protective splint, taping, and ongoing hand and finger muscle training can help prevent re-injury.
By applying a protective splint or strapping your dislocated finger to another finger, you can frequently avoid further injury after treatment. Surgery may be advised if dislocations happen frequently.
Prognosis
- Although it can take four to six months for your finger pain to go away, the long-term outlook is typically advantageous. A minor degree of persistent swelling may also occasionally be present around the injured joint, particularly if it is the proximal interphalangeal joint. A dislocated finger frequently sustains another injury in athletics.
- The majority of people heal from a dislocated finger without any long-term consequences. However, it’s crucial to take preventative measures because your finger can be more susceptible to dislocation in the future.
- Although it may take up to four to six months for the finger pain to go away, the long-term prognosis is typically advantageous. In certain instances, there may be a potential for re-injury, and there may also be a slight amount of persistent swelling surrounding the wounded joint, particularly if it is the proximal interphalangeal joint.
- Recovery to preinjury ranges takes around 4 to 6 weeks, and MCP joint dislocations have a high probability of necessitating surgical intervention.
- Except for lateral PIP joint dislocations, which typically call for surgical intervention, PIP joint dislocations are stable with reduction or relocation.
- Similar to PIP joint dislocation, lateral DIP joint dislocation is more likely to require surgical intervention, and isolated DIP joint dislocation is uncommon.
Is there an urgent medical situation?
If you think you may have a dislocated finger, you should get medical help. A finger that has been dislocated may also be sprained or broken. It might be challenging to distinguish between a sprain and a break without medical assistance because they have symptoms that are similar to those of a dislocation.
- Joint stiffness and long-term loss of mobility might result from postponing treatment or attempting to identify and treat the finger on your own.
Summary
A dislocated finger might be painful and upsetting, but it is not a life-threatening situation. But it’s crucial to get medical help right away.
One should not try to move the dislocated finger on their own. Attempting to manipulate the wounded finger may result in further harm to the surrounding structures or the joint. Dislocated fingers typically take a few weeks to mend after medical intervention. Recovery time might be greatly prolonged by bone fractures and associated tissue injury.
FAQs
How can a dislocated finger be fixed?
Most finger dislocations are treated by doctors injecting an anesthetic into the base of the affected finger, which causes the finger bones to return to their original position (a process known as reduction). Physicians are unable to manually straighten the finger. Even after physical straightening, the joint is still unstable. People have big fractures as well.
Are dislocated fingers self-healing?
You will be given an appointment to return to the fracture clinic for follow-up if necessary; these injuries typically heal on their own with time. Get in touch with the fracture clinic right away if the affected joint keeps dislocating.
Finger subluxation: what is it?
Hand therapy: Interphalangeal joint between the thumb and fingers…
When the two gliding surfaces of these joints separate abnormally, it is called a dislocation. A subluxation occurs when the joint surfaces are only partially separated.
How can a fractured finger be straightened?
Using a well-designed splint or orthosis to administer a mild, continuous corrective force over an extended period is one of the best methods to restore extension to a bent finger. The creation of orthoses intended to straighten a bent finger is a specialty of our therapists.
What is the at-home treatment for dislocated fingers?
If you can, ice the finger for 20 minutes every few hours for a few days. When you can, keep raising your finger. Observe your physician’s advice when taking painkillers. Surgery or follow-up care with a hand orthopedist may be required, depending on the type of injury.
Can a finger that has been dislocated be bent?
If your finger is dislocated, you most likely won’t be able to bend or straighten it. A “jamming” force applied to the end of a finger can cause dislocation of the finger or from hyperextending the digit beyond its natural range, though they are most commonly associated with sports-related incidents.
How can one determine whether a finger is sprained?
The injured joint will become painful, stiff, and swollen following a sprain. The degree of injury is typically reflected in the amount of swelling. The PIP joint is the most often sprained. The volar plate (palmar plate) is the most often injured ligament.
Is massaging an injured finger beneficial?
Early Immobilization: Use the proper splint to immobilize the injured joint for approximately two weeks. Gradual Movement: To avoid being overly rigid, begin with little motions after the initial phase. Concentrate on gently stretching and stroking the finger’s sides.
Will my crooked finger straighten out?
After three to four months, you should be back to your usual self. As soon as you are injured, call your doctor. People may be reluctant to be checked out because they believe the injury is not significant. You may need to wear a splint for a longer amount of time as a result of this delaying the healing process.
Reference
- Harvard Health. (2023, December 7). Finger dislocation. https://www.health.harvard.edu/a_to_z/finger-dislocation-a-to-z#:~:text=Prognosis,dislocated%20often%20is%20injured%20again.
- Christiano, D. (2018, September 18). Identifying and treating a dislocated finger. Healthline. https://www.healthline.com/health/dislocated-finger#outlook
- Finger dislocations. (n.d.). Cambridge University Hospitals. https://www.cuh.nhs.uk/patient-information/finger-dislocations/#:~:text=What%20is%20a%20finger%20dislocation,with%20the%20splint%20/%20strapping%20intact.
- Finger (Phalanx) dislocation – Gateshead Health. (2024, December 2). Gateshead Health. https://www.gatesheadhealth.nhs.uk/resources/finger-phalanx-dislocation/#:~:text=What%20can%20I%20expect%20after,moving%20the%20finger%20and%20gripping
- Eske, J. (2019, March 13). How to treat a dislocated finger. https://www.medicalnewstoday.com/articles/324683