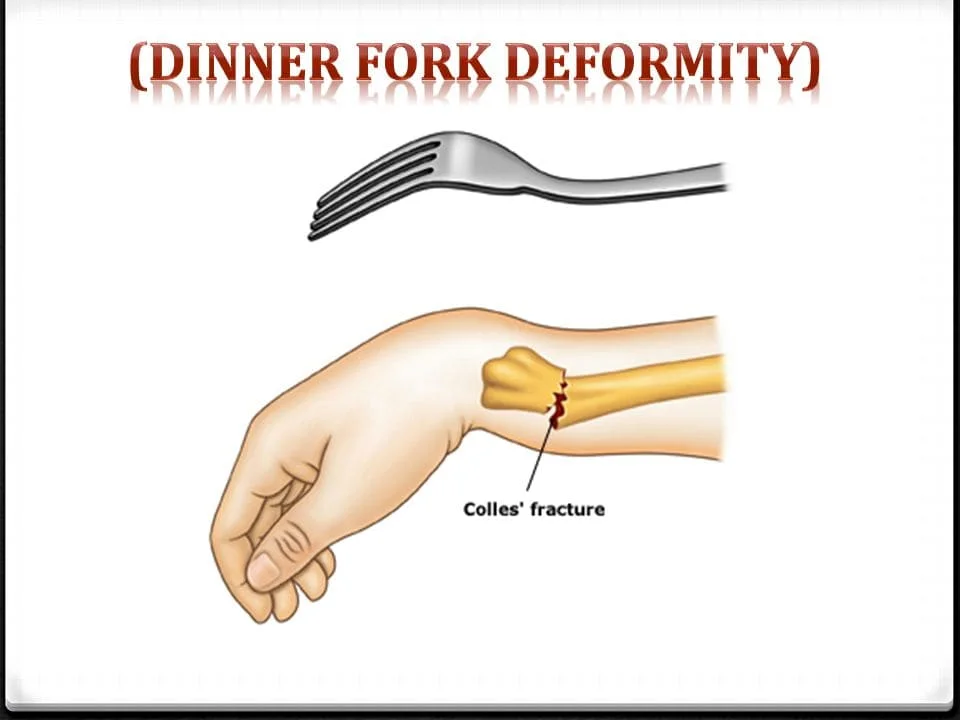
Dinner Fork Deformity
What is Dinner Fork Deformity?
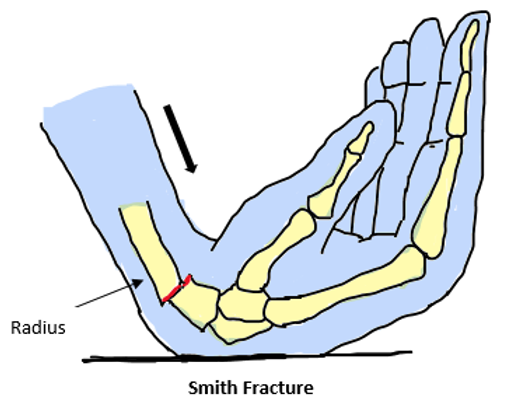
The term “Dinner Fork Deformity” refers to a characteristic deformity seen in certain wrist and hand injuries, particularly associated with Colle’s fracture, where the distal radius in the forearm is fractured with dorsal and radial displacement of the wrist and hand. This deformity resembles the shape of a dinner fork, hence the name.
Colle’s fracture, which results in a distal radius fracture in the forearm with dorsal (posterior) and radial displacing of the wrist and hand, is the cause of the dinner fork deformity
The
Deformity known as the “bayonet” or dinner fork is caused by the way the forearm is shaped.
Causes of Dinner Fork Deformity
Causes of this deformity include Colle’s fracture, traumatic injury, overextended hand (common in children), osteoporosis, and sports-related injuries among others. While not the primary cause, calcium deficiency can contribute to its development.
- fractured wrist Mostly Colle’s Fracture
- Overextended Hand (frequent in children)
- Osteoporosis Patients
- Traumatic Injury
- Sportsmen, skiers, skaters, and bikers
Although not the primary cause of the deformity, a calcium deficiency is one of its contributing factors.
Symptoms of Dinner Fork Deformity
Symptoms of the Dinner Fork Deformity include wrist pain, difficulty moving the wrist, swelling, tenderness, numbness, bruising, and difficulty holding objects.
- The patient experiences pain when flexing his wrist.
- The patient finds it difficult to move his wrist.
- The area around the wrist is swollen.
- There is tenderness to the touch.
- Severe impact frequently results in bruises.
- The affected hand is numb.
- Pale fingers are possible.
- The patient has trouble holding anything.
Diagnosis
Diagnosis involves assessing factors such as radial shortening, loss of ulnar inclination, wrist radial angulation, dorsal displacement of the distal end, and dorsal tilt.
- Radial shortening
- loss of ulnar inclination
- wrist radial angulation
- dorsal displacement of the distal end, and dorsal tilt
Treatment
Treatment options include therapy for the upper limb, medication, elevation, compression, and surgical intervention depending on the severity of the fracture.
Physiotherapy plays a crucial role in the recovery process, involving techniques like active and passive wrist mobilization exercises to improve the range of motion and reduce pain and discomfort.
- Therapy for the upper limb Medication, Elevation, and Compression. ⇒ Surgical intervention – Management is based on how severe the fracture is.
- A cast by itself can be used to treat an undisplaced fracture.
- A moderately displaced and angulated fracture may require closed reduction.
- For severe angulation and deformity, an open reduction and internal or external fixation can be required.
Physiotherapy Treatment in Dinner Fork Deformity
After fracturing in a cast –
Look for any loss or excessive tightness in the plaster cast.
Make sure the sling has the appropriate neck padding by checking it.
Elevation and massage from the fingertip to the palm should be used to treat dependent oedema.
To avoid stiffness, actively range of motion exercise the thumb, shoulder joint, elbow, and unaffected side digit.
Supination and pronation are the only movements prohibited on the affected side; all other movements are encouraged.
⇒ In second week –
If the cast is excessively loose or broken recasting is advised.
Exert your ROM muscles in your thumb, elbow, shoulder, and digit.
If external fixation is used, in addition to the previously mentioned conditions, look for any infections and aggressive pronation and supination.
After the second week –
Wrist Mobilization –
A combination of hydrotherapy and thermotherapy was used to lessen pain, oedema, and discomfort.
Wrist mobilization is started actively. The patient is made to remain mid-prone over a table while seated in a chair. The patient is taught to vigorously flex and extend the wrist with
gravity abolished while the other hand holds the affected forearm in place.
Passive wrist mobilization:
This starts 7–10 days following the previous course of treatment. With the injured hand lying on the table’s edge, the patient sits. The injured arm is periodically elevated above the table (dorsiflexion) and lowered below it (palmer flexion) while being fixed with the usual hand.
Alternately, pronation and supination can be accomplished with the Indian salutation method of namaskar (for dorsiflexion) and reverse salutation (for palmer flexion).
exercises include actions such as opening doors, turning on lights, and collecting beans to place them into a box.
Exercises involving ulnar deviation are recommended to enhance writing proficiency and grip.


One Comment