Motor Neuron Disease (MND)
What is a Motor Neuron Disease (MND)?
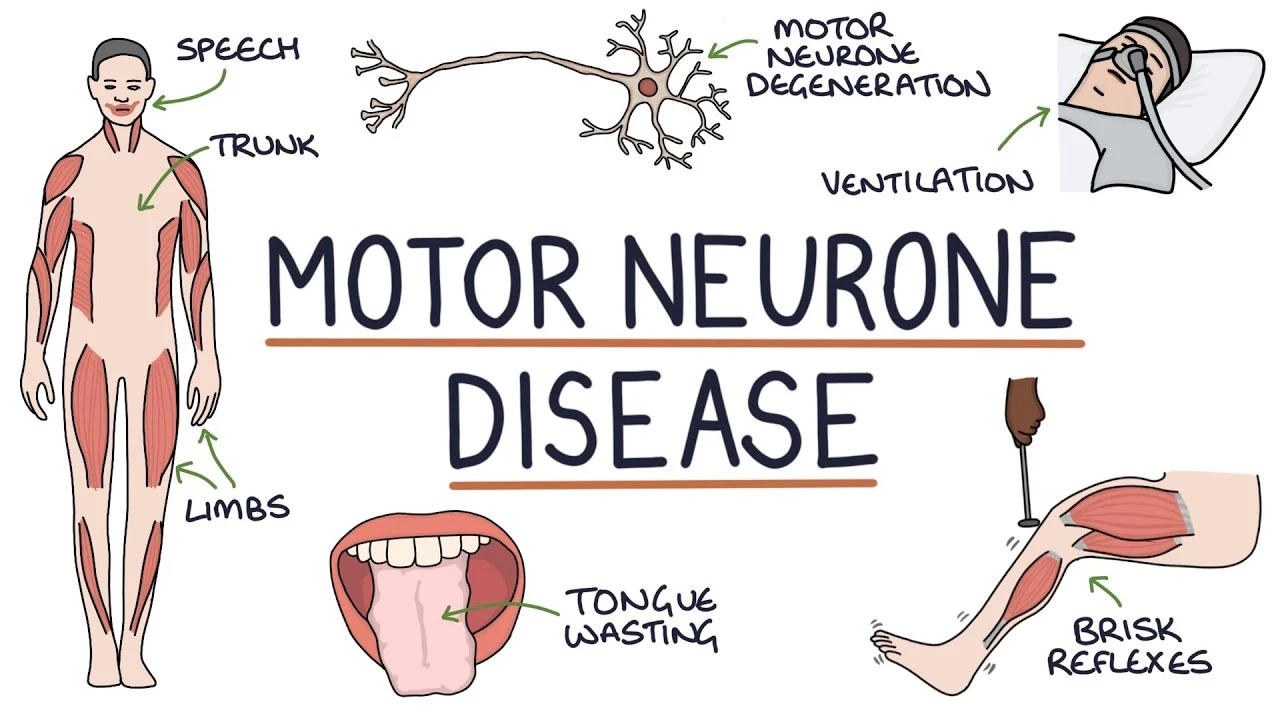
Motor Neuron Disease (MND), also called Amyotrophic Lateral Sclerosis (ALS) is a progressive neurodegenerative disorder affecting the nerve cells in the brain and spinal cord that control voluntary muscle movement.
It is characterized by the gradual degeneration and eventual death of motor neurons, leading to muscle weakness, atrophy, and eventual paralysis. MND typically progresses rapidly, with individuals experiencing a decline in mobility and function over time.
While the exact cause of MND remains unknown in most cases, genetic factors, environmental influences, and abnormal protein metabolism are believed to play a role in its development.
MND is the short form of motor neuron disease, which affects the nerves known as motor neurons. These nerves are located in the brain and spinal cord and help signal your muscles what to do.
Adults of any age can be affected by motor neuron disease, an uncommon condition that mainly affects those in their 60s and 70s. Motor neurons, which are cells in the brain and nerves, are the source of this disease. These cells eventually quit functioning over time.
There is no cure for MND, however, there are therapies that can assist in alleviating its effects on a person’s everyday life. Some people have had the ailment for many years. MND can severely reduce life expectancy and, tragically, cause death.
What is Motor Neuron Disease?
- Motor neuron disease (MND) is an uncommon disorder that gradually destroys different parts of the nervous system. This causes muscular weakness, typically with visible wasting.
- In terms of MNDs, amyotrophic lateral sclerosis (ALS) is the most common type. MND occurs when motor neurons, which are specialized nerve cells in the brain and spinal cord, stop functioning correctly and die prematurely. This is referred to as neurodegeneration.
- Motor neurons control muscular function, including grasping, walking, speaking, eating, and breathing.
As MND advances, any or all of these tasks may become increasingly difficult to do.
Physiology of Motor Neuron Disease
They are a sort of nerve cell that transmits information throughout your body, allowing you to move freely. There are two primary types:
- Upper motor neurons are located in your brain. They transmit signals from there to your spinal cord.
- The lower motor neurons are situated in your spinal cord. They send signals from your brain to your muscles.
When you have motor neuron disease, nerve cells die, so electrical messages cannot travel from your brain to your muscles. Your muscles gradually deteriorate. You may hear a doctor or nurse refer to this as “atrophy.”
When this happens, you lose control of your motions. It becomes more difficult to move, speak, swallow, and breathe. Each form of motor neuron disease affects various types of nerve cells and has a unique etiology. ALS is the most prevalent of these disorders in adults.
Types of Motor Neuron Disease
Here’s an overview of the types of several motor neuron illnesses.
Amyotrophic Lateral Sclerosis(ALS)
- Both upper and lower motor neurons are impacted by ALS. With ALS, you gradually lose control of the muscles that allow you to move, speak, chew, swallow, and breathe. They weaken and deteriorate with time. Your muscles may also be stiff or twitching.
- Most of the time, ALS is referred to be “sporadic.” This indicates that anyone can have it. Only 5% to 10% of instances in the United States involve families.
- Amyotrophic Lateral Sclerosis generally begins between the ages of 40 and 60. Most persons with the condition live for three to five years after their symptoms appear, although others might live for ten years or more. Primary Lateral Sclerosis (PLS) is comparable to ALS but exclusively impacts higher motor neurons.
- It produces weakness and stiffness in the arms and legs, as well as a decreased walking pace and impaired balance. Speech becomes sluggish and slurred.
- It often begins in persons between the ages of 40 and 60, similar to ALS. With time, the muscles weaken and become stiffer. But it doesn’t result in death, unlike ALS.
Progressive Bulbar Palsy(PBP)
- This is a type of ALS. Many patients with this syndrome will eventually acquire ALS.PBP harms motor neurons in the brain stem, which is located at the base of the brain.
- The stem contains motor neurons that allow you to chew, swallow, and talk. With PBP, you may slur your speech and have difficulty eating and swallowing. It also makes it difficult to regulate emotions. You may unintentionally laugh or cry out.
- This condition is analogous to progressive bulbar palsy. It affects the motor neurons that govern speech, chewing, and swallowing. Pseudobulbar palsy produces uncontrollable laughter or crying.
Progressive Muscular Atrophy
- This kind is much less common than ALS or PBP. It may be hereditary or episodic. Progressive muscular atrophy mostly affects lower motor neurons. Weakness commonly begins in the hands and progresses to other regions of the body. Your muscles become weaker and may cramp. This illness can progress to ALS.
Spinal Muscular Atrophy
This is a hereditary disease that affects the lower motor neurons. Spinal muscular atrophy is caused by a deficiency in a gene called SMN1. This gene produces a protein that protects motor neurons. They perish without it. This weakens the upper legs, arms, and trunk.
SMA is classified into multiple categories based on when symptoms initially show.
- Type 1. (also known as Werdnig-Hoffmann illness). It normally begins when the child is six months old. Children of this type are unable to sit on their own or hold their heads. They have low muscular tone, slow reflexes, and difficulty eating and breathing.
- Type 2. It begins between six and twelve months. Children of this kind can sit, but they cannot stand or walk independently. They may also have difficulty breathing.
- Type 3. (also known as Kugelberg-Welander illness). It starts between the ages of two and seventeen. It hinders a child’s ability to walk, run, stand erect, and climb stairs. Children with this condition may also have a bent spine, short muscles, or tendons surrounding their joints.
- Type 4. It generally begins after age 30. People with this kind may have muscular weakness, tremors, twitching, or difficulty breathing. It primarily affects muscles in the upper arms and legs.
Kennedy’s Disease
- It is also hereditary and only affects men. Females can be carriers without becoming sick. A mother carrying the Kennedy’s disease gene has a 50 percent probability of passing it on to her kid.
- Males with Kennedy’s illness have trembling hands, muscular cramps and twitches, and weakness in their face, arms, and legs. They may have difficulty swallowing and speaking. Men may have larger breasts and a low sperm count.
What are some Basic Facts Concerning MND?
- Motor neuron disease (MND) causes signals from motor neurons to stop reaching the muscles eventually. This causes the muscles to weaken, stiffen, and waste, affecting your ability to move, talk, eat, drink, and breathe.
- Some people have cognitive and behavioral problems, although the illness affects everyone differently. Not all symptoms impact everyone or occur in the same sequence. Symptoms grow at variable rates, making the disease’s course difficult to predict.
- MND reduces life expectancy and has no treatment. Although the condition will advance, symptoms can be treated to help patients attain the highest possible quality of life.
Causes of Motor Neuron Disease
MND develops when specialized nerve cells (motor neurons) in the brain and spinal cord gradually fail. It’s unclear why this occurs
Genetic Causes
- MND is caused by a genetic mistake, which accounts for 20% of cases. Half of all genetic cases will occur in persons with a family history of MND. The remaining half of genetic instances will develop in people who do not have a family history.
- A family history of frontotemporal dementia may also enhance the likelihood of inheriting MND.
The gene mistake impairs the cell’s capacity to function normally and persist. - If you have a hereditary type of MND, your kid may be at risk of having it as well. A variety of factors, including age, can influence their likelihood of getting the illness. Not everyone with the genetic mutation develops MND in their lifetime.
- Typically, the longer you live, the higher your chances of developing the illness. If you have a parent with MND and no other family history of the disease, you have a 1.4% higher chance of developing MND. The risk of MND in the general population is around 0.3%.
Other Possible Causes of Motor Neurone Disease
It’s unknown why motor neurons start to lose function. The majority of specialists feel it is a mix of variables affecting either the motor neurons or the cells that support them. Some ideas include various cell processes, including:
RNA Processing and Aggregates
- Protein clumps that are abnormal and form inside motor neurons are called aggregates. They may impair the motor neurons’ regular function and are present in almost all cases of motor neuron disease (MND). It also indicates that the cell is experiencing stress.
- The most frequently occurring protein in these aggregates is TDP-43. This protein helps the cell process its genetic instructions through RNA, a molecule. Genetic motor neuron disease (MND) cases may be caused by mutations in the gene (TARDBP) carrying this protein.
Interruption of Cell Transport
- Transport systems are found in every cell and are responsible for bringing chemicals and nutrients into the cell and removing waste. Studies indicate that disruptions occur to the motor neuron transport networks. Toxic waste can naturally accumulate in cells over time as a result of aging and regular cell activity.
- The body uses waste disposal processes that are impacted by environmental factors and aging to get rid of harmful waste.
Glial Cells
- Motor neurons are surrounded, supported, and nourished by glial cells. The motor neurons no longer receive the nourishment and support necessary for normal operation when they aren’t functioning properly.
- Research is still ongoing regarding their relevance in MND.
Glutamate
- Neurotransmitters are specialized “messenger chemicals” that nerve cells employ to communicate with one another. The neurotransmitter glutamate is one of them. It stimulates neurons, and an excessive amount of activity through this is thought to harm the neurons.
- Riluzole, a medication used to treat motor neuron disease (MND), works by preventing glutamate from acting on neurons.
The Mitochondria
- A cell’s mitochondria are its “batteries.” They give a cell the energy it requires to perform its regular tasks. People with motor neuron disease (MND) may have malfunctioning mitochondria.
Symptoms of Motor Neuron Disease
Motor neuron disease (MND) affects people differently. Not everyone experiences all of the symptoms in the same order. The rate at which symptoms develop might also vary. Take aid from your health and social care specialists when you notice a change.
MND cannot be cured or reversed, however, therapy, technology, and medications can help with symptoms. All of the following symptoms could be present in you:
- Muscular weakness, a decrease of muscular mass (wasting), and movement and mobility issues.
- Muscle cramps and spasms, cause vibrating sensations, known as fasciculation;
- Stiff joints that limit the range of action; and pain or discomfort produced by other symptoms (MND does not often cause pain).
- Speech and communication issues can influence how you talk, gesture, and express yourself.
- Swallowing issues might alter how you eat and drink.
- Saliva difficulties occur when thin saliva collects in the mouth or becomes thick and sticky.
- Weak coughing makes it difficult to clean the throat.
- Breathing difficulties can cause shortness of breath and weariness.
- Emotional lability refers to improper emotional reactions, such as laughing when unhappy.
- Changes in thinking and conduct affect around half of persons diagnosed with MND, and this figure rises in the later stages.
Risk Factors of Motor Neuron Disease
The following are some of the recognized risk factors for MND:
- Age: MND is most typically diagnosed in adults aged 50 to 70.
Genetics: Approximately 10% of MND cases are hereditary, which means they occur in families. There have been various genes linked to an increased risk of MND.
Military service: Veterans, particularly those who fought during the Persian Gulf War, are more likely to acquire MND. This might be caused by exposure to certain substances or environmental conditions. - Occupation: People who labor in specific jobs, such as farming, construction, and electrical work, may be more susceptible to MND. This might be caused by exposure to poisons or chemicals.
- Some studies have found that a history of head trauma may raise the risk of MND.
- Other medical conditions: People with autoimmune illnesses, for example, may be at a higher risk of developing MND.
Diagnosis
A neurologist would often diagnose MND based on the patient’s symptoms and the results of a physical examination. For MND, there isn’t a single test. To rule out other potential reasons for your symptoms, several tests may be performed.
- Blood tests are one type of test that may be performed. They can be used to examine the function of organs or to find a sign of muscle injury called creatinine kinase.
- Magnetic Resonance Imaging (MRI) scan, which provides a thorough image of your spinal cord and brain.
- Electromyography (EMG): Electromyography (EMG) measures the electrical activity in your muscles measured by electromyography (EMG), which provides information on how well your motor neurons communicate with your muscles.
- Nerve conduction test: this test is similar to an EMG but measures the speed at which your nerves can conduct an electrical signal.
- Lumbar puncture: this test tests spinal fluid to rule out conditions involving inflammation or nerve damage brought on by an infection.
- Muscle biopsy: in very rare cases, this test examines a small sample of muscle to see if the issue is with the muscles.
In certain cases, the diagnosis can be supported by gene tests. They could explain how they came to have the illness. More details about experts who can assist with genetic testing can be obtained from your general practitioner.
Differential Diagnosis
Early diagnosis of motor neuron disease (MND) might be challenging. This is because a lot of the initial symptoms may be brought on by other, more prevalent medical diseases, such as a trapped nerve, which can occasionally result from wear and tear on the bones of the spine and trap nerves beneath it.
- Peripheral neuropathy is the term for damage to a portion of the nerve system caused by another illness, such as type 2 diabetes.
- Swallowing issues brought on by gullet inflammation or constriction.
- Speaking difficulties brought on by voice box issues.
- Injury to the brain in younger individuals caused by a stroke or other neurological diseases like multiple sclerosis (MS)
Complications of Motor Neuron Disease
The most frequent complications of MND include:
- Respiratory failure: is the most prevalent cause of mortality in patients with MND. The muscles that govern breathing weaken, making it more difficult to breathe. Eventually, patients with MND may need to utilize a ventilator to breathe.
- Difficulty swallowing: can result in malnutrition and dehydration. People with MND may need to use a feeding tube to acquire the nourishment they require.
- Speech problems: As the muscles that regulate speech weaken, speaking becomes more difficult. People with MND may require assistive technology, such as a voice synthesizer, to communicate.
- Pain: MND patients frequently experience pain, which can be caused by muscular weakness, spasms, and bone and joint disorders.
- Exhaustion: People with MND frequently suffer exhaustion, which can make it difficult to do everyday tasks.
- Emotional issues: MND is a tough condition to deal with, and patients may experience anxiety, depression, and other emotional issues.
Additional complications that may develop in patients with MND include:
- Nutritional deficits can occur when patients with MND have difficulties swallowing or ingesting enough food.
- Pneumonia: This is a dangerous pulmonary infection that is more likely in persons with MND due to their difficulties removing mucus from the lungs.
- Pressure sores are sores that form on the skin as a result of laying or sitting in the same posture for an extended period.
- Contractures are shortened muscles that make movement difficult.
Living with Motor Neuron Disease
- The outlook varies depending on the kind of motor neuron disease.
- Some are milder and move more slowly than others. Although there is no cure for motor neuron disorders, medications, and therapy can help alleviate symptoms and improve quality of life.
Treatment of Motor Neuron Disease
A person with motor neuron disease (MND) would typically need support from a variety of professionals, including general practitioners.
- Highly specialized clinics where patients receive occupational therapy and assistance with daily duties from a specialist nurse.
- Exercises and physiotherapy to keep you strong and less stiff.
- Guidance from a speech-language pathologist.
- Dietitian’s recommendations for food and diet.
- A medication known as riluzole can somewhat halt the illness’s course.
- Medications to treat issues with saliva and to ease the tightness of the muscles.
- Mental assistance for both you and your carer.
MND has no known treatment. But there are plenty of things you may do to:
- lessen your symptoms with the assistance of experts.
- keep up your standard of living.
- Maintain your mobility for as long as feasible.
Medication
- Riluzole: The first medication for ALS to be licensed by the Food and Drug Administration (FDA) in the United States is riluzole; nevertheless, it is unable to repair motor neuron damage that has already occurred.
- The antioxidant edaravone, which has FDA approval for the treatment of ALS, decreases the deterioration of physical function and stops the disease from getting worse in ALS patients.
- Nusinersen is the first FDA-approved medication for treating SMA in children and adults. It belongs to a class of treatment known as anti-sense oligonucleotide therapy and functions by raising the level of SMN protein, which is required for the normal function of the muscles and neurons.
- Gene therapy with Onasemnogeme abeparovec-xioi (ZolgensmaTM): The FDA approved Onasemnogeme abeparovec-xioi gene therapy for infantile-onset SMA in children under the age of two. The targeted motor neurons receive a fully functional human SMN gene from a safe virus, which enhances both survival and muscle activity.
- Benzodiazepines, baclofen, and tizanidine are examples of muscle relaxants that can help with muscle spasms and relieve stiffness.
- Injections of botulinum toxin have the potential to alleviate stiffness in muscles by attenuating hyperactive muscles. To halt drooling, they could be injected into the salivary glands. Medication for excessive salivation includes atropine, glycopyrrolate, and amitriptyline.
Supporting Treatments
- Rehabilitation and physical therapy can help with atrophy and weakness of the muscles, avoid joint immobility, and improve posture. Exercises for strengthening and improving the range of motion and circulation will help lessen stiffness. For issues with speech, chewing, and swallowing, some people need further therapy.
- Heat application may help with muscle soreness. Some persons may find it easier to preserve their independence with the use of assistive devices such as wheelchairs, orthotics, speech synthesizers, supports, or braces.
- A balanced diet and adequate nutrition are necessary to maintain weight and strength. People who are incapable of chewing or swallowing may require a feeding tube.
- To help with movement and function, you could need the assistance of equipment and home changes. A wheelchair, communication devices, tube feeding, and a ventilator are a few examples of these.
- Sleep apnea during the night can be avoided with non-invasive positive pressure ventilation (NIPPV), commonly referred to as ventilators.
- Some people may also have weakened their neck, throat, and chest muscles, which makes them need assisted breathing during the day.
Depending on the kind of MND and the age at which symptoms first appear, different people have different prognoses. Most MND patients pass away two to three years after their illness first manifests. On the other hand, some people have extended lifespans.
MNDs, including PLS and Kennedy’s disease, typically don’t have a fatal outcome and develop slowly. Long stretches of stability are possible in SMA type III patients. Certain types of MND, like ALS and the severe form of SMA, are fatal.
Physical Therapy of Motor Neuron Disease
For those with motor neuron disease (MND), physical therapy can provide several advantages, such as:
- Enhanced muscle function and strength.
- expanded range of motion.
- less weariness and pain.
- enhanced respiration.
- improved standard of living.
Here are some of the objectives of physical therapy for MNDs:
- Maintain and increase muscular strength and function: This can assist MND patients remain active and independent for as long as feasible.
- Prevent contractures: Contractures are muscular shortenings that make joint movement difficult. Physical therapists can assist avoid contractures by stretching and using other treatments.
- Pain and spasticity are frequent signs of motor neuron disease. Physical therapists can employ a range of approaches to assist patients manage their symptoms.
- Improve breathing: As MNDs worsen, they may impact the muscles that govern respiration. Physical therapists can educate persons with MNDs on improving their breathing and staying independent for longer.
- Maintain proper posture and alignment: This might help you avoid discomfort and other issues.
- Promote general well-being: Physical therapy can also assist persons with MNDs to stay active and involved in their lives.
Here are some of the particular therapies that physical therapists can utilize for patients with MNDs:
- Exercise: This might involve strengthening, stretching, and aerobic activities. The type and amount of exercise will differ according to the individual’s demands and ability.
- Manual Therapy: Massage, joint mobilization, and other approaches for pain relief and movement can all be considered manual therapy.
- Assistive Devices: Physical therapists can support persons with MNDs in selecting and using assistive equipment such as canes, walkers, and wheelchairs to maintain mobility and independence.
- Education: Physical therapists may educate patients with MNDs about their disease and how to manage their symptoms. They can also educate carers on how to support their loved ones with MNDs.
It is crucial to emphasize that physical therapy is not a cure for MNDs, although it can help manage symptoms and improve quality of life. If you have MND, discuss with your doctor if physical therapy is suitable for you.
How does it develop with time?
- Motor neuron disease worsens steadily over time.
- As breathing, eating, and moving become increasingly difficult, interventions like face mask breathing or feeding tubes may be needed.
- The disease eventually leads to death, however, the time it takes to reach this point varies greatly.
A few people can live with motor neuron disease for years even decades. - You would prefer not to know how long you’ll live. If you want to learn more, speak with your GP or your care team.
Prevention of Motor Neuron Disease
Unfortunately, there is no known technique for preventing motor neuron disorders (MNDs), such as Amyotrophic Lateral Sclerosis. The specific origins of MNDs are still unknown, although research indicates that a mix of genetic and environmental factors may be involved. However, certain lifestyle choices can improve general health and well-being, which is always beneficial. This includes:
- Maintaining a nutritious diet: A well-balanced diet high in fruits, vegetables, and whole grains can offer your body the resources it requires to function effectively.
- Regular exercise can assist in enhancing your general fitness and well-being. However, it is critical to select activities that are appropriate for your specific skills and prevent overexertion.
- Maintaining a healthy weight: Being overweight or obese increases your chances of acquiring a variety of health issues, including MNDs.
- Quitting smoking: Smoking is a significant risk factor for a variety of health issues, including cancer, heart disease, and stroke. It is also considered a risk factor for MNDs.
- Limiting alcohol consumption: Excessive alcohol use can harm your liver and other organs and raise your chance of getting MNDs.
- Managing stress: Chronic stress may be detrimental to both your physical and mental health. Finding healthy stress-management techniques, such as yoga or meditation, might be useful.
It is crucial to recognize that these lifestyle practices do not ensure MND prevention. However, they can assist enhance general health and well-being, which is beneficial to everyone.
What’s new regarding the study of motor neuron disorders?
The goal of the National Institute of Neurological Disorders and Stroke (NINDS) is to lessen the burden of neurological disease by conducting basic research on the brain and nervous system. The National Institutes of Health (NIH) component NINDS funds a wide spectrum of research to identify the etiology of motor neuron diseases (MNDs), develop more effective therapies, and eventually prevent and cure the disorders.
Summary
Although there is yet no cure for motor neuron disease (MND), many of its symptoms are manageable. There is no impact on the sensations of taste, smell, touch, hearing, or vision.
Under the care of a multidisciplinary team, people with MND live longer and in better health.
FAQs
What is the primary cause of Motor Neurone Disease?
Overall, MND is thought to be caused by a mix of environmental, behavioral, and genetic factors. Most occurrences of MND occur without a clear etiology. Approximately one in every ten instances is ‘familial’, which means the disorder is inherited. This is caused
What are the typical early indicators of motor neuron disease?
Fasciculation refers to muscle twitching, tingling, or pins & needles.
Numbness in the hands, feet, or legs.
Fatigue or excessive fatigue.
Tripping, and one or both legs get thinner.
Dropping items owing to weak or stiff hands.
Speech may be slurred or feeble.
Swallowing difficulty.
How long do individuals with motor neuron disease live?
Patients with MND grow more handicapped. Life expectancy following diagnosis is between one and five years, with 10% of those with MND living for ten years or more. People with MND have complicated and individual demands.
Where do the most typical symptoms of MND begin?
MND does not often create cognitive issues or impair an individual’s cognition. The major signs of MND include muscular wasting (which is frequently initially observed in the muscles of one hand, arm, or leg). Muscle weakness may make it difficult to open bottles or jars, carry heavy things, or climb stairs.
Where do the most typical symptoms of MND begin?
MND does not often create cognitive issues or impair an individual’s cognition. The major signs of MND include muscular wasting (which is frequently initially observed in the muscles of one hand, arm, or leg). Muscle weakness may make it difficult to open bottles or jars, carry heavy things, or climb stairs.
Can motor neuron illness be cured?
There is no cure for motor neuron disease, although therapy can help alleviate the symptoms that impact your life. You will be treated by a team of experts as well as a general practitioner. Treatments include highly specific clinics, which often involve a trained nurse and occupational therapist to assist with everyday chores.
What is the last stage of MND?
The last stages of MND often feature progressive weakness of the respiratory muscles and increased drowsiness. This is frequently the cause of mortality, either due to infection or muscular failure. Specialist palliative care improves quality of life by managing symptoms.
What age groups are affected by MND?
You are likely to be over 40 years old when diagnosed, and the majority of patients with MND are between the ages of 50 and 70. Men suffer about twice as frequently as women, however this varies. It varies depending on the kind of MND and is consistent in patients over the age of 70.
References
- Healthdirect Australia. (2022, August 29). Motor neuron disease (MND). https://www.healthdirect.gov.au/motor-neurone-disease-mnd
- Motor neuron diseases. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/motor-neuron-diseases
- What are motor neuron diseases? (2016, December 15). WebMD. https://www.webmd.com/brain/what-are-motor-neuron-diseases
- Department of Health & Human Services. (n.d.). Motor neuron disease (MND). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/motor-neurone-disease
- What is MND? (n.d.). MND Association. https://www.mndassociation.org/about-mnd/mnd-explained/what-is-mnd
- Motor Neurone Disease MND. (n.d.). Physiopedia. https://www.physio-pedia.com/Motor_Neurone_Disease_MND