Trigeminal Nerve
Introduction
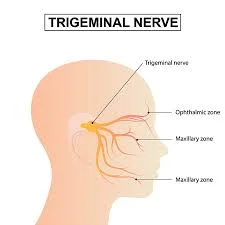
The trigeminal nerve (CN V) is its fifth and largest cranial nerve. Its primary function is to provide sensory innervation to the face, which is divided into three major branches. The ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves are the three branches. The trigeminal ganglia, located within the Meckel’s cave of the middle cranial fossa, connect these branches.
The ophthalmic nerve communicates with the eye, part of the nasal cavity, the face, and the skull above the palpebral fissure. The nasal cavity, sinuses, palate, maxillary teeth, middle region of the face, and skull above and below the brow are all innervated by the maxillary nerve, a sensory branch.
The mandibular nerve is unique in that it includes both sensory and motor fibres. It provides sensory innervation to the buccal mucosa, mandibular teeth, and skin beneath the mouth. The motor parts of V3 innervate all masticatory muscles.
Anatomical Course
Three sensory nuclei—the mesencephalic, primary sensory, and spinal nuclei of the trigeminal nerve—as well as one motor nucleus that runs from the midbrain to the medulla make up the trigeminal nerve. A nucleus (plural nuclei) is a collection of neuronal cell bodies found in the central nervous system.
At the pons level, the sensory nuclei combine to form a sensory root. The motor nucleus continues to develop into a motor root. These roots are similar to the dorsal and ventral roots of the spinal cord.
The trigeminal ganglion develops from the sensory root in the middle cranial fossa. A ganglion (plural ganglia) is an association of nerve cells away from the central nervous system. The trigeminal ganglion is situated lateral to the cavernous sinus, in a depression in the temporal bone. This depression is referred to as the trigeminal cave.
The trigeminal ganglion’s peripheral aspect divides into three areas: ophthalmic (V1), maxillary (V2), and mandibular.
The motor root travels along the floor of the trigeminal cave, below the sensory root. Its fibres are limited to the mandibular division.
The superior orbital fissure and foramen rotundum allow the ophthalmic and maxillary nerves to exit the cranium lateral to the cavernous sinus. The mandibular nerve exits the foramen ovale into the infra-temporal fossa. (Note: whereas we talk about nerves getting out of the cranial cavity, sensory parts can also be said to be nerves entering the cranial cavity considering they are afferent fibres).
Divisions
Ophthalmic Nerve
The ophthalmic nerve divides into three terminal branches: frontal, lacrimal, and nasociliary, which innervate the skin and mucous membrane of frontonasal prominence derivatives.
- forehead and scalp
- Frontal and ethmoid sinuses
- Upper eyelid and conjunctiva
- Cornea
- Dorsum of the nose.
Parasympathetic Supply:
Lacrimal gland: Postganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve) travel along the zygomatic branch of V2 before joining the lacrimal branch of V1. The fibres provide parasympathetic innervation to the lacrimal glands.
The maxillary nerve
The maxillary nerve has 14 terminal branches that innervate the skin, mucous membranes, and sinuses of the maxillary prominence of the first pharyngeal arch.
- Lower eyelid and its conjunctiva
- Cheeks and maxillary sinuses
- The nasal cavity, lateral nose, canine teeth, incisor, upper lip, upper molar, and gingiva are all involved.
- Superior palate.
Parasympathetic Supply:
Lacrimal gland: Postganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve) travel along the zygomatic branch of V2 earlier combining the lacrimal branch of V1. The fibres provide parasympathetic innervation to the lacrimal glands.
Nasal glands: Parasympathetic fibres are also transported to the mucous glands of the nose. Post-ganglionic fibres travel with the nasopalatine and greater palatine nerves (V2 branches).
Mandibular Nerve
The lingual nerve, auriculotemporal nerve, inferior alveolar nerve, and buccal nerve are the four terminal branches of the mandibular nerve that emerge in the infra-temporal fossa.
The skin, mucous membrane, and striated muscle derivatives of the first pharyngeal arch’s mandibular prominence are innervated by these branches.
Sensory Supply:
- The oral cavity’s floor and mucous membranes
- The external ear
- Lower lip Chin Anterior 2/3 of the tongue (general sensation only; special taste sensation provided by the chorda tympani, a branch of the facial nerve)
- Lower molar, incisor, and canine teeth, along with their associated gingiva.
Motor Supply:
- Masticatory muscles include the medial and lateral pterygoid, masseter, and temporalis.
- Anterior belly of the digastric and mylohyoid muscles (both suprahyoid)
- Tensor Veli Palatini
- Tensor tympani.
Parasympathetic Supply:
Submandibular and sublingual glands are innervated by post-ganglionic fibres from the submandibular ganglion (derived from the facial nerve), which travel with the lingual nerve.
Post-ganglionic fibers from the otic ganglion, which originates from the glossopharyngeal nerve (CN IX), innervate the parotid gland. These fibers follow the auriculotemporal branch of the V3.
Trigeminal Nerve Function
The trigeminal nerve is the sensory nerve for the head and face. It senses touch, heat, cold, and pain through structures inside the skull (the brain’s coverings, or meninges), the scalp, face, corneas of the eyes, sinuses, and the insides of the mouth and nose. It also transmits proprioceptive sensations from the temporomandibular joint. This input tells your brain whether your mouth is open or closed without having to look in the mirror.
The mandibular branch of the trigeminal nerve also contains motor nerve fibres. It controls the chewing muscles (masseter, temporal, pterygoid, mylohyoid, and digastric). These muscles allow you to move your lower jaw (mandible) up and down, as well as side to side. The mandibular nerve also regulates muscles in the palate and temples.
Causes of trigeminal nerve
Trauma and injuries can harm the trigeminal nerves. Accidents, tumours, and damage from dental or facial surgery can bruise or cut nerves.
A trigeminal nerve injury can affect a small area, such as a piece of gum, or a large area, such as one side of the face. The injury can interfere with chewing and speaking. The extent of nerve damage is determined by where it occurs.
You may continue to experience numbness or facial pain in the area served by the nerve. These symptoms are indicative of trigeminal neuropathy.
In most cases, an injured trigeminal nerve will regain function over time. Surgery is only used in rare cases to reconnect severed nerves. Some patients require a nerve graft to replace a damaged nerve with a healthy one.
Trigeminal neuralgia
Trigeminal neuralgia is characterised by pain emanating from the trigeminal nerve, which originates near the top of the ear and divides into three branches, leading to the eye, cheek, and jaw. We have two trigeminal nerves, one on each side of our faces, but trigeminal neuralgia pain typically affects only one side.
Trigeminal neuralgia pain differs from other types of facial pain. It is frequently described as stabbing, lancinating, or electrical sensations, and it is severe enough to prevent the affected person from eating or drinking. The pain passes through the face in seconds, but as the condition progresses, it can last minutes or even longer.
Trigeminal neuralgia is also known as tic douloureux, which translates to “painful tic.”
Assessment
The paranasal sinuses of the face, mucous membranes, corneas, and skin of the face and neck are all under the control of the CN V’s three terminal branches. As a result, the trigeminal reflex can be used to assess the nerve’s proper function in each of the areas it serves.
A trigeminal nerve reflex is a natural response to stimuli that indicates the nerve is functioning properly. As it contains both motor and sensory fibres, responses from each structure should be evaluated in clinical examinations and assessments.
It is safe to presume that the CN V tract is operating normally when the reflex, such as the corneal or jaw reflex, is present.
It’s interesting to note that a reduction or increase in the reflex’s strength can help pinpoint the lesion and estimate how big the defect is inside the CN V tract.
Sensory Examinations –
Pain and light touch are the two primary sensory perceptions related to the CN V that are being studied. The preferred method for light touch testing is to use a cotton wisp, with the examiner instructing the patient to close their eyes and say “yes” each time they feel something.
Assuming there are no sensory deficiencies in the area, this test is first conducted on regions not supplied by the CN V to establish an initial starting point. Once the subject has closed their eyes, the examiner lightly touches the area supplied by the nerve with the cotton wisp. The nerve is always tested bilaterally to identify unilateral or bilateral (B/L) lesions.
The same procedure is used to test nociception, but instead of using a cotton wisp, a sharp object is used for the test.
Corneal reflex
The corneal reflex is the B/L involuntary eyelid blinking that occurs when the cornea is stimulated thermally, painfully, or tactilely. Since the facial nerve is an efferent limb and the ophthalmic nerve is an afferent limb, the lack of this reflex suggests damage to either the ophthalmic or TNr/Ophthalmic nerve or facial nerve.
Deficits in ipsilateral reflexes are caused by peripheral damage, while deficits in bilateral reflexes are caused by central damage. Other cornea-related disorders and environmental factors, such as glaucoma and diabetes, can also affect this reflex.
Jaw jerk
The jaw jerk reflex is utilised to determine the health of upper motor neurons that project to the trigeminal motor nucleus. The examiner places a finger between the subject’s lower lip and chin, keeping the mouth slightly open.
After that, the examiner taps the finger downward. Normally, the reflex is minimal or absent. Interestingly, the reflex is amplified in upper motor neuron lesions because the mandible jerks upward due to the masseter muscles.
Lacrimal reflex
The lacrimal reflex is triggered by irritation of the cornea and conjunctiva, resulting in the production of tears. The reflex arc’s CNS components are the superior salivary nucleus and facial nerve (CN VII), while its afferent limb is the ciliary fibres of the nasociliary branch of V1 in the trigeminal nerve. An abnormal reflex arc causes watering of the eyes in the absence of an appropriate stimulus.
Motor Examination
The Motor Examination tests the superficial muscles of mastication, specifically the temporalis and masseter muscles.
Muscle mass: To measure the subject’s mass, an examiner palpates the masseter and temporalis muscles while the subject is instructed to squeeze their teeth.
Placing the fingers of the examining hand beneath the chin and asking the patient to open and resist closing their mouth are two ways to measure muscle strength.
Motor nucleus function – the subject is asked to open their mouth and move their jaw from left to right. A lesion of the trigeminal nerve nuclei that innervate the pterygoid muscle on that side is indicated by inadvertent jaw deviation to one side.
Diagnosis
There is no specific test to assess the condition of the trigeminal nerves, making diagnosis difficult. Other conditions that can cause facial pain and symptoms include cluster headaches, temporomandibular disorders, and sinus infections.
Your doctor may make a diagnosis based on symptoms and a physical examination. You may also receive an MRI, CT scan, or X-rays. These tests can determine whether a cyst, tumour, or artery is pressing on the trigeminal nerve.
Treatment
The recovery and treatment of trigeminal nerve disease or injury are condition-dependent. Managing the cause can help you recover faster and avoid permanent nerve damage.
Surgical considerations
Trigeminal neuralgia surgery is one of the most common surgical procedures involving the trigeminal nerve. There are two types of surgical interventions for trigeminal neuralgia: destructive and non-destructive.
By using microvascular decompression to remove any structure that may be impinging on the nerve—typically the superior cerebellar artery—non-destructive surgery aims to ease nerve compression.
Percutaneous rhizotomy and stereotactic radiosurgery are destructive procedures that completely disrupt the trigeminal nerve, rendering it incapable of transmitting pain. A damaging procedure causes permanent loss of sensation on the impaired side of the face through the ablated nerve distribution.
Rehabilitation
Techniques for rehabilitating damaged trigeminal nerves have yet to be successful. On the other hand, nerve function may be enhanced by training the nerve with occasional sensory stimulation, especially in those with reduced nasal sensitivity.
Prevention
There are no treatments that specifically improve trigeminal nerve health. However, some general measures help keep your nervous system healthy.
- Consume a balanced and nutritious diet.
- Lead a physically active lifestyle.
- Reduce stress.
- Avoid smoking and using harmful drugs.
- Get enough, restful sleep every night.
- Diseases such as high blood pressure (hypertension) and diabetes impair nerve function. Maintain control by treating them regularly
Summary
The trigeminal nerve (CN V) is the fifth and largest cranial nerve in the body, providing sensory innervation to the face. It is divided into three major branches: ophthalmic (V1), maxillary (V2), and mandibular (V3). The trigeminal ganglia connects these branches, and the ophthalmic nerve communicates with the eye, nasal cavity, face, and skull above the palpebral fissure.
The nasal cavity, sinuses, palate, maxillary teeth, middle region of the face, and skull above and below the brow are all innervated by the maxillary nerve. The mandibular nerve innervates the buccal mucosa, mandibular teeth, and the skin beneath the mouth. It is special in that it combines sensory and motor fibers. The motor parts of V3 innervate all masticatory muscles.
The trigeminal nerve senses touch, heat, cold, and pain through structures inside the skull, scalp, face, corneas, sinuses, mouth, and nose. It also transmits proprioceptive sensations from the temporomandibular joint. Trigeminal nerve injuries can cause numbness or facial pain but, but most cases regain function over time. Trigeminal neuralgia is characterized by pain emanating from the trigeminal nerve, typically affecting only one side of the face.
The trigeminal nerve (CN V) is responsible for controlling the paranasal sinuses, mucous membranes, corneas, and skin of the face and neck. Its proper function is assessed through sensory examinations, such as pain and light touch, and motor examinations. The corneal reflex, jaw jerk reflex, and lacrimal reflex are used to determine the health of upper motor neurons.
Diagnosis is difficult due to the lack of specific tests, but symptoms and physical examinations can help. Treatment is condition-dependent, with surgical interventions like trigeminal neuralgia surgery and rehabilitation techniques.
Prevention measures include a balanced diet, physical activity, stress reduction, avoiding harmful drugs, and regular treatment of diseases like high blood pressure and diabetes. Surgical interventions can be destructive or non-destructive, depending on the condition.
FAQs
What differentiates it from the trigeminal nerve?
The trigeminal nerve is the largest of the cranial nerves, and it innervates the masticatory muscles both sensory and motor. More specifically, this nerve transmits sensory information such as touch, pain, and temperature.
Which nerve is most commonly involved in trigeminal neuralgia?
Trigeminal neuralgia (TN), commonly referred to as tic douloureux, is a chronic pain condition marked by intense facial pain that flares up suddenly. It affects the trigeminal nerve, also known as the fifth cranial nerve, which transmits sensation and nerve signals throughout the head and face.
What can cause damage to the trigeminal nerve?
Trauma and injuries can harm the trigeminal nerves. Accidents, tumours, and damage from dental or facial surgery can bruise or cut nerves. A trigeminal nerve injury can affect a small area, such as a piece of gum, or a large area, such as one side of the face.
What is the main branch of the trigeminal nerve?
The superior orbital fissure, foramen rotundum, and foramen ovale, respectively, are the three distinct foramina through which the ophthalmic, maxillary, and mandibular branches of the trigeminal nerve emerge from the skull.
Is trigeminal nerve motor or sensory?
The largest cranial nerve, the trigeminal nerve (V), has a motor and sensory division. The “muscles of mastication” and the tensor muscle of the tympanic membranes of the ear are innervated by the motor division of the trigeminal nerve, which has its nucleus situated in the pons.
References:
- Huff, T., Weisbrod, L. J., & Daly, D. T. (2022, November 9). Neuroanatomy, Cranial Nerve 5 (Trigeminal). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482283/#:~:text=The%20trigeminal%20nerve%20is%20the,and%20mandibular%20(V3)%20nerves.
- The Trigeminal Nerve (CN V) – Course – Divisions – TeachMeAnatomy. (2023, July 2). TeachMeAnatomy. https://teachmeanatomy.info/head/cranial-nerves/trigeminal-nerve/
- Trigeminal Nerve. (n.d.). Physiopedia. https://www.physio-pedia.com/Trigeminal_Nerve
- Mehta, P. (2022, October 12). Trigeminal Nerve: What to Know. WebMD. https://www.webmd.com/brain/trigeminal-nerve-what-to-know
- Trigeminal Neuralgia – Causes, Symptoms and Treatments. (n.d.). https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Trigeminal-Neuralgia
- Professional, C. C. M. (n.d.). Trigeminal Nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/21581-trigeminal-nerve
- Seladi-Schulman, J. (2021, November 9). Trigeminal Nerve Overview. Healthline. https://www.healthline.com/human-body-maps/trigeminal-nerve
- Trigeminal Neuralgia. (2023, February 14). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/trigeminal-neuralgia

3 Comments