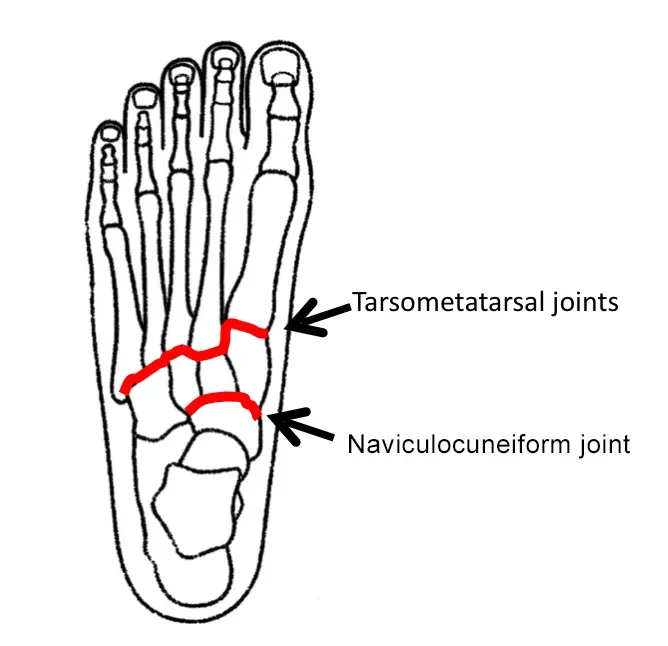
Tarsometatarsal Joints
The tarsometatarsal joints (also known as Lisfranc joints) are the articulations between the tarsal bones of the midfoot and the metatarsal bones of the forefoot. These synovial plane joints play a crucial role in maintaining foot stability and enabling movements such as walking and running. Strong ligamentous support, including the Lisfranc ligament, provides stability, while limited motion at these joints aids in transferring forces during gait.
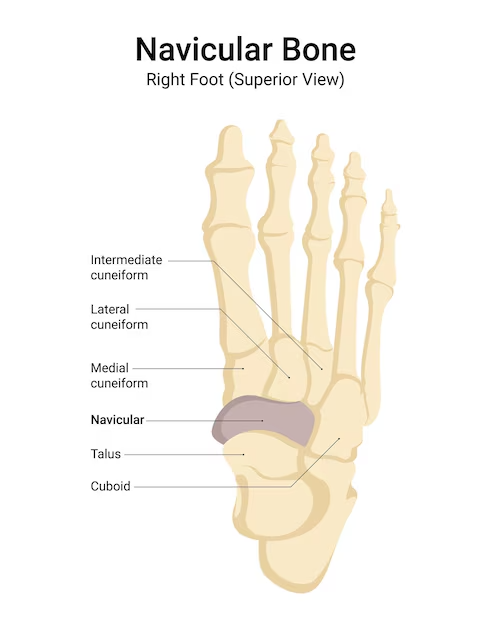
The first, second, and third cuneiform bones, the cuboid bones, and the metatarsal bones are all involved in the tarsometatarsal joints. The 18th and 19th-century surgeon and gynecologist Jacques Lisfranc de St. Martin is the namesake of the Lisfranc joint.
Introduction
Lisfranc joints, sometimes called tarsometatarsal joints, are planar synovial joints made up of articulations between the bases of the foot’s metatarsal bones and the distal surfaces of some tarsal bones. The cuboid articulates with the fourth and fifth metatarsals, the lateral cuneiform with the third and fourth, the medial cuneiform with the first, and the intermediate cuneiform with the second.
Dorsal and plantar tarsometatarsal ligaments, along with cuneometatarsal interosseous ligaments, make the tarsometatarsal joints relatively tiny and closely packed, which primarily restricts their range of motion to mild gliding.
In general, it is said that the fourth and fifth tarsometatarsal joints are more movable than the first three. While the capsules of the second and third joints and the fourth and fifth joints can communicate with one another, the first tarsometatarsal joint has its fibrous capsule.
Structure
The first, second, and third cuneiforms and the cuboid bone, which articulate with the bases of the metatarsals, are the bones that enter their creation.
The cuneiform is articulated with the first metatarsal bone; the cuboid and third cuneiform are articulated with the fourth; the cuboid is articulated with the fifth; and the second, which is firmly wedged between the first and third cuneiforms, articulates with the second cuneiform by its base.
Synovial membrane
The synovial membrane forms a unique sac between the first cuneiform and the first metatarsal.
The synovial membrane of the great tarsal region includes the space between the second and third metatarsals in front and the second and third cuneiforms behind.
Between the neighboring sides of the second and third metatarsals and between the third and fourth metatarsals, it sends forward two prolongations.
The synovial membrane forms a unique sac between the cuboid and the fourth and fifth metatarsals.
Between the fourth and fifth metatarsals, a prolongation is extended forward from it.
Ligament
The bones are held together by interosseous, dorsal, and plantar ligaments.
Dorsal ligaments
- Dorsal ligaments are flat, robust bands.
- A broad, thin band connects the first metatarsal to the first cuneiform; three, one from each cuneiform bone, three from the third cuneiform, four from the cuboid one from the third cuneiform, and five from the cuboid.
Plantar ligaments
- The longitudinal and oblique bands that make up the plantar ligaments are arranged less regularly than those of the dorsal ligaments.
- The strongest are those for the first and second metatarsals; oblique bands connect the second and third metatarsals to the first cuneiform, while a few fibers connect the fourth and fifth metatarsals to the cuboid.
Interosseous ligaments
Three types of interosseous ligaments are present.
- The first, which extends from the first cuneiform’s lateral surface to the second metatarsal’s adjacent angle, is the strongest.
- The second joins the neighboring angle of the second metatarsal to the third cuneiform.
- Third, it joins the opposite side of the base of the third metatarsal to the lateral angle of the third cuneiform.
Blood supply
The lateral plantar, medial plantar, and dorsalis pedis arteries all have branches that give blood to the Tarsometatarsal (Lisfranc) joints. Particularly:
The anterior tibial artery continues as the dorsal pedal artery.
Creates branches that support the dorsal portion of the joint, including the deep plantar artery and the arcuate artery.
A branch of the posterior tibial artery is the lateral plantar artery.
Provides support for the joint’s plantar facet and helps create the deep plantar arch.
A branch of the posterior tibial artery is the medial plantar artery.
Provides support to the tarsometatarsal region’s medial wall.
Innervation
Branches from the following nerves innervate the tarsometatarsal (Lisfranc) joints:
Deep Peroneal (Fibular) Nerve
- Facilitates the joints’ dorsal aspect
- Helps with pain perception and proprioception.
Medial Plantar Nerve (Branch of the Tibial Nerve)
- Innervates the joints’ medial surfaces, primarily the first TMT joint.
Lateral Plantar Nerve (Branch of the Tibial Nerve)
- Innervates the joints’ lateral side, primarily the TMT joints’ fourth and fifth.
- The lateral aspect of the foot could get some sensory input.
Saphenous Nerve
- Permits the medial aspect of the foot to receive some sensory innervation.
Proprioception, pain perception, and motor control—all essential for stable and mobile feet—are facilitated by these nerves.
Function
Only minimal sliding of the bones upon one another is allowed between the tarsal and metatarsal bones.
- These joints are essential for preserving the foot’s transverse arch.
- When walking or running, they aid in the transmission of force.
- They help with foot stability and flexibility on uneven surfaces.
Movement
The main gliding and rotational motions made possible by the tarsometatarsal (Lisfranc) joints help the foot become more flexible and adapt to various surfaces. The various joints move in different ways:
First Tarsometatarsal Joint (Medial Cuneiform & 1st Metatarsal)
- Plantarflexion and some dorsiflexion
- Slight rotation
Second & Third Tarsometatarsal Joints (Intermediate & Lateral Cuneiforms & 2nd/3rd Metatarsals)
- The foot arch is stabilized by the strong ligamentous support that renders these joints nearly motionless.
Fourth & Fifth Tarsometatarsal Joints (Cuboid & 4th/5th Metatarsals)
- Permit more movement than the medial joints
- Plantarflexion, some dorsiflexion, and a small amount of eversion or inversion
- An essential component of stress absorption and foot flexibility
Clinical significance
The role that the tarsometatarsal (Lisfranc) joints play in foot stability and movement makes them clinically relevant. Important clinical features include:
Lisfranc Injury (Tarsometatarsal Joint Complex Injury)
- Lisfranc joint complicated dislocation or fracture-dislocation.
- High-energy trauma (such as falls or auto accidents) or low-energy injuries (like stepping while twisting).
- Incapacity to support weight, pain, bruising, and swelling.
Arthritis of the Tarsometatarsal Joints
- The second and third TMT joints are frequently affected by osteoarthritis, which causes stiffness and pain.
- Lisfranc injuries may result in post-traumatic arthritis.
- The TMT joints may be affected by rheumatoid arthritis, which can lead to joint degeneration and abnormalities.
Pes Planus (Flatfoot)
- Foot biomechanics may be impacted by TMT joint instability, which can lead to medial longitudinal arch collapse.
- May result in discomfort and irregular walking.
Gout & Other Inflammatory Conditions
- Gout: Crystal deposition of uric acid can harm the TMT joints, particularly the first joint.
- Other circumstances: Some joints may also be affected by psoriatic or septic arthritis.
Stress Fractures & Overuse Injuries
- The stability of the TMT joint may be impacted by stress fractures in the metatarsals caused by repetitive stress, such as that experienced by sports or military personnel.
Charcot Foot (Neuropathic Arthropathy)
- Dislocation, foot deformity, and joint degeneration are common in diabetic neuropathy.
- Comprehending the clinical importance of the tarsometatarsal joints is essential for accurately identifying and treating foot conditions and injuries.
FAQs
Tarsometatarsal joints: what are they?
The intricate joints in the middle of the foot are called tarsometatarsal (TMT) joints, or Lisfranc joints. These joints serve to unite the metatarsal and tarsal bones. The metatarsal bones join the tarsal bones to the toe bones, and the tarsal bones form the foot’s arch.
What are the tarsometatarsal joint numbers four and five?
The fourth and fifth metatarsals’ bases are joined together as a single unit by the fourth and fifth intermetatarsal joints. However, due to the weaker connection of the ligaments, the articulation is more loosened than the other intermetatarsal joints.
What other name does Lisfranc’s joint go by?
The tarsometatarsal articulations are the Lisfranc joints. The lateral two metatarsals articulate with the cuboid, while the first three metatarsal bases articulate with their corresponding cuneiforms in the normal Lisfranc joint complex. The three cuneiform bones create a mortise that securely recedes into the second metatarsal base.
Are the tarsometatarsal bones long?
The middle part of the foot is called the tarsometatarsal joint or Lisfranc joint. It connects the metatarsal bones, which are the five long bones in the foot, with the tarsal bones, which are the bones in the foot arch. Lisfranc fractures can result from a violent car accident or a fall from a height.
Why do tarsometatarsal joints hurt?
Wear and Tear: Over time, osteoarthritis can develop as a result of the tarsometatarsal joints’ cartilage gradually deteriorating due to years of repetitive strain and use. This is particularly prevalent in highly active people who play high-impact sports.
References
- Wikipedia contributors. (2024b, February 11). Tarsometatarsal joints. Wikipedia. https://en.wikipedia.org/wiki/Tarsometatarsal_joints
- Tarsometatarsal joints. (2024, March 6). Kenhub. https://www.kenhub.com/en/library/anatomy/tarsometatarsal-joint