Spasticity
What is a Spasticity?
One aspect of upper motor neuron syndrome is spasticity, a motor condition characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with heightened tendon jerks as a result of the stretch reflex’s hyperexcitability.
Lance’s 1980 physiological definition of spasticity is the most well-known and frequently used explanation of the condition.”Spasticity, a motor condition defined by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with excessive tendon jerks due to hyperexcitability of the stretch reflex, is one facet of upper motor neuron syndrome.”
An upper motor neuron lesion (UMN) can cause disordered sensorimotor control, which manifests as sporadic or persistent involuntary muscle activations.
In patients with a range of neurological diseases, spasticity can lead to substantial difficulties with participation and activity. Among the numerous diverse characteristics of upper motor neuron (UMN) syndrome, spasticity is just one.
One of the characteristic features of spasticity is that the hypertonia is reliant on the speed at which the muscle is stretched; that is, more resistance is experienced with quicker stretches, leading to the clinical manifestation of a “spastic catch.” Thus, muscular lengthening and stretching are resisted by spasticity. There are two important ramifications to this.
First, there is a propensity for the muscle to stay in a shortened position for extended periods of time. This can lead to alterations in the soft tissue and eventually contractures. Secondly, there is a clear restriction on attempted motions. For instance, if the person tries to fully extend their elbow by contracting their triceps, this will cause their biceps to get stretched, which would create resistance and maybe prevent the elbow from extending all the way.
It is important to note, nevertheless, that the circumstances are typically more complicated. In the aforementioned case, biceps spasticity alleviation could not result in an improvement in arm function since other aspects of the UMN syndrome, like muscular weakness, might also be involved.
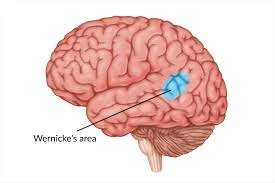
Damage or interference to the part of the brain and spinal cord in charge of regulating muscle and stretch responses is often the cause of spasticity. The imbalance between the excitatory and inhibitory impulses that the muscles receive, which causes them to lock in place, maybe the cause of these disturbances. The spasticity is due to lesions in the upper motor neurons.
Categorization of Spasticity into Different Components and Sub-Definitions
- Increased tonic component of the stretch reflex (intrinsic spasticity); exaggeration of the phasic component of the stretch reflex (intrinsic phasic spasticity; manifests as tendon hyperreflexia and clonus); and
- Exaggeration of extrinsic flexion or extension spinal reflexes is known as extrinsic spasticity.
Anatomy and Etiology:
A UMN lesion causes the spinal cord’s reflex arc to become hypersensitive and lose its downstream inhibition.
Proprioceptive, cutaneous, and other neurological functions are affected by the loss of supraspinal regulation of descending pathways that control excitatory and inhibitory Deficits arising from an upper motor neuron injury usually stemming from nociceptive spinal reflexes (UMNL).
The Inhibitory System
Corticoreticular Spinal Tract: These tracts, which are distinct from the Corticospinal Tract but travel alongside it, are in charge of facilitating the ventromedial reticular formation, an inhibitory region in the medulla. This is the site of the genesis of the Dorsal Reticulospinal Tract, which inhibits the flexor and stretch reflexes.
The Excitatory System
The bulbopontine tegmentum is the source of the Medial Reticulospinal Tract. It also functions in a weaker manner with the Vestibulospinal Tract, being both excitatory and inhibitory to the stretch and extensor reflexes, as well as the dorsal reticulospinal tract.
Different Lesions and Their Presentations
Depending on where the disruption has occurred, cortical UMN lesions and spinal cord UMN lesions have different indications and symptoms.
Normal
Due to the dynamic balance of the excitatory (Medial Reticulospinal and Vestibulospinal Tract) and inhibitory (Corticospinal Tract and Dorsoreticulospinal Tract) systems, the inhibition of the spinal cord may be readily altered in response to demand.
Corticospinal Tract Lesion
Stretch and flexor reflexes are inhibited by the Corticospinal Tract, while the major inhibitory system generated by the Dorsal Reticulospinal Tract is unaffected, maintaining the balance between excitatory and inhibitory forces.
Internal Capsule Lesion
causes a partial loss of inhibition to flexor stretches and the disruption of the Corticospinal Tract and Corticoreticular Tract pathways, which are in charge of the inhibitory response. Extensor and stretch reflexes are facilitated while flexors are inhibited due to the greater dominance of the excitatory systems from the Medial Reticulospinal and Vestibulospinal Tract.
Incomplete Spinal Cord Lesion
The location and severity will determine the signs and symptoms. There will be an unimpeded excitatory drive to stretch and extensor reflexes with partial suppression of flexor reflexes if the inhibitory system is compromised.
Complete Spinal Cord Lesion
The total lack of supraspinal control results in the absence of opposition to spinal reflexes. People may get both flexor and extensor spasms because both flexor and extensor reflexes are disinhibited.
Spasticity is seen as a positive indicator of the upper motor neuron syndrome (UMNS), which is defined as motor disorders arising from lesions in the brain or spinal cord that are close to the alpha motor neuron. Two more beneficial features of UMNS include heightened muscle stretch reflexes and upward-moving plantar reflexes.
Motor weakness, slower movement, lack of dexterity, or selective motor control are examples of negative traits. A UMN lesion causes the spinal cord’s reflex arc to become hypersensitive and to lose its downstream inhibition. Spasticity can be a symptom of a number of clinical conditions, such as multiple sclerosis (MS), stroke, cerebral palsy (CP), anoxia, traumatic brain injury (TBI), spinal cord injury (SCI), and other neurodegenerative diseases.
Epidemiology
Spasticity affects over 35% of stroke patients, over 90% of CP patients, roughly 50% of TBI patients, 40% of SCI patients, and between 37% and 78% of MS patients among the aforementioned disorders.
Caused Of Spasticity:
- An imbalance in the impulses sent to the muscles by the brain and spinal cord, which make up the central nervous system, is the cause of spasticity.
- People with multiple sclerosis, cerebral palsy, traumatic brain injury, stroke, and spinal cord injuries are frequently found to have this imbalance.
Symptoms Of Spasticity:
- Spasticity symptoms can range from simple muscular tightness or stiffness to excruciating, uncontrolled spasms. Joint pain or tightness is another typical symptom of spasticity.
- wrist spasticity
- stiffness in the muscles, which results in fewer accurate motions and makes some jobs hard to complete.
- spasms in the muscles, resulting in uncontrollably painful contractions.
- a reflexive crossing of the legs.
- Muscle fatigue.
- inhibition of the development of muscles over time.
- Muscle cell inhibition of protein production.
- increased tone in the muscles.
- Reflexes that are too rapid.
- involuntary movements, such as clonus (a sequence of rapid involuntary contractions) and spasms (a quick and/or persistent involuntary muscular contraction).
- pain and discomfort.
- reduced capacity for function and postponed motor development.
- a challenge to hygiene and caring.
- unusual position.
- Contractures are defined as permanent muscle and tendon contractions caused by extreme, ongoing stiffness and spasms.
- joint and bone abnormalities.
- Breakdown of skin shear.
- inhibits the breathing process.
- inhibits movement and gait.
- Additional effort for the caregiver.
- inadequate security.
- difficulties in sexuality.
- insomnia.
- Poor posture.
Differential Diagnosis
The conditions of rigidity, catatonia, and contractures are among the differential diagnoses for spasticity. Reduced suppleness of a muscle, tendon, ligament, joint capsule, and skin results in a contracture, which is characterized by greater resistance during passive stretching and is analogous to spasticity. The distinction between the two, though, is that contractures now exhibit any velocity-dependent alterations in limb posture or movement. Most often, damage to the basal ganglia is linked to rigidity.
Unlike spasticity, rigidity has a high tone that is non-selective and equally affects all the muscles surrounding a given joint. Like a contracture, stiffness remains constant throughout its range of motion regardless of movement speed.
The psychiatric illness known as catatonia is characterized by abnormal posture in the patient; the degree of force exerted on the affected muscle determines the degree of muscle tone increase observed. In contrast to spasticity, catatonia often exhibits comorbid symptoms such as stupor, impulsivity, perseverance, grimacing, gazing, echolalia, echopraxia, and withdrawal.
Diagnosis:
History and Physical
A patient may experience new-onset spasticity following a traumatic brain injury, stroke, or SCI. Alternatively, they could have had CP from childhood or a previous MS diagnosis, in which case their current spasticity may be new or worsening. The high muscular tone in the forearm pronators, elbow, wrist, finger flexors, and shoulder adductors are characteristic of physical exam findings. One common malformation in the hand is a “thumb in palm” deformity, in which the thumb clenches the fist and the fingers wrap around it due to excessive finger bending and adduction. The enhanced tone is particularly noticeable in the plantar flexors and invertors of the lower limbs, hip adductors, and knee flexors and extensors.
Patients experiencing spasticity including persistently high tone in the extensor hallucis longus or long toe flexors may report difficulties wearing shoes. During a physical examination, the physician will see that spasticity is correlated with movement speed; that is, the quicker a muscle is stretched or moved, the more resistance to passive elongation or stretch is observed. Clonal movements, spastic co-contractions, and spastic dystonia are other physical exam findings.
The definition of clonus is the agonist and antagonist muscles contracting and relaxing alternately. Abnormal antagonist contractions that occur during intentional agonist effort are known as spastic co-contractions. Muscle contraction that occurs at rest is known as spastic dystonia, and it results in a persistent clinical posture that is extremely sensitive to stretching.
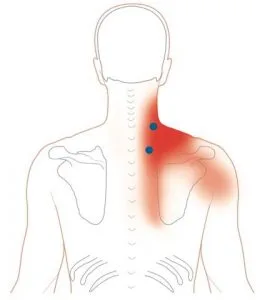
- Elevated muscular tone in the adductors of the shoulder, flexors of the elbow, wrist, and fingers, and pronators of the forearm. The hip adductors, knee flexors and extensors, plantar flexors, and ankle invertors are the lower extremities where the increased tone is most noticeable. The muscles involved in antigravity are mostly impacted.
- Patients experiencing spasticity including persistently high tone in the extensor hallucis longus or long toe flexors may report difficulties wearing shoes.
- Because spasticity is velocity-dependent, a muscle will resist stretch or passive elongation more readily when stretched or manipulated more quickly.
- It’s possible to see clonus, spastic co-contractions, and spastic dystonia. i.e., Clonus is characterized by the agonist and antagonist muscles contracting and relaxing alternately. Abnormal antagonist contractions that occur during intentional agonist effort are known as spastic co-contractions. Muscle contraction that occurs at rest is known as spastic dystonia, and it results in a persistent clinical posture that is extremely sensitive to stretching.
- The phenomenon of clasp knives: Limb refuses to move at first, but then abruptly yields
- Grabbing Effect: Applying pressure to the antagonist muscle’s surface may lessen spasticity’s tone.
Evaluation
Healthcare professionals may encounter a patient who exhibits either newly developed spasticity as a preliminary sign of an underlying neurological disorder, or pre-existing spasticity that has gotten worse due to the advancement of a recognized chronic neurologic disease or an exacerbating factor. A patient’s history and the course of their symptoms, including any motor weakness, altered sensation, pain, bladder and/or bowel dysfunction, and sexual dysfunction, are important information for a physician to gather while examining a patient who has recently developed spasticity.
A thorough history should also cover dietary habits, travel history, family history, and any weakened immune systems. A neurological assessment of the patient’s muscle tone, motor function, reflexes, and sensibility should be included in the physical examination.
A doctor must assess for triggers, illness progression, and the possibility of a new disease in a patient whose persistent spasticity is deteriorating, which is sometimes a more prevalent reason for consultation than spasticity with a recent beginning. Skin, visceral, drug-related, or device-related problems are examples of triggers.
Skin problems can manifest as infections, boils, ingrown toenails, and ulcers. Urinary tract infections, calculi, and constipation are examples of visceral problems. Spasticity may intensify if antispasmodic medications are stopped abruptly. Last but not least, triggers relating to the device may include inadequate seating, an improperly fitted orthotic, or an intrathecal baclofen pump failure. Other harmful triggers including deep vein thromboses (DVT), wounds, infections, or stress can also exacerbate spasticity.
CLINICAL PRESENTATION:
Mobility:
elevated muscular tone in the forearm pronators, elbow, wrist, and finger flexors, and shoulder adductors. The hip adductors, knee flexors and extensors, plantar flexors, and ankle invertors are the lower extremities where the increased tone is most noticeable. The muscles involved in antigravity are mostly impacted.
Walking difficulties are perhaps the most prevalent side effect of the UMN condition. Falling might become a regular occurrence, and the gait can become awkward and uncoordinated. Walking may eventually become difficult due to a combination of spasms in the flexor or extensor muscles, soft tissue contractures, and ineffective responses.
Even in cases when the affected person is unable to walk, the UMN syndrome may exacerbate their inability to maintain proper sitting posture. Having spasticity might make it challenging to push a wheelchair by yourself.
While seated on a chair, extensor spasms may propel the person forward repeatedly, increasing the possibility of shear pressures that might result in pressure sores. To keep the individual in a functional and comfortable posture, seating frequently calls for a wide range of bracing, supports, and modifications.
Loss of dexterity:
The UMN syndrome in the arm can lead to further challenges with tasks including writing, eating, taking care of oneself, and self-catheterization. Loss of arm dexterity may make it difficult to self-ambulate in a wheelchair and may limit mobility in bed. All of these issues have the potential to gradually develop dependency on a third party and impair independence.
Patients experiencing spasticity including persistently high tone in the extensor hallucis longus or long toe flexors may report difficulties wearing shoes.
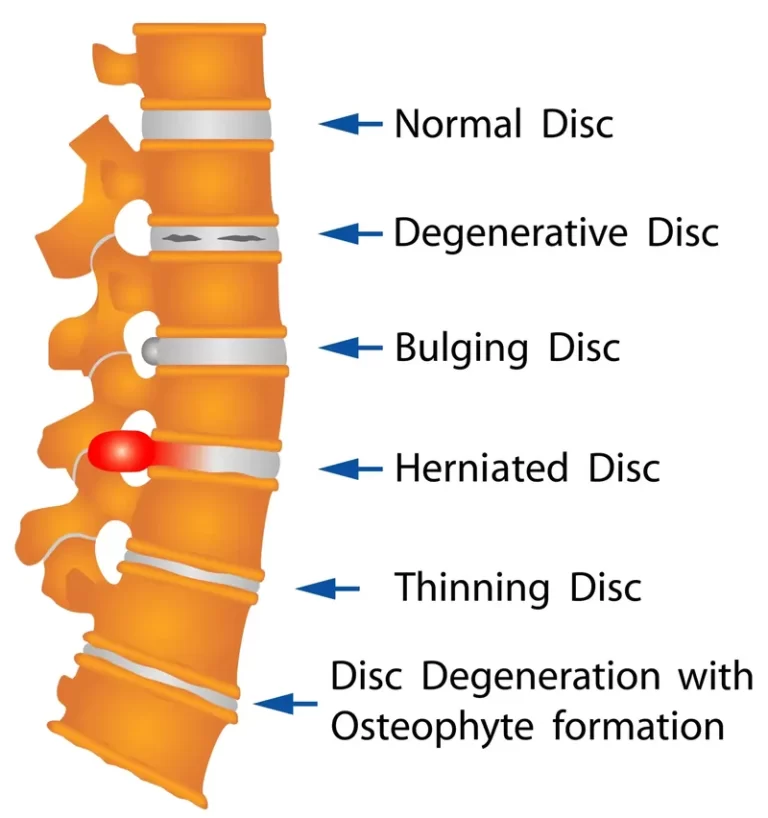
Bulbar and trunk problems:
It is important to keep in mind that truncal spasticity can lead to difficulties with sitting and keeping an upright position, which is essential for eating and communicating, even if the majority of the functional effects of spasticity are felt in the arm or leg. Difficulty swallowing may result from bulging discs, increasing the risk of aspiration or pneumonia. Further communication difficulties may result from both improper posture and spastic types of dysarthria.
Pain:
The intense p associated with spasticity and other kinds of UMN syndrome is not well acknowledged. This is especially true for flexor and extensor spasms, when analgesia alone may require therapy in order to prevent further impairment of function. A higher risk of musculoskeletal issues and osteoarthritic joint changes can also result from abnormal postures. There can be a vicious cycle of increasing pain and greater stiffness if there is any peripheral stimulation from issues like minor pressure sores or ingrowing nails.
- Because spasticity is velocity-dependent, a muscle will resist stretch or passive elongation more readily when stretched or manipulated more quickly.
- It’s possible to see clonus, spastic co-contractions, and spastic dystonia. i.e., Clonus is characterized by the agonist and antagonist muscles contracting and relaxing alternately. Abnormal antagonist contractions that occur during intentional agonist effort are known as spastic co-contractions. Muscle contraction that occurs at rest is known as spastic dystonia, and it results in a persistent clinical posture that is extremely sensitive to stretching.
- The clasp knife phenomenon is the limb’s initial resistance to movement followed by a quick yielding.
- Effect of Stroking: Applying pressure to the antagonist muscle’s surface can lessen spasticity’s tone.
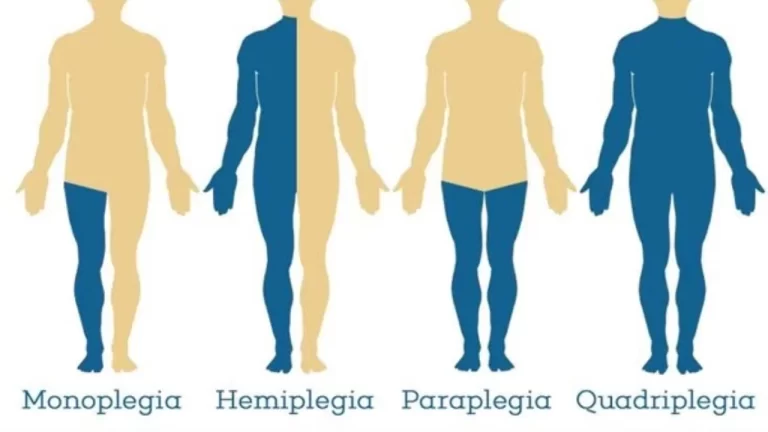
It is crucial to identify spasticity early in the diagnostic process so that it may be monitored and treated as needed. Permanent loss of joint mobility has been observed to happen 3-6 weeks following both stroke and brain damage. - Hemiplegics have lower limb patterns that include adductor spasticity and hamstring tightness restricting knee range of motion. They also exhibit plantar flexion and inversion of the ankle. Shoulder adduction, internal rotation, elbow flexion, and forearm pronation with wrist and elbow flexion are typical upper limb presentations.
Measurement techniques based on neurophysiology:
Three commonly employed methods for clinical measurement include F-wave studies, H-reflex studies, and spasticity tendon jerks.
Tendon jerks:
An example of a spinal response that is most frequently employed is the tendon jerk, which is produced by quickly (but slightly) stretching a muscle. It has been proposed that oligosynaptic routes may have an impact on the subsequent reaction, which is said to be mostly mediated by the monosynaptic pathway.
Tendon jerks have been shown to be more easily elicited in individuals with spasticity, meaning that they can be elicited at lower stimulus levels than usual and that the response to these stimuli is more diffuse and has a larger amplitude, meaning that it can involve muscles that were not initially stimulated. As a result, the tendon jerk has been proposed as a possible quantitative indicator of spasticity.
It’s crucial to remember that tendon jerk increases are not just related to spasticity. It also has to be determined if the rise in the tendon jerk response is caused by a drop in threshold, an increase in gain, or a combination of the two.
H –REFLEX
A mixed nerve is electrically stimulated submaximally to elicit the long-latency reaction known as the H reflex.
The subsequent muscular reaction is the outcome of conduction across the Ia afferent pathways. While oligosynaptic reflex pathways may possibly be implicated, the majority of these reflexes are assumed to be monosynaptic. The H-reflex response has been represented as a percentage of the M-reaction, or the stimulus of a muscle to supramaximal stimulation, in order to account for this variability.
It should be mentioned that the afferent component of the reflex reaction is assumed to be fixed when utilizing this ratio. Although investigations have indicated an increase in H/M ratios in spasticity, it has also been shown that the ratios did not drop once spasticity was treated. Additionally, it has been shown that there was little relationship between the severity of spastic hyperreflexia and H/M ratios. It has been proposed that in spastic limbs, there should be less inhibition of H-reflex activity due to the fact that in normal people, muscle vibration suppresses this activity.
F waves
F waves, which are produced by stimulating a mixed nerve above its maximum potential, are utilized to gauge the excitability of motor neurons. The F wave, in contrast to H reflexes, is the outcome of antidormic activation of the -motor neuron rather than stimulation of a sensory nerve.
Furthermore, the F wave, which comes after the M wave, has no link with M-wave amplitudes, in contrast to the H reflex, which has an inverse relationship with the M wave. Furthermore, the Fwave’s amplitude is substantially less than the H reflex’s. The average F-wave response from many tests is frequently employed due to fluctuations in latency and amplitude, even though the F-wave gives a more stable signal that is less affected by resting position and a subject’s capacity to relax. higher F-wave amplitudes in spastic people have been shown, which may indicate higher motor neural excitability.
Outcome measures:
The following are some helpful, objective metrics to track changes in spasticity:
Personal:
Pain:
Pain Numeric Scale (e.g. for stiffness, comfort, and pain)
noticing a grimace or retreat
Arms A and B
LegA
Objective:
Resting position: measurements, descriptions, and photos of bony landmarks
range of motion in passive mode
Rating of Adductor Tone
Range of motion that is active
Strength of muscles: Oxford Measure of
Modified Penn Spasms Scale of Spasm Frequency
The score for Clonus and Spasm
Description:
Walking: a ten-meter stroll
Transfers: There is a time lag
The function of the Upper Limb: 9-Hole Peg Test
Speech: The score for speech comprehension
Strolling and Dropping Result
Ashworth Scale or Modified Ashworth Scale for muscle tone
ASHWORTH SCALE:
The Ashworth scale is the measuring method most frequently applied in a clinical context. The Ashworth test is predicated on the doctor evaluating the patient’s resistance to passive stretch using the motion.
The following is the scale:
Grade Description:
- 0 No increase in muscle tone;
- 1 small improvement in tone that causes a catch when the limb is moved.
- 2 A greater rise in tone, yet the limb moved with ease.
- 3 Significant tone increase; difficult to move passively.
- 4 The limb is stiff while extending or flexing.
MODIFIED ASHWORTH SCALE:
When testing the upper extremities compared to the lower, the Modified Ashworth Scale scores showed improved reliability. The following is the scale:
Grade Description:
- 0 No increase in muscle tone;
- 1 Slight increase in muscle tone, exhibited by a catch and release or by very little resistance when the affected portions are moved in flexion or extension near the end of their range of motion.
- 1+ A little rise in muscle tone, indicated by a catch, and then very little resistance for the remaining portion of the range of motion (less than half).
- 2 A further notable rise in muscular tone across the majority of the range of motion, yet the affected area or parts are readily moved
- 3 Significantly higher muscular tone, difficult passive movement
- 4 Affected part(s) inflexible in any direction.
Tardieu Scale
This scale measures how a muscle responds to a stretch delivered at a given speed in order to quantify muscular spasticity. Grading is done consistently at the same time of day and with the body in the same posture for each leg. Reaction to stretch is assessed at a given stretch velocity for every muscle type.
Stretching
- V1 at Tardieu’s velocity as slowly as feasible
- V2 The limb segment’s falling speed (against gravity)
- V3 quickly (>gravitational pull)
Muscle Reaction Quality
- 0: There is no resistance during passive motion
- 1 Mild resistance the entire time, lacking a distinct catch at a certain angle.
- 2 Clear catch at an exact angle, then release
- 3 Attainable Clonus (less than 10 seconds) at a certain angleFatiguable Clonus (less than 10 seconds) at a certain angle
- 4 Identifiable Clonus (> 10 seconds) at a certain angle
- 5 Joint immobilized
Angle of Spasticity
- R1Angle of catch observed at V2 or V3 Velocity
- R2 When a muscle is evaluated at V1 velocity when at rest, its full range of motion occurs.
Spasticity Treatment:
The doctor must evaluate the patient’s support network, medical comorbidities, the date of the spasticity’s development, its etiology, and the overall management goals when deciding how best to treat spasticity.
Treatment choices for this condition are similar to those for other disorders in that they are step-wise, progressing from more conservative approaches to more invasive surgical treatments. One modality is identifying and avoiding uncomfortable stimuli, such as pain, infection, heterotopic ossification, pressure ulcers, urinary retention or stones, and ingrown toenails.
Physical modalities and therapies, including serial casting, heat and cold modalities, functional electrical stimulation, vibration, biofeedback, and stretching and splinting, must then be used. The Food and Drug Administration (FDA) has authorized a number of choices for pharmacotherapy at this time. These consist of diazepam, tizanidine, baclofen, and dantrolene. The most common conditions for which these systemic medications are used to treat spasticity are multiple sclerosis (MS) and spinal cord injury (SCI). They may also relieve mild to moderate spasticity. These medications have not been demonstrated to considerably enhance performance, despite the possibility that they will lessen tone and pain.
Medical Treatment:
Medication may be helpful for some people in controlling their spasticity. These interventions might be intrathecal, targeted, or generalized.
Systemic medicine is utilized if the spasticity is broad. This comprises:
Botox treatment for spasticity
For the treatment of spasticity, local injections of phenol or botulinum toxin (Botox) into spastic muscles can be quite beneficial. The muscles generating the most stiffness or spasm might have their tone specifically reduced by these injections.
In order to calm spastic muscles, your doctor will inject botulinum toxin into specific locations within your muscle. This might enhance function, posture, and comfort. Usually, the results take seven to ten days to become apparent, and they usually persist for three months.
When only a few muscular groups need to be alleviated of spasticity, this therapy is typically taken into account. It can be used in conjunction with other spasticity therapies.
Baclofen
By acting as a gamma-aminobutyric acid (GABA) agonist at GABA receptors, increases the reflex pathway’s overall inhibitory effects. Presynaptic GABA receptor activation decreases calcium influx and inhibits excitatory neurotransmitter release from the presynaptic axon. It becomes more difficult to depolarize the postsynaptic cell and lessens the impact of any excitatory neurotransmitters delivered from the presynaptic axon when postsynaptic GABA receptors are activated. This increases potassium outflow and preserves membrane polarization. Consequently, input to muscle fibers and muscle spindle sensitivity are both reduced as a result of this reduction in neuron excitability. Baclofen is side effects include tiredness and sedation, to which the patient may eventually get acclimated. Additionally, baclofen may induce gastrointestinal problems, muscular weakness, and a lowering of the seizure threshold.
Tizanidine:
Alpha-2 adrenergic agonists like this medication are chemically linked to clonidine. It functions by enhancing the presynaptic inhibition of the spinal reflex. Up to 50% of patients experience sedation and sleepiness as one of its adverse effects, along with liver damage, hypotension, dry mouth, bradycardia, and dizziness. Tizanidine is equally effective as oral baclofen or diazepam, but it is more tolerable overall, according to clinical studies. Because tizanidine is processed by the liver, there are precautions to follow when taking medication, such as routinely monitoring liver function tests (LFTs). Tizanidine’s short half-life necessitates frequent doses, and concurrent intravenous ciprofloxacin use is prohibited owing to cytochrome P450 inhibition.
Dantrolene Sodium:
Compared to other medicines, this is specific to the treatment of spasticity because it inhibits the release of calcium from the sarcoplasmic reticulum at the muscle’s peripheral level.[17] This leads to a decrease in the strength of extrafusal muscle fiber contraction and a loss in muscle spindle sensitivity. Dantrolene has little effect on cardiac or smooth muscle. The fact that 1% of people have liver damage is a significant side effect. Female patients over 30 who have been taking larger dosages for longer than two months are at the biggest risk. LFTs should be continuously monitored since liver toxicity entails a risk of hepatonecrosis. Sleepiness, sedation, weakness, exhaustion, paresthesias, diarrhea, nausea, and vomiting are other side effects.
Diazepam:
This works by enhancing the actions of GABA on GABA receptors, which ultimately results in membrane hyperpolarization and reduced neuronal activity. Overall, it results in decreased reflexes and enhanced presynaptic inhibition. Diazepam is the most sedative of the previously described antispasmodic medications. It may also result in less REM sleep and cognitive impairment. It has, however, been demonstrated to be helpful for spasticity caused by SCI and MS. Because of its side effect of impairing memory, it is frequently inappropriate for TBI patients. Due to its hepatic metabolism, diazepam can have a relatively lengthy half-life because of its active metabolites and the concomitant use of other hepatically metabolized drugs may alter its clearance.
Diagnostic Nerve Blocks:
Using electrostimulation as guidance, a local anesthetic is given perineurally to inhibit nerve transmission for a few hours. Because of the transient reduction in spasticity, the doctor can analyze the prospective advantages of longer-lasting therapies, such as chemo-neurolysis, botulinum toxin, or possibly surgery, in order to plan for more permanent interventions. These local anesthetics work by obstructing the voltage-gated sodium channels on the axon, which stops the signal from traveling down the axon and prevents the axon membrane from depolarizing. It is not recommended to inject local anesthetics into skin that is infected or cannot be thoroughly cleaned. Commonly used substances are bupivacaine and lidocaine.
Chemoneurolysis:
Chemical neurolytic treatments can work for several months or even years. Through axonal necrosis and protein denaturation, these substances induce demyelination and axonal damage. Additionally, electrostimulation or electromyography (EMG) guidance is used to inject these medicines. Phenol and ethyl alcohol are agents utilized in these processes. Usually, phenol is utilized in quantities between 2% and 7%. Lower amounts produce minor axonolysis but demyelination, which produces a momentary anesthetic effect. Higher doses have neurolytic effects that persist longer than six months and damage axons. To produce neurolytic effects, ethyl alcohol should be administered at concentrations between 45% and 100%. It is less hazardous and used less often than phenol.
Chemodenervation with Botulinum Toxin:
This is an additional course of therapy. For clinical usage, the FDA has licensed one type B toxin, rimabotuinumtoxin B, and three type A toxins, onabotulinumtoxin A, incobotulinumtoxin A, and abobotulinumtoxin A. At present, onabotulinumtoxin A is authorized for the treatment of spasticity in the upper and lower limbs in five distinct muscles, whereas incobotulinumtoxin A is permitted for the treatment of spasticity in the upper limbs. Every serotype works at the neuromuscular junction, where it prevents acetylcholine from being released presynaptically. It cleaves to the host protein SNAP-25, which is in charge of fusion, in the cytoplasm. SNAP-25 cannot fuse vesicles once they have been cleaved.
Intrathecal Baclofen Pump:
An intrathecal baclofen (ITB) pump is an additional alternative for treatment. Baclofen may now be administered directly into the intrathecal space’s cerebrospinal fluid (CSF) thanks to this gadget. With a ratio of 100:1 for the baclofen concentration at the spinal cord level when taken intrathecally vs orally, enables a patient to get a high concentration of the medication straight to the spine while reducing the CNS hazards associated with large oral dosages of the drug. The parts consist of an intrathecal catheter and a pump and reservoir that are subcutaneously implanted into the abdomen wall.
Spasticity Surgical Treatment:
Surgery for Spasticity: Dorsal rhizotomy with selection
The first line of treatment for spasticity is non-invasive, nonsurgical methods that may enhance the quality of life and function. Nevertheless, surgery could be suggested as part of the therapy approach in cases when the spasticity is severe and persistent.
Orthopedic procedures: In order to preserve function as a child develops, orthopedic surgery may entail modifying bone, muscle, and tendon. This allows for the restoration of mobility and flexibility.
Neurological surgeries: One type of neurosurgical treatment is known as selective dorsal rhizotomy, in which the damaged nerves that supply sensory data from the spastic limbs are severed at the spinal cord’s entry point. Nerves in good health are not damaged. Children with mild cerebral palsy benefit greatly from this technique, which has been demonstrated to enhance leg function and independent walking.
Intrathecal baclofen for spasticity: The insertion of a pump and a catheter to provide liquid medicine to the fluid around the spinal cord is another successful surgical procedure. This therapeutic method, known as intrathecal baclofen therapy, applies a continuous, steady supply of the spasticity-relieving medication baclofen via a pump beneath the skin. Just a brief hospital stay is necessary for the surgery to install the pump and catheter, and subsequent doctor visits are necessary to check the dose.
Intrathecal baclofen (ITB) therapy: This procedure includes putting a pump under general anesthesia in your abdomen so that it may continuously discharge a dosage of the drug baclofen into the spinal fluid via a catheter that is attached to the pump. Compared to taking baclofen orally, this can result in a considerable reduction in pain and spasticity with a decreased risk of sleepiness.
Dorsal rhizotomy with selection (SDR): An imbalance in the electrical impulses that go to certain muscles might result in spasticity. SDR physically removes certain nerve roots to correct the electrical impulses transmitted to your spinal cord. Surgeons only perform this procedure on patients whose legs have significant spasticity. Precisely slicing problematic nerve roots may reduce muscular stiffness while maintaining other functions. Typically, medical professionals recommend SDR to patients who have cerebral palsy.
PHYSICAL THERAPY TREATMENT FOR SPASTICITY :
Long stretches, positional stretches, weight-bearing exercises, exercises to strengthen the muscles in the opposing group, and the use of ice and cold packs are the primary physical therapy treatments used to alleviate spasticity. The consequences of these exercises are as follows:
minimizing alterations to the connective tissue’s viscoelastic features;
modifying the brain circuitry underlying spasticity or spasms, and preserving the person’s functional levels.
Standing:
tilt table/standing frame: It is hypothesized that the advantages of standing on a tilt table or standing frame stem from the following: decreasing lower limb spasms, maintaining or improving soft tissue and joint flexibility, stimulating anti-gravity muscle activity in the trunk and lower limbs, modulating the neural component of spasticity through prolonged stretch and altered sensory input, and having a positive psychological impact.
Stretching Exercise to Reduce Spasticity :
Unwind Long-term muscular stretching and passive movement are very helpful in lowering spasticity.
Stretch therapies work by affecting the extensibility of the soft tissues that cover the joints in an effort to preserve or improve joint mobility. Stretch therapies can be physically done by therapists or self-administered by patients.
Soft tissues are mechanically extended for variable lengths of time in all procedures. Certain procedures have a limited duration of application. Stretches may be applied over extended periods of time using several methods, such as placement. When it comes to providing continuous stretch for several days or even weeks, splints or serial casts are utilized to supply stretch for even longer durations.
How ICE is Used for Reducing Spasticity?

Ice Pack: Clinically, localized application of ice is used to lessen or completely eliminate clonus and to lessen the resistance of spastic muscle to fast stretching. Three methods exist for applying cold to the body:
- (1) soaking in cold water;
- (2) massaging with ice cubes or packs; or
- (3) employing evaporative sprays, such as ethyl chloride. It has been claimed that a safe intramuscular temperature of 30°C can prevent a full conduction block of nerve fibers. The change in muscle caused about by cold treatment may have a retrograde effect on the spinal cord’s excitability, reducing spasticity.
The change in muscle caused about by cold treatment may have a retrograde effect on the spinal cord’s excitability, reducing spasticity. This might be proposed as one of the ways that cold treatment reduces spasticity. Decreased spasticity may also result from modifications made to the mechanical characteristics of muscles during cryotherapy.
How HOT PACK are used for reducing spasticity?

Patients with spasticity benefit greatly from hot pack therapy, or taking a bath in hot water. This method has been utilized to modify motor neuron excitability in stroke survivors experiencing spasticity. Following the use of thermotherapy (e.g., submerging muscles in water at 41°C for 10 minutes), alterations in spastic muscles have been illustrated using the F-wave characteristics (amplitude, F-wave/M-wave ratio) of motor-neuron excitability. Following thermotherapy, a drop in F-wave characteristics has demonstrated the treatment’s anti-spastic properties.
Static Positioning:
The impact of a muscle’s length on stretch reflex activation is referred to as muscle length positioning. Given that spasticity is known to be length-dependent, patients’ positions during testing may have an impact on the assessment’s findings, especially when bi-articular muscles are involved. It has been shown that varied postures affect stretch reflex activity, with supine positions showing greater Root mean square (RMS) values of muscular activity in spastic muscles than seated positions.
A muscle in an extended condition has more stretch reflex activity than a muscle in a shortened state, which may be the result of changes in intrinsic muscle properties. This issue needs to be considered while using various strategies to assess and treat spasticity.
Reflex inhibitory thermoplastic splinting/orthotics:

The goal of splinting is to modify muscular extensibility, depending on the degree of stretch produced by the splint. Wrist splints are supposed to prevent or minimize contracture. It has been demonstrated that stretching and static passive motions of spasticity-affected joints improve motor neuron excitability, increase flexibility, and lessen tensile stress on soft tissues. Thus, reduced spasticity seems to be the outcome of both reflexive and mechanical processes working together. Whether passive exercises or stretching in a weight-bearing or non-weight-bearing position is better for decreasing spasticity is not well understood.
Mechanical gait trainer (treadmill training)
The patient walks on a treadmill while wearing the mechanized gait trainer, which supports a portion of the patient’s body weight via a harness and overhead suspension system. The apparatus regulates the center of mass in both vertical and horizontal directions, stimulates the phases of gait, and supports the patients in accordance with their capacities. It has been shown to lessen stiffness by enabling postural and stepping response training at an early age. It makes gait cycle motor relearning easier.
- reduction of uncomfortable stimuli.
- Positional stretching and activities involving weight bearing.
- Extended Stretching of Muscles.
- Physical techniques such as heating, cooling, and icing.
- Electrical stimulation:
In order to restore the proper balance between your flexor and extensor muscles, electrical stimulation is occasionally utilized to re-educate muscles. When stimulation is first administered, the effects typically persist for around ten minutes, although they may continue longer after a few months. - Orthoses: Also referred to as casts, braces, or splints, orthoses are any devices that are used to improve the function of the body’s moveable components or to support, align, prevent, or repair abnormalities. Orthoses can decrease muscular tone, enhance or maintain range of motion, and shield the skin from harm—such as the deterioration that would happen in your palm if your hand were always clenched—when used to treat spasticity.
Postoperative and Rehabilitation Care
In many cases, rehabilitation is essential to controlling a patient’s spasticity. In addition to pharmaceutical treatments, it is important to consider the utilization of the physical modalities and therapies previously discussed. It is vital to include the patient, the family, and any other caregivers in controlling spasticity and to agree on the intended goals of treatment and management. It is essential to recognize and keep away from any potentially harmful stimuli while continuing regular range-of-motion and stretching activities.
Prognosis
From patient to patient, the prognosis for spasticity might vary greatly. In terms of symptomatic spasticity management, a patient may have a good prognosis if their spasticity responds well to treatment, whether it be physical modalities, therapy, or pharmaceutical intervention. Furthermore, as was already indicated, spasticity may benefit the patient in other ways, such as assisting with walking and avoiding deep vein thrombosis (DVTs), preserving muscular mass, and preventing osteoporosis through weight bearing.
Complications
The consequences of spasticity might differ. When severe, spasticity can make it difficult to go about daily tasks. It can interfere with cleanliness and the caregiver’s ability to deliver care, as well as cause the patient to experience excruciating agony or suffering. Thus, there may be a higher chance of pressure ulcers forming, which may result in infection and sepsis. In addition, it raises the risk of heterotopic ossification and can result in dislocation, subluxation, and bone fractures.
Conclusion
Spasticity is a prevalent sign and characteristic of several neurological disorders. The degree of spasticity you experience might vary from a small annoyance to a major hindrance to your daily routine. Fortunately, there are several approaches to treating spasticity. Your healthcare team and you will collaborate to choose the most appropriate course of therapy for you.
FAQs
Does spasticity disappear by itself?
It is caused by damage to the spinal cord in patients suffering from stroke, traumatic brain injury, cerebral palsy, or other disorders affecting the brain or spinal cord. Since the damage in cerebral palsy is irreversible, real spasticity in the condition does not go away on its own.
When is the onset of spasticity?
In the first month following a stroke, spasticity occurred in around half of the patients. Post-stroke spasticity, however, can appear more than three months following the commencement of the stroke. Thus, even in the chronic stage, it is critical to evaluate spasticity.
Do you have spasticity when walking?
Spasticity, a condition where muscles feel heavy, tight, and difficult to move, may be an indication of multiple sclerosis. When spasticity affects the lower limbs, walking and other activities may become more challenging.
Does heat help with spasticity?
Muscle spasms as a result of nerve root irritation or musculoskeletal disease have decreased. Heat also lessens spasticity, although its effects are transient and unhelpful for muscle retraining. Cold efficiently diminishes the spasticity of upper motor neuron origins.
Does spasticity damage the nerves?
Damage to the area of the brain responsible for controlled movements is a common cause of spasticity. Damage to the spinal cord’s nerves may possibly be the cause. Among the signs of spasticity are: unusual posture.
How can leg spasticity be stopped?
Drugs for spasticity
There are several drugs used to treat spasticity, such as the injection of botulinum toxin directly into muscles that spasm. Baclofen: a sedative. The sedative diazepam.
In physical treatment, how may spasticity be reduced?
Using ice to lessen the frequency and pain of spasms is one way that physical therapy treatments might help reduce spasticity. extending muscles to their maximum length to reduce stiffness in the surrounding tissue and joints.
How painful is spasticity?
Spasticity-related pain can range in intensity from a dull sensation akin to taut muscles to excruciating spasms in the limbs, notably the legs. In addition to causing sensations of pain or stiffness in and around joints, spasticity can also result in lower back pain.
How can someone who is spastic sleep?
It could help to sleep on one side or with a pillow beneath your knees. Perhaps an occupational therapist can provide assistance. To ensure that your medication is at its most effective when you need it, try taking it around 30 minutes before going to bed if you take it for muscle stiffness or spasms.
How can muscular spasticity be prevented?
You can learn stretches, postures, and exercises from physical and occupational therapy that can help you keep your range of motion. The treatments can aid in preventing contracture, or the shortening and tightening of muscles. oral medications. A few oral prescription medications may be able to lessen muscular stiffness.
How is spasticity treated?
The most popular treatments for spasticity are injections and oral medications; however, your doctor may suggest further physical rehabilitation based on the severity of your spasticity.
What sorts of spasticity are there?
Exaggeration of the phasic component of the stretch reflex, which can cause tendon hyperreflexia and clonus, is known as intrinsic phasic spasticity. Exaggeration of extrinsic flexion or extension spinal reflexes is known as external spasticity.
How is spasticity measured?
tests for spasticity and its severity will involve a physical examination and neurological tests. Imaging techniques like magnetic resonance imaging (MRI) can reveal more details about the degree of damage-causing spasticity as well as its etiology.
Which exercise is ideal for those with spasticity?
Imagine a thread tugging from the top of your head as you begin by sitting on a chair. With your fingers pointing inside, place your hands on your thighs and start to alternately shift your weight. After a few seconds of holding the posture on each side, repeat six to ten times.
Can spasticity be treated?
The outlook for spasticity
But spasticity resulting from other disorders, including cerebral palsy, is irreversible damage, meaning the spasticity symptoms will not go away on their own. However, certain therapies could reduce pain and enhance functionality.
Which is better, spasticity or spasm?
A sign of spasticity is that your muscles seem heavy, rigid, and difficult to move. A muscle spasm is an abrupt, uncontrollable tightening or contracting of the muscle. The interior springiness of muscles is similar to that of a gently wrapped spring. It feels like the spring is wound too tightly in a spastic muscle.
What causes a spastic reaction?
Damage or interference to the part of the brain and spinal cord in charge of regulating muscle and stretch responses is often the cause of spasticity. The imbalance between the excitatory and inhibitory impulses that the muscles receive, which causes them to lock in place, may be the cause of these disturbances.
What do rigidity and spasticity mean?
Furthermore, faster movement elicits a greater involuntary contraction, or “catch,” of the affected muscles in cases of spasticity. Rigidity causes the elevated muscle tone to stay consistent across the affected joint’s range of motion.
What signs of spasticity are present?
Among the signs of spasticity is: Improper posture.
owing to tense muscles, carrying the arm, finger, wrist, and shoulder at an unusual angle.
heightened deep tendon reflexes (such as the knee-jerk reflex)
clonus, or repeated jerky movements, especially in response to touch or movement.
References
- Professional, C. C. M. (n.d.). Spasticity. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/14346-spasticity
- Spasticity. (n.d.). Physiopedia. https://www.physio-pedia.com/Spasticity
- Rivelis, Y., Zafar, N., & Morice, K. (2023, August 8). Spasticity. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507869/
- Dhameliya, N. (2023, April 27). Spasticity : Cause, Symptoms, Physio Treatment, Exercises. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/spasticity-treatment/
- Physiotherapist, N. P. (2022, February 17). Spasticity of Muscles : Grades, Treatment, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/techniques-to-inhibit-spasticity-with-physiotherapy-treatments/


9 Comments