Scoliosis
What is a Scoliosis?
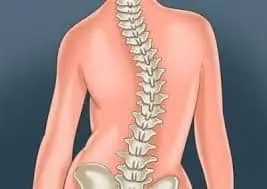
Scoliosis is an abnormal lateral curvature of the spine that causes abnormal twisting. The rib cage on one side of the body may protrude more than usual due to the twisting of the spine, and The side-to-side curvature may cause unequal hips and/or shoulders, among other postural abnormalities.
People with scoliosis frequently have stable spinal curvature, which means their curve does not vary over time. On occasion, though, it gets worse with time and frequently needs medical treatment. For example, during periods of rapid growth throughout puberty, teenagers may have a more severe curvature of the spine. Furthermore, there is a general increased risk of progression for spines with a larger degree of curvature.
Scoliosis can affect children and adults, but it usually first manifests in childhood or adolescence. The disorder in adults may have started in childhood or adolescence and subsequently persisted throughout maturity.
Adult-onset scoliosis can sometimes result from trauma, neuromuscular disorders, osteoporosis, degenerative changes in the spine, or other medical conditions.
Anatomy of Scoliosis
It is essential for individuals with spinal problems to have an understanding of the structure and functioning of the spine. It starts by giving a “big picture” overview of the regions, main curvature, and functions of the spine. This is followed by thorough details on individual anatomical features such as vertebrae, intervertebral discs, the spinal cord and nerve roots, joints, muscles, and ligaments.
Functions of the spine
The spine’s three primary functions are as follows:
Protect the body’s interior organs, spinal cord, and nerve roots.
To keep your posture straight, provide yourself with balance and structural support.
Make flexible motion possible.
Regions of the spine
The cervical, thoracic, lumbar, and sacral parts of the spine are usually divided into four primary regions. Each region has its own special characteristics and functions.
Cervical Spine
The Cervical Spine refers to the area of the spine that is in the neck. The seven vertebrae that make up this region are known to as C1 through C7 (top to bottom). These vertebrae support the skull, protect the spinal cord and brain stem, and allowing a full range of movement of the head.
Thoracic Spine
The Thoracic Spine consists of 12 vertebrae located under the last cervical vertebra. T1 through T12 have been shortened (from top to bottom). The smallest thoracic vertebra is T1, while the largest is T12. The spinous processes of the thoracic vertebrae are longer and bigger than those of the cervical bones.
The thoracic spine is strengthened by rib attachments along with longer spinous processes. The thoracic spine is more stable because of these components than the cervical or lumbar areas. The rib cage and ligament systems also protect a number of important organs and restrict the range of motion of the thoracic spine.
Lumbar Spine
The five vertebrae of the lumbar spine are referred to as L1 through L5 (the biggest). Each lumbar vertebra is sized and shaped to support the majority of the weight of the body. Comparable structural elements in the cervical and thoracic areas are smaller, narrower, and less broad than those in the lumbar vertebra.
Compared to the thoracic spine and the cervical spine, the lumbar spine has a greater range of motion. Rotation is restricted by the lumbar facet joints, although considerable flexion and extension movement is possible.
Sacral Spine
The sacrum is placed behind the pelvis. The sacrum is made up of five bones that are combined to form a triangle (abbreviated S1 through S5). The sacrum, which connects the spine to the pelvis, rests between the two hipbones. The sacrum and the final lumbar vertebra (L5) articulate, or move, together. The Coccyx, or tailbone, is made up of five extra bones that are fused together just below the sacrum.
Spinal planes
Normal curves in the spine occur at the cervical, thoracic, and lumbar areas in what is known as the “sagittal” plane. The head is positioned above the pelvis by these anatomical curves, which also serve as shock absorbers to distribute mechanical stress during movement. A common definition of scoliosis is spinal curvature in the frontal, or “coronal,” plane. Although the coronal plane is used to measure curvature, scoliosis actually describes a more complex, three-dimensional issue involving the following planes:
- Coronal Plane
- Sagittal Plane
- Axial Plane
The coronal plane, which divides the body into anterior (front) and posterior (back) parts, is a vertical plane that runs from head to foot and parallel to the shoulders. The right and left halves of the body are divided by the sagittal plane. The coronal and sagittal planes are perpendicular to the ground, while the axial plane is parallel.
In addition to vertebral rotation in the transverse plane and hypokyphosis in the sagittal plane, scoliosis is characterized by Cobb’s angle of spine curvature in the coronal plane. The rib cage, costal-vertebral joints, and spine abnormalities produce “convex” and “concave” hemithoraxes. The more severe the scoliosis, the earlier the rotation component is started. This condition, known as torsion-scoliosis, results in a gibbus.
Vertebral structures
All vertebrae, except the first two cervical vertebrae, are made up of the same fundamental components.
Cortical bone makes up a vertebra’s outer shell. This kind of bone is strong, dense, and solid. The weaker cancellous bone—which resembles a honeycomb of loosely linked structures—found inside each vertebra is called cancellous bone. The cavities in cancellous bone contain bone marrow, which produces red blood cells and certain types of white blood cells.
The following elements are common to vertebrae:
Vertebral Body: the largest part of vertebrae. It usually has an oval-like form when viewed from above. The vertebral body resembles an hourglass when viewed from the side, with thicker ends and thinner middles. Strong cortical bone covers the body, while cancellous bone is found inside.
Pedicles: The two short processes that extend from the back of the vertebral body are made up of strong cortical bone.
Laminae: There are two comparatively flat bone plates that meet in the middle after extending from each side of the pedicles.
Processes: Articular, transverse, and spinous are the three types of processes. Ligaments and tendons are connected by these processes. The four articular processes produce the facet joints by joining forces with the articular processes of neighboring vertebrae. Spinal motion is made possible by the intervertebral discs and facet joints. The spinous process functions as a lever to alter vertebral motion and extends posteriorly from the junction of the two laminae.
Endplates: An endplate “coats” the superior and inferior surfaces of each vertebral body. Endplates are complex structures that support the intervertebral disc by “blending” into it.
Intervertebral Foramen: The bottom surface of the pedicles has a deep notch, whereas the upper surface has a minor notch. The intervertebral foramen is the region formed by the pedicle notches when the vertebrae are stacked on top of one another. Since the nerve roots that supply the rest of the body leave the spinal cord through this region, it is vitally important.
Facet joints
The spinal column’s joints are situated posterior to the vertebral body, or on the back. The spine can bend, twist, and extend in various directions with the assistance of these joints. While these joints allow for mobility, they also prevent overextension and hyperflexion (i.e. whiplash).
There are two facet joints in each vertebra. With the inferior articular facet (below), the superior articular facet functions as a hinge, facing upward.
Similar to other joints in the body, synovial fluid is produced by each facet joint to lubricate and nourish it. Each facet joint is enclosed in a capsule of connective tissue. Cartilage covers the joint surfaces, facilitating smooth joint motion or articulation.
Intervertebral Discs
There is a “cushion” between each vertebral body called an intervertebral disc. Through the absorption of shock and strain during movement, each disc prevents the vertebrae from grinding against each other. The largest structures in the body without blood flow are the intervertebral discs. Each disc gets necessary nutrients by osmosis.
Each disc consists of two components: the annulus fibrosis and the nucleus pulposus.
Annulus Fibrosus
The nucleus pulposus is located in the core of the annulus, a strong, tire-like structure that surrounds it. The annulus helps the spine withstand compressive stress and improves its rotational stability.
Water and layers of strong, elastic collagen fibers make up the annulus. The strands are arranged horizontally at various angles, resembling the design of radial tires. Strong, interconnected protein bundles are what give collagen its strength.
Nucleus pulposus
Every intervertebral disc has a gel-like, elastic material filled in its middle. The nucleus pulposus transfers weight and stress from vertebra to vertebra along with the annulus fibrosis. The nucleus pulposus consists of collagen, proteoglycans, and water, the same as the annulus fibrosus. However, the ratio of these compounds within the nucleus pulposus varies. There is more water in the nucleus than in the annulus.
The Nerve Roots and Spinal Cord
A thin, cylindrical structure roughly the width of a little finger makes up the spinal cord. Starting right below the brain stem, the spinal cord goes all the way to the first lumbar vertebra (L1). After that, the cord combines with the conus medullaris to form the cauda equina, a collection of nerves that resembles a horse’s tail. Movement and sensation are stimulated by the spinal nerve roots. The intervertebral foramen, which are small apertures between each vertebra, is where the nerve roots leave the spinal canal.
The Central Nervous System (CNS) is made up of the brain and spinal cord. The Peripheral Nervous System (PNS) is made up of nerve roots that leave the spinal cord and spinal canal and spread out throughout the body.
The spinal canal, which houses the spinal cord and the intervertebral foramen, is located between the front and rear portions of the vertebra (also known as the mid-region). The foramen are small openings that develop in between each vertebra. The nerve roots can pass through these “holes” in order to leave the spinal canal and branch off to form the peripheral nervous system.
Ligaments, muscles, and tendons ligament
Fibrous bands of connective tissue that attach to bone are called tendons and ligaments. Ligaments serve to support joints in addition to joining two or more bones together. Muscle and bone are joined via a tendon. They come in different sizes and have some give.
Causes of Scoliosis
Some of the potential causes of scoliosis are listed below:
Neuromuscular conditions: these diseases affect both the muscles and nerves. These involve muscular dystrophy, poliomyelitis, and cerebral palsy.
Certain genes: It is thought that the development of scoliosis is triggered by at least one gene.
Leg length: An individual may acquire scoliosis if one leg is longer than the other.
Syndromic scoliosis: Neurofibromatosis and Marfan’s syndrome are two conditions in which scoliosis can occur as a side effect.
Osteoporosis: As a result of bone degeneration osteoporosis can lead to secondary scoliosis.
Other causes: include connective tissue disorders, bad posture, carrying satchels or backpacks, and certain traumas that can result in spine curvature.
Risk factor
Age
Scoliosis symptoms typically start between the ages of 10 and 18 during puberty. It’s possible that you’ll discover your youngster has uneven hips or that the backpack straps come off of one shoulder too readily. Additionally, you may observe that your child has unequal ribs.
Gender
Females are more likely to develop scoliosis than boys. Additionally, girls who are taller are more likely to develop scoliosis. According to some researchers, the hormone leptin may be involved in this problem. The body’s energy levels and food intake are regulated by leptin. Reduced bone mass has been linked to low leptin levels, and this can cause scoliosis to develop.
Developmental delay and genetic syndrome
Scoliosis is more common in patients with chromosomal abnormalities or genetic diseases. Among these conditions is Down syndrome. Scoliosis is essentially caused by developmental delays that interfere with a child’s normal growth process.
Prematurity
Individuals who experience an early birth are more likely to develop to scoliosis. Premature babies may have a spine that is underdeveloped because the spine develops at exactly the same time as other organs.
A family history of scoliosis
Although scoliosis can run in families, most affected youngsters do not have a family member who also has the disorder. However, a person’s likelihood of developing scoliosis is increased if they have a parent or sibling who has the condition.
Types of Scoliosis and Their Known Causes
1. Idiopathic scoliosis
The most common type of scoliosis is idiopathic. A medical condition for which there is no known cause is referred to as idiopathic. A patient’s age at diagnosis helps to further define idiopathic scoliosis.
During normal physical examinations, idiopathic scoliosis patients are frequently diagnosed. Scoliosis may be mentioned by pediatricians or family doctors at a yearly checkup or during a sports physical. During health checks carried out in school settings, certain people are recognized.
Occasionally, an asymmetrical shoulder, hip, or curved spine is noticed by a patient or family member, which inspires a visit to the doctor. Some people get scoliosis symptoms, which prompt the sufferer to seek medical care. The age of the patient at the time of diagnosis determines the classification of idiopathic scoliosis.
classified into the follow-up subtypes:
A. Infantile Scoliosis
An abnormally shaped lateral curvature of the spine that affects newborns and toddlers is known as infantile scoliosis. The term “condition” refers to scoliosis in children under the age of three. between the ages of 0 and 3 years, infantile scoliosis develops, with a 1% frequency.
Idiopathic scoliosis includes the type known as infantile scoliosis. “Idiopathic” means an unclear its cause. Less than 1% of children with idiopathic scoliosis also have infantile scoliosis, despite idiopathic scoliosis being the most frequent kind of scoliosis.
Scoliosis in infants does not present with x-ray detectable skeletal abnormalities at birth. As an example, congenital scoliosis affects children from birth. The onset of symptoms usually happens by the time the baby is six months old. Boys are more likely than girls to have infantile scoliosis.
In most cases, infantile scoliosis does not cause pain. However, it’s critical to keep a careful eye on the situation. Even while the majority of infantile scoliosis cases resolve on their own, the disorder can occasionally result in severe deformity.
Casting and bracing are usually effective treatments for infantile scoliosis in children. Only a very small number of kids require spine surgery.
B. Juvenile scoliosis
Scoliosis that is initially diagnosed between the ages of 4 and 10 is commonly referred to as juvenile idiopathic scoliosis. This group includes between 10% and 15% of all pediatric cases of idiopathic scoliosis.
Boys are affected slightly more than females at the younger end of the spectrum, and the curve is frequently skewed to the left. The disease is more common in girls at the upper end of the age range, and the curve tends to lean to the right.
Juvenile scoliosis patients typically have a significant risk of their curve worsening. Scoliosis bracing is necessary for the active treatment of seven out of ten youngsters whose condition worsens.
C. Adolescent Idiopathic Scoliosis
The most common type of scoliosis is called adolescent idiopathic scoliosis, and it is typically diagnosed in patients between the ages of 10 and 18. Since this kind is idiopathic, its exact cause is unknown; however, we do know how to manage it going ahead, and that growth is the primary progressive trigger for the disorder. When it comes to scoliosis, progression indicates the enlargement of the scoliotic curve.
A disease might go from mild to moderate, from severe to extremely severe. There is no certain way of predicting with 100% accuracy how quickly one patient will progress in comparison to another, even if every case is different and the various classification points shape characteristics like progressive rate.
The most typical signs of AIS are postural abnormalities that impact the body’s overall symmetry. Again, each case is unique, but the degree of the problem will determine how obvious these abnormalities are. Uneven shoulders and hips are classic indicators of scoliosis in teenagers. This type is also distinct in that it might be difficult to diagnose in its early stages, even though there is no guarantee that therapy will be successful. However, early discovery can raise those odds.
Since modest forms of the condition might be difficult to detect early because of their delicacy, most of my patients have already progressed from mild to moderate when their diagnosis is based on more obvious symptoms.
A scoliotic curve’s compressive force is countered in patients who are still growing by their spines continuously lengthening until they achieve skeletal maturity. Compression of the spine and its accompanying ligaments, muscles, and nerves due to the uneven forces produced by scoliosis is believed to be the primary cause of discomfort associated with the condition. Adult scoliosis differs from other conditions in that pain is felt differently after a problem becomes compressive in maturity.
2.Degenerative Scoliosis
Degenerative scoliosis is also referred to as adult-onset scoliosis, late-onset scoliosis, or de novo scoliosis. The characteristic of degenerative scoliosis is a sideways curvature of the spine that gradually appears in adulthood. Degeneration of the spine’s joints and discs is one of the inevitable effects of aging. One side of the spine may exhibit more prominent spinal curvature than the other due to uneven “wear and tear” of these discs and joints. a scoliosis characteristic.
Loss of bone health is frequently linked with degenerative scoliosis.
Degenerative scoliosis is characterized by a small C-shaped deformity that primarily affects the lumbar spine or lower back. Scoliosis is diagnosed when the sideways curvature (as determined by the Cobb angle) is more than 10 degrees.
Degenerative scoliosis can be painful, even though many other types of scoliosis don’t hurt. Typical symptoms consist of:
- A dull pain or stiffness in your lower back
- A pain that radiates and spreads down the legs,
- a sense of tingling down the leg,
- or an intense pain in the leg that goes away when you rest but returns when you walk.
More than 60% of people over 60 may have some degenerative scoliosis, according to a recent study on adult scoliosis. Age-related degeneration of the spine is the cause of de novo scoliosis.
Adult patients who have never experienced scoliosis before experience it.In adults who are over 50, x-rays and a physical examination are used to diagnose it. Symptoms in the legs, such as numbness or paralysis, stiffness, and pain in the back are common in patients with de novo scoliosis.
Patients frequently experience loss of balance and bad posture over time. Due to the risks involved with back surgery in the elderly, treatment is difficult.
3.Congenital scoliosis
Congenital scoliosis occurs at birth, although no genetic or familial component has been identified. The spine develops abnormally in the womb; it starts early in development and usually finishes by the sixth week of pregnancy. There are mainly two types of congenital scoliosis: unilateral bar and hemivertebrae. Both may have an effect on one or more vertebrae.
Hemivertebrae are the most prevalent kind of congenital deformity; they are vertebrae that are not fully developed. Because the spinal vertebrae are stacked on top of each other, the hemivertebrae serve as a ‘wedge’ and cause the spine to curve.
A unilateral bar, also known as a block vertebrae, is a spinal fusion caused by the vertebral bodies’ inability to separate into a single, unique vertebra during creation. An abnormal curvature may result from only one side of the vertebral bodies growing due to inadequate separation.
When both congenital defects happen at the same time, a more serious condition may result. Congenital scoliosis is usually discovered during a newborn examination, but because the deformity may not be visible at birth, the spine may not curve, it is frequently missed until puberty.
4.Neuromuscular Scoliosis
Secondary neuromuscular scoliosis develops as a result of another disease. When there is poor communication between the brain and muscles, spinal curvature develops. It is possible for this curvature to worsen in people who are unable to walk as they get older. Wheelchair-bound patients may find it difficult to sit up straight and may lean to one side more often than not.
Some of the underlying disorders that have been linked to neuromuscular scoliosis are:
- Myelodysplasia,
- cerebral palsy
- Duchenne muscular dystrophy.
- The Freidrich ataxia
- Spinal muscular atrophy.
Neuromuscular scoliosis is usually not uncomfortable unless the spinal curvature gets severe.The change in posture is frequently the initial indication of scoliosis. either when sitting orstanding, bending forward or to one side.full spinal x-rays and clinical examinations typically reveal a long, C-shaped curvature affecting the entire spine.
An understanding of the many forms of scoliosis can be built upon a foundation of knowledge regarding the classification of spine curvature problems.
Types of Scoliosis Patterns
1.Thoracic scoliosis
Thoracic scoliosis is the most common type of curvature, occurring when the scoliotic curve forms in the middle or upper part of the thoracic spine. since the thoracic spine, which consists of the T1 through T12 vertebral bodies, is the longest spinal segment, this makes explanation.
The formation of a rib arch is a characteristic of thoracic scoliosis because the abnormal spinal curvature can pull on the rib cage, causing it to move in position and one side protrudes more than the other. Furthermore, one leg appearing longer than the other and/or unequal shoulders are frequently linked to this region of curvature.
2.Lumbar Scoliosis
The development of an abnormal spinal curvature in the lower back is known as lumbar scoliosis. uneven hip and leg lengths are known to result from lumbar scoliosis because it applies uneven forces to the lower body.
Additionally, given the sciatic nerve originates in the lower back and travels down the buttocks, back of the leg, and foot, sciatica is a frequently occurring complication of compressive lumbar scoliosis in adults. Compression-related back and/or radicular pain can range in severity from minor to severe, depending on the extent of nerve involvement.
Lumbar scoliosis that appears later in life can be categorized as degenerative since the lumbar spine is the most susceptible to spinal degeneration due to its heavy weight bearing capacity.
3.Thoracolumbar Scoliosis
When a person has thoracolumbar scoliosis, their spine curves include vertebrae from both the upper and lower lumbar regions. It is frequently congenital, manifesting at birth and developing in the 3rd to 6th week of pregnancy. It might potentially be a side effect of a neuromuscular disorder (such cerebral palsy or spina bifida).
Females are more likely than males to develop thoracolumbar scoliosis, which typically results in a curvature toward the right.
Types of Scoliosis Spinal Curvature
The human spine’s side view shows natural curves that assist absorb the pressures of everyday movement. A healthy spine shows moderate bends when viewed from the side and runs straight down the middle of the body when viewed from the back. The abnormal lateral curving of the spine that results from scoliosis can be moderate or severe. The spine may curve backward or inward due to other conditions.
1.Dextroscoliosis
An abnormal sideways curvature of the spine that points to the right is called dextrocurvature and is characteristic of dextroscoliosis. (Levoscoliosis is a condition in which the spine curves left.)
One of the more prevalent forms of scoliosis, dextroscoliosis can give the spine a “S” or “C” shape, depending on how severe it is. Usually affecting the thoracic spine, this type of scoliosis appears in youngsters between the ages of 10 and 15 after their first growth spurt. Later in life, different muscle or connective tissue disorders may potentially be the cause.
Dextroscoliosis symptoms include unequal shoulder height, asymmetrical shoulder blade or rib prominence, uneven hips or waistline, and visible spine curvature. In situations that are more severe, the patient may tilt their head or tilt their entire body to one side due to the abnormal curvature. Dextroscoliosis can compress the organs, causing respiratory and circulation issues, depending on the degree of curvature. In addition, it could hurt in the back, legs, or chest.
Unfortunately, the idiopathic scoliosis accounts for up to 85% of cases, meaning there is no identified the cause. In the remaining 15–25% of cases of dextroscoliosis, the problem is either congenital, neuromuscular, or age-related. Though it can affect anyone, preteen and teenage girls are the ones who experience it most frequently.
2.Dextroconvex Scoliosis
The lumbar area of the spine has an S-shaped curvature, which is characteristic of dextroconvex scoliosis. Lumbar dextroscoliosis or dextroscoliosis of the lumbar spine are other names for this type of scoliosis. A slight curve, roughly between 10 and 20 degrees, is frequently referred to as mild dextroscoliosis. The term describes the degree of spinal curvature; it has nothing to do with the severity of symptoms brought on by the curvature.
3.Thoracic Dextroscoliosis
The thoracic area of the spine has an abnormal curvature, bending laterally to the right, which is the hallmark of thoracic dextroscoliosis. Mild thoracic dextroscoliosis is usually defined as a curvature of 20 degrees or less on the Cobb angle measuring scale, same like mild lumbar dextroscoliosis. Even in cases when this type of scoliosis is modest, pain and other symptoms may still be present. Additionally, the curve might develop with time.
4.Levoscoliosis
Levoscoliosis, which is the opposite of dextroscoliosis, is defined by an abnormal levocurvature, or lateral curvature, of the spine that extends to the left. Although this type of scoliosis usually affects the lumbar spine, it can also occasionally affect the thoracic spine.
When the thoracic spine is affected, the organs may be compressed, which may result in heart and lung issues. Levoscoliosis can cause breathing difficulties and shoulder and hip asymmetry in more severe cases, but in milder situations, it may not cause any symptoms and may even go away on its own. It’s not usually a painful condition.
Levoscoliosis has no known origin, although it is frequently a congenital scoliosis, a disorder that is present from birth. It can also develop as a result of muscle and tissue disorders such as muscular dystrophy.
When a tumor grows on the spinal cord, levoscoliosis in the thoracic spine is frequently a clear indicator. X-rays can be used for diagnosis, and MRI and CT scans can be used to assess the condition’s severity and effect on internal organs.
5.Levoconvex Scoliosis
Thoracic levoscoliosis, or levoconvex scoliosis, is a type of scoliosis that affects the thoracic portion of the spine. It is identified by an abnormal lateral curve that points to the left.
Levoconvex scoliosis can range in severity from mild to severe, just like other types of scoliosis, however, the curvature is typically limited to the T1 through T12 vertebrae. However, this type of scoliosis may affect the rib cage and possibly compress internal organs, which can be harmful. It’s essential to keep an eye out for any possible signs of levoconvex scoliosis advancement.
6.Lumbar Levoscoliosis
Lumbar levoscoliosis, the opposite of lumbar dextroscoliosis, is defined by an S-shaped curvature of the spine in the lumbar area. The curve itself turns to the left and impacts the lower back’s L1 through L5 vertebrae. Similar to dextroscoliosis, lumbar levoscoliosis is typically modest at first but can worsen over time, especially if it first appears in childhood or early adolescence.
Symptoms of Scoliosis
Scoliosis rarely shows symptoms in its early stages, and each person’s degree of the condition might differ significantly. While some people’s spinal curvatures are rather small, others have significantly greater curvatures.
Scoliosis is defined as a sideways curve of at least 10 degrees. When the person wears clothing, a 10- to 20-degree curve might not be seen. When a person’s body tilts to one side or their clothes hangs unevenly, viewers may perceive a curvature that progresses to 20 degrees or more.
Typical scoliosis symptoms include:
- One shoulder blade could stick out more than the other due to uneven shoulder blades.
- uneven hips, waist, or rib cage.
- Spine that appears asymmetrical.
- Leaned to one side.
- The head is positioned off-center from the pelvis.
- Hip misalignment resulting in altered gait.
- Breathing difficulties (particularly common in cases with severe neuromuscular or congenital scoliosis).
- More severe episodes of muscle spasms or back pain due to imbalances in the trunk.
- Reduced range of motion: Scoliosis can cause the spine to twist, which can make it more inflexible and less flexible.
- Lower self-esteem is a symptom that often goes unnoticed, but it can be very important for people with obvious spinal deformities, particularly teenagers. Wearing a conspicuous back brace can be quite uncomfortable and embarrassing, especially at school.
Epidemiology
There are five to nine million cases of scoliosis in the US, which represents 2-3% of the population. 1.5–3% of people have a scoliosis (spinal column curve) of 10° or less. The age of onset among children and adolescents, who account for up to 85% of those diagnosed, is typically between 10 and 15 years old (but it can happen earlier). This results from fast growth spurts that occur throughout puberty, a time when environmental and genetic factors have the most effect on spinal development.
Scoliosis is more common in female teenagers because growth spurts occur before to postural musculoskeletal maturation. Scoliosis is still a common condition that affects otherwise healthy youngsters, even though the number of cases has decreased since Cobb angle analysis was used for diagnosis. Even though scoliosis is a deformity of the spine, studies have indicated that it affects children’s pneumonic function, standing balance, and stride execution.
Numerous studies have been conducted on how wearing a backpack affects these three adverse consequences. Idiopathic scoliosis (IS) is less common after adolescence when skeletal maturity is reached; however, because of vertebral osteoporosis and weakening muscles, further curvature may develop in late age.
Diagnosis
A physical examination, x-ray, spinal radiograph, CT scan, or MRI are typically used to confirm scoliosis. The curve’s degree of severity is indicated by the number of degrees, which is measured using the Cobb Method. A posterior-anterior radiograph with a coronal curvature of greater than 10 degrees can be used to prove a positive diagnosis of scoliosis. When a curve has an angle greater than 25 to 30 degrees, it is frequently considered important. An angle between 45 to 50 degrees is considered a severe curvature, and patients are often referred for more treatment.
The Adam’s Forward Bend Test is a common examination that pediatricians and screening officers in elementary schools occasionally use. During the examination, the patient leans forward and puts both feet together while bending 90 degrees at the waist. From this angle, examiners can quickly spot any irregular spinal curvatures or trunk asymmetry. Although the first screening test is basic, it can indicate possible problems but not the specific type or severity of the condition. An accurate and conclusive diagnosis needs radiographic testing.
X-ray: Radiation can be used to generate a picture of a body part, revealing the structure of the vertebrae and joint locations. Spine X-rays are taken in order to look for additional possible sources of pain, such as infections, fractures, or deformities.
Computed tomography scan (also known as a CAT or CT scan): A diagnostic image that is produced by a computer reading X-rays and that shows the shape, size, and contents of the spinal canal together with its surrounding structures. exceptional at imagining skeletal structures.
Magnetic resonance imaging (MRI): A diagnostic process that creates three-dimensional pictures of human parts using powerful magnets and computer technology. The images shown can show tumors, anomalies, the spinal cord, surrounding tissues, and nerve roots.
In children
Children with scoliosis can be divided into three age groups: infantile (0 to 3 years), juvenile (3 to 10 years), and adolescent (age 11 and older, or from the start of puberty until skeletal maturity). Idiopathic scoliosis accounts for the majority of cases that develop during adolescence. Depending on the child’s age and the severity of their scoliosis, treatment options include bracing, surgery, and/or close supervision.
There is a reported higher prevalence of additional congenital abnormalities in children with congenital scoliosis. The organs most frequently linked to these are the spinal cord (20%), the heart (10–15%), and the genitourinary system (20–33%). When congenital scoliosis is detected, it is essential to evaluate the neurological, genitourinary, and cardiovascular systems.
In adults
Adult-onset scoliosis differs from childhood scoliosis in that patients with adult-onset scoliosis have different treatment aims and underlying causes because they have already reached skeletal maturity. The three groups that follow represent the majority of adults with scoliosis: 1. People in their adult years who suffer from degenerative scoliosis. 2.. Adults with scoliosis who have undergone surgery as adolescents. 3. adults who were not treated while they were younger.
About 40% of adult scoliosis patients saw a progression throughout the course of a 20-year study. Of those, 30 percent had very minor progression, often less than one degree each year, and 10 percent had extremely considerable progression.
Degenerative scoliosis is more common among individuals 65 years of age and older. It usually affects the lumbar spine or lower back. Spinal stenosis, or the narrowing of the spinal canal, frequently occurs with it, pinching the spinal nerves and impairing their ability to function correctly. Pain in the back associated with degenerative scoliosis usually begins gradually and is activity-related. Because the curvature of the spine in this type of scoliosis is frequently quite mild, surgery may only be recommended in cases when non-operative measures are unable to relieve the condition’s associated pain.
Treatment of Scoliosis
The majority of scoliosis cases in children and adolescents are mild and don’t require treatment. When a patient has a curve between 10 and 25 degrees, a doctor will typically see them every three, six, or twelve months to see if their condition is changing.
A physician might suggest bracing for a curvature between 25 and 40 degrees. A physician might advise surgery if the curve is larger than this and the skeleton is still developing.
The factors that follow will be taken into consideration by the physician when selecting a course of treatment:
Gender: Scoliosis that progressively worsens is more common in women than in men.
Severity of the curve: The curve’s kind and severity may have an impact on how it develops.People with idiopathic scoliosis typically have S-shaped curves, while people with neuromuscular scoliosis are more likely to have C-shaped curves.
Position of curve: A curve in the middle of the spine is more prone to worsening than one in the upper or lower half.
Bone maturity: If a person’s bones have finished developing, there is a decreased chance of things getting worse. while the bones are still growing, braces work better.
Various treatments for scoliosis include:
1. Observation
The spinal curvature in a large number of children with scoliosis is so modest that treatment is not warranted. Throughout adolescence, the doctor may want to check on the child every four to six months if they have concerns that the curve may be rising.
X-rays are often advised for adults with scoliosis once every five years unless their symptoms are becoming worse.
2. Casting
Plaster casting is a better option to bracing that a doctor may use to assist a newborn with infantile scoliosis develop into a normal posture for their spine. The baby will always be wearing the cast, which is attached to the outside of their body. Since most babies develop quickly, the doctor will need to replace the cast on a frequent basis.
3. Bracing
Bracing is typically used to maintain curvature and stop it from getting worse to the point where surgery is necessary. It is typically done on those who still have bone growth. Bracing has been shown in some situations to considerably reduce curves in adolescent patients; in one example, the curve out of the brace decreased from 40° to 18°.
Adult patients may occasionally be administered braces to alleviate scoliosis-related pain. Fitting someone with a brace involves covering their torso and, in certain situations, their neck (the Milwaukee Brace, for example).
The most frequently used type of brace is a Thoracolumbosacral orthosis (TLSO), or Boston brace, which is a custom-built corset-like appliance made of plastic or fiberglass that fits from the armpits to the hips. Wearing it for 22–23 hours a day is often advised since it puts pressure on the spine’s curvature. In addition to the design of the brace and the ability of the orthotist, other factors that affect its effectiveness include the wearer’s compliance and daily wear quantity.
An alternate type of brace is a nocturnal-only brace, which overcorrects the deformity and is only worn at night while the child sleeps. Even if nocturnal braces are more convenient for kids and families, it’s unclear if they work as well as traditional braces.
Indications for Bracing:
Individuals who present with Cobb angles less than 20° and are still growing should be properly watched. When bracing growing individuals with Cobb angles between 20 and 29°, the risk of advancement should be taken into account. This includes taking age, Cobb angle rises during a six-month period, Risser sign, and clinical presentation into account. Individuals who show Cobb angles greater than 30° while still growing should wear braces. But keep in mind that these are only recommendations, and not everyone will fit in this table.
4. Medications
The symptoms of scoliosis can be treated with a variety of over-the-counter and prescription drug kinds.
Acetaminophen and NSAIDs are commonly available over-the-counter drugs. Since acetaminophen is an analgesic, it reduces pain but does not also reduce inflammation. NSAIDs, which are available over-the-counter in both brand-name and generic formulations, are useful for both pain relief and inflammation reduction.
For the purpose of to reduce muscular spasms and improving range of motion, muscle relaxants are best used when combined with physical therapy or a regular exercise and stretching program. Tizanidine, Baclofen, Robaxin, Soma, and Flexeril are examples of common muscle relaxants.
Another class of drugs that are frequently used to treat scoliosis-related numbness, tingling, shooting, stabbing, or radiating pain is nerve membrane stabilizers. Nerve membrane stabilizers such as gabapentin (Neurontin) and Lyrica (Pregabalin) are often prescribed medications that decrease the number of pain signals that are generated by nerves.
5. Epidural Steroid Injections
By injecting steroid or anti-inflammatory medicine at a particular level or levels in the spine, epidural steroid injections help patients feel less pain. When a nerve is compressed by a herniation, the nerve and surrounding tissue become inflamed, which results in discomfort. Medication is administered to the right location, as close to the spinal nerves as feasible, and past the back muscles, using a specialist needle.
Since steroids naturally reduce inflammation, they can decrease the pain caused by disc herniation by reducing the inflammation surrounding the nerve. Up to many months of pain reduction can be obtained via steroid injections, which may give superior pain relief for radiating symptoms like leg pain compared to back pain treatments alone.
6. Chiropractic Treatment
Chiropractic treatment may be taken into consideration to help improve flexibility and reduce pain. Although this type of treatment can help with pain sensations, it won’t cure scoliosis.
Though evidence is limited, an older study found that persons with scoliosis experienced improvements in pain and other symptoms both immediately after chiropractic treatment and 24 months later.
It is essential to choose a chiropractor who specializes in treating scoliosis. It is possible for non-specialists to worsen the illness.
7. Diet and Vitamin Supplementation
Numerous investigations have demonstrated that teenagers with idiopathic scoliosis have reduced vitamin D levels compared to the overall population. Although the jury is still out on whether vitamin D supplements are beneficial or not, they can’t hurt. Apart from consuming supplements, you can get vitamin D by:
- Tuna
- Sardines
- Mushrooms
- Oysters
- Sun exposure
- Egg yolks
- Shrimp
8. Counseling
You could be referred to a counselor by a doctor. When medical treatments aren’t effectively controlling chronic pain, counseling may be useful.
Cognitive behavioral therapy (CBT) is one kind of counseling. While CBT won’t make the pain go away, it can assist you in developing ways to cope.
You can discuss how you handle your pain with a CBT counselor. Your counselor can also assist you in learning ways to manage pain.
Physical therapy exercises
Pelvic Tilts.

Postural awareness, alignment, and engagement are the main goals of a pelvic tilt. Additionally, it works the transverse abdominal muscles, which support stability in the core.
To perform a pelvic tilt, you should:
- With their knees bent and their feet flat on the ground, they should lie on their back.
- Flatten their back toward the ground and contract their stomach muscles.
Breathe normally for five seconds while holding. - Release
- Perform two sets of ten.
Arms and legs raise

With arm and leg raises, one can strengthen their lower back. To avoid putting too much torque on the spine, a person might need to start with just their arms or legs.
To perform the raises, an individual should:
1. They should lie face down with their foreheads towards the floor. Placing their hands on the ground, they should extend their arms straight over their heads. Make sure both of your legs are straight.
2. Lift their legs and arms off the floor.
3. After taking a deep breath, raise their arms and legs again.
4. 15 repetitions is the goal.
Cat-Cow
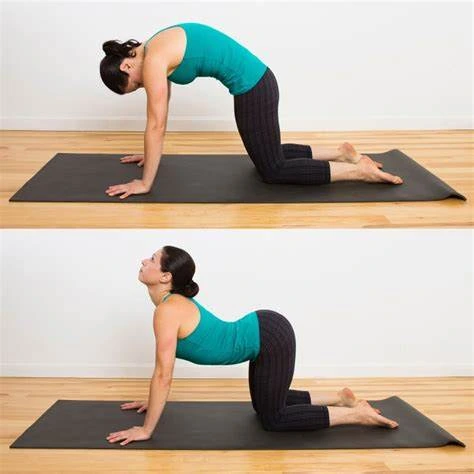
A common yoga pose that helps maintain a supple and pain-free spine is the cat-cow. Additionally, it helps spine mobility.
To perform the Cat-Cow position, people should:
1. As they start out on their hands and knees, make sure their head and neck are comfortable and their back is level.
2. Take a deep breath and arch your back by contracting your abdominal muscles.
3. Release the muscles in their abdomen, lower their back, allow their tummy to drop, and raise their head toward the sky as they exhale.
4. Perform two sets of ten.
Latissimus dorsi stretch
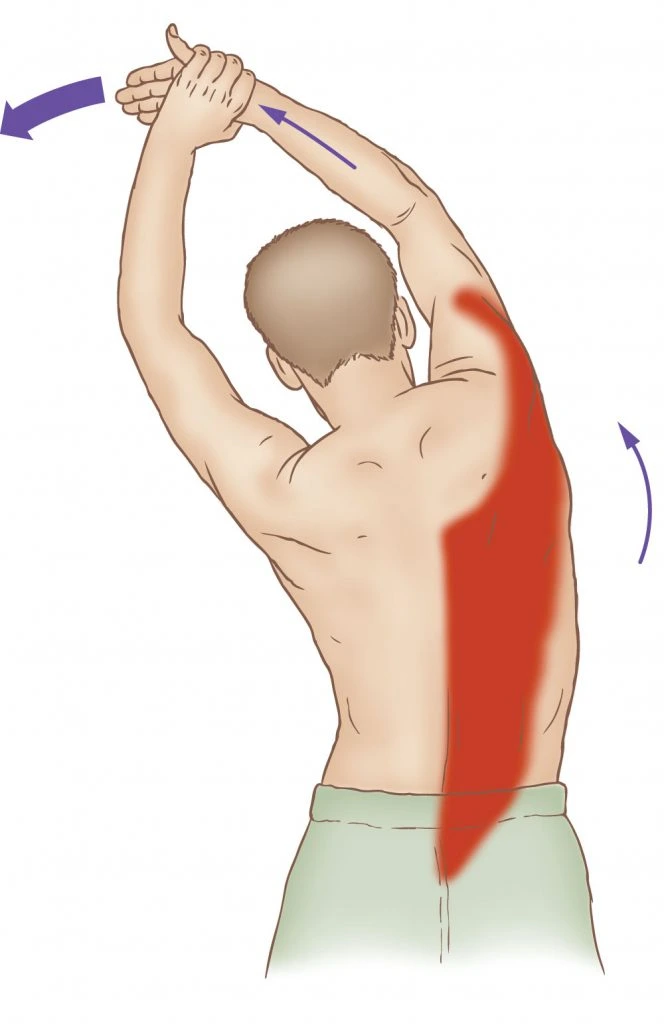
The latissimus dorsi, a large, flat muscle that covers the majority of the lower thoracic cavity in the back, is the target of this stretch. Its primary purpose is to move the upper limbs.
These muscles are directly affected by thoracic scoliosis. The latissimus dorsi can become tight as a result of lumbar scoliosis.
To perform a stretch of the latissimus dorsi, one should:
1. Maintain good posture while standing in a neutral position.
2. Keep their knees slightly bent and their feet shoulder-width apart.
3. Grasp their right wrist with your left hand while extending your arm over them.
4. They should flex slightly to the right until their left side starts to feel stretched.
Abdominal press

Strong abdominal muscles may reduce strain on the back muscles while supporting good posture. Activating the muscles of the transverse abdomen might also be beneficial.
When performing an abdominal press, people should:
They should be lying on their back with their knees bent and their feet flat on the floor.
Maintain a neutral, tension-free back posture.
When their knees are over their hips and their thighs and feet are at a 90-degree angle, raise both of their feet off the ground.
With their hands, push their knees out of the way, then use their abdominal muscles to pull their knees toward their hands.
As this is a static exercise, pressing should be done with the arms and legs still.
Take three deep breaths and then relax.
Perform two sets of ten.
Bird-dog

Another yoga-inspired exercise is the bird-dog.
To perform this exercise, people should:
1. Start with their back straight and on their hands and knees.
2. Put their knees under their hips and their hands directly under their shoulders.
3. Stretch one arm straight out in front of you and the other leg straight back.
4. Breathe normally for five seconds, then hold it.
5. With the opposite arm and leg, repeat.
6. Perform 10-15 reps for each side.
Upward Dog

For performing this exercise,
1. Begin on your hands and knees, ensuring that your elbows and shoulders are aligned.
2. The next thing you’ll want to do is lower your hips and shoulders at the same time. Make sure you look up at the ceiling and expand your chest outward throughout this period.
3. After completing the exercise, raise your thighs off the floor and take a deep breath. Ensure that you repeat this exercise as necessary depending on your comfort level.
4. The lower back muscles, which are crucial in stabilizing the lumbar spine, are stretched out during upward dog.
Downward Dog

For performing this exercise,
1. Starting from the hands and knees position, make sure your elbows are in alignment with your shoulders.
2. Next, move your chest closer to your legs and raise your hips toward the ceiling and back without locking your arms. During this stage, make careful to raise your coccyx to maintain spinal alignment.
Your toes should point toward your head while your feet are aligned with your hips.
3. Now that you are in this position, take a few deep breaths and then release.
Surgical Treatment
The main two goals of surgery in children are to reduce their spinal deformity and to prevent the curve from getting worse as they get older. Only in cases where there are indications of advancement and a spinal curve more than 40 degrees would the majority of specialists advise surgery. Depending on the specific situation, either an anterior approach—through the front—or a posterior approach—through the back—can be used for this procedure.
Revision surgery may be necessary for some individuals who received treatment as children; this is especially true if the treatment was received 20 to 30 years ago before significant advancements in spine surgery methods were made.
A lengthy spinal segment would often be fused back then, the remaining movable segments of the spine bear a far greater load and stress during movement when numerous vertebral segments of the spine are fused together. Degenerative changes in the mobile segments above and below the spinal fusion over time are known as adjacent segment disease. This may lead to painful ligament, facet joint, and disc arthritis.
The majority of persons with spinal curves more than 50 degrees, leg nerve injury, and/or problems related to the bladder or intestines may benefit from surgery. Adults who have spinal stenosis and degenerative scoliosis may need to have spinal fusion during decompression surgery, which involves both front and back surgical approaches.
When it comes to surgery, there are several factors that can raise the risks for older persons with degenerative scoliosis. Advanced age, smoking, being overweight, and the existence of additional health issues are some examples of these factors. For elderly persons with scoliosis, longer recovery times are often expected following surgery.
Posterior approach: For adolescents with idiopathic scoliosis, posterior spinal fusion with instrumentation and bone grafting is the most common surgical procedure. The patient is positioned on the person’s stomach, with the back open. Spinal fusion occurs after the spine is straightened using stiff rods during this procedure. In spinal fusion, the curved part of the spine receives a bone graft to firmly fuse two or more vertebrae together.
When it comes to young children, this treatment often takes several hours; however, older people will typically require more time. Thanks to recent technological advancements, the majority of patients with idiopathic scoliosis are discharged from the hospital a week after surgery and don’t need braces afterward. After surgery, the majority of patients are back to work or school in two to four weeks, and they can resume their pre-surgical activities in between 4 and 6 months.
Anterior approach: During the procedure, the patient rests on his or her side. To access the spine, the surgeon makes incisions in the patient’s side, deflates the lung, and removes a rib. Compared to an open operation, video-assisted thoracoscopic (VAT) surgery is less invasive and provides improved spine visibility. Better deformity repair, speedier patient rehabilitation, enhanced spine mobilization, and fusion of fewer segments are some potential benefits of the anterior spinal approach. There are two potential disadvantages to this procedure: the risk of morbidity is higher with this approach, though VAT has helped to lower it, and many patients need bracing for several months after surgery.
Decompressive laminectomy: For the purpose of providing more space for the nerves, the laminae (roof) of the vertebrae are removed. When both spinal stenosis and scoliosis are present, a spinal fusion—either with or without spinal instrumentation—is frequently advised. A variety of tools, like as rods or screws, can be used to strengthen the fusion and provide support for the spine’s unstable regions.
Minimally invasive surgery (MIS): Fusion can be done with smaller incisions using MIS. The accuracy of hardware placement and incisions has increased with the use of endoscopes (camera technology) and advanced fluoroscopy (X-ray imaging during surgery), reducing tissue stress and facilitating a MIS approach. It is essential to remember that not every case can be handled in this way, and the surgical approach chosen depends on a variety of factors.
Complications of Scoliosis
If you don’t get treatment for scoliosis, the curvature of your spine may get worse and cause long-term problems that will negatively impact your overall health. Possible complications of scoliosis include:
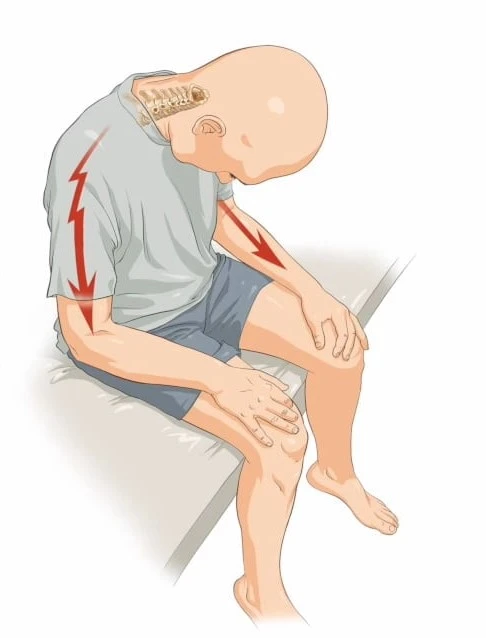
Nerve Compression
It’s possible for the spine to put pressure on neighboring nerves when its vertebrae have abnormal curvatures. There may be problems from this compression of the nerve. Usually, tingling and numbness are signs of a nerve problem. This may cause tingling and numbness to travel down the legs. Pain in the back is another possible problem for patients. In severe cases, spinal nerve compression can cause loss of control of the bowels or bladder. Nerve compression can occasionally cause erectile dysfunction in men.
Psychological Complications
A person with mild scoliosis may not experience many problems in their day-to-day activities. Scoliosis, however, can sometimes result in noticeable anatomical abnormalities. One hip and shoulder may be higher than the joints on the other side, which the patient may sense. Items of clothing could hang unevenly. The patient may have to give up some activities if a back brace is required. Scoliosis can cause emotional issues such as low self-esteem and excessive self-consciousness, especially in young people. A patient support group could be beneficial if scoliosis is causing psychological issues for you or your kid.
Reduced flexibility.
As scoliosis becomes more severe, it can restrict the spine’s flexibility and range of motion, making it difficult to carry out specific exercises and affecting balance and posture.
Impaired lung function.
Breathing problems and dyspnea may arise from severe scoliosis, which limits lung function and prevents the lungs from fully extending.
Lumbar stenosis
Scoliosis is linked to lumbar stenosis, although regardless of age, it is unlikely to result in any serious neurological issues. The narrowing of the spinal canal known as lumbar stenosis might eventually result in weakness, pain in the legs, or problems affecting the nerves.
Back pain
Back pain and discomfort can be brought on by strain on the joints, ligaments, and discs surrounding the spinal structures as well as muscular imbalances caused by abnormal spine curvature.
Heart problems
When a person has severe scoliosis, their rib cage is severely affected by the curvature, which can put a strain on the heart and raise the risk of cardiac disorders such as mitral valve prolapse.
Differential diagnosis
Malformation comes to mind osteogenesis imperfecta, congenital hemivertebra, Marfan syndrome, and arthrogryposis. It may also indicate a short leg syndrome.
Inflammation may indicate fungal disease of the spine or Tuberculosis. I should also bring out idiopathic scoliosis, which accounts for 80% of cases.
Neurologic conditions such as Friedreich ataxia, poliomyelitis, syringomyelia, and muscular dystrophy can result in scoliosis.
Trauma should make it easier to remember thoracolumbar sprains, fractures, compressions, and herniated discs. It needs to bring to mind thoracoplasty as well as other surgical causes.
Systemic diseases such as Paget disease, pulmonary fibrosis, and Ehlers-Danlos Syndrome are connected with Scoliosis
Prognosis
The degree of spinal deformity can have an important effect on the prognosis of scoliosis. Since it is difficult to predict how the child’s spine will develop as they get older, the projected deformity cannot be determined with precision at the time of the initial diagnosis in childhood.
However, certain suggestive variables can help in speculating about the individual’s conditional outlook. Anomalies of the thoracic spine and several totally segmented hemivertebrae tend to advance more quickly.
Most of the growth in the spine happens in the first five years of life and during the growth spurt in adolescents right before puberty. As a result, these two intervals are the most crucial ones, and children with scoliosis in these age ranges should have regular monitoring of their spinal development. The prognosis usually improves with therapies designed to minimize curvature and promote healthy spine growth.
Mild Scoliosis
Mild scoliosis is defined as a curve that is less than 20 degrees. The majority of people with this kind of illness have an acceptable prognosis and don’t need any special treatment.
Instead, to keep the severity from getting worse, these patients should be watched for indications that their disease is getting worse, especially as the kids get older.
Moderate scoliosis.
A moderate case of scoliosis is defined as a curve that ranges from 25 to 70 degrees. Strong conclusions about the results or following health complications of this group of individuals with the illness have not been formed by current research.
As such, the usefulness of surgical intervention is unclear, and suggestions are typically given based on individual cases.
Severe scoliosis
Severe scoliosis is defined as a curve of greater than 70 degrees. This frequently results in the ribs pressing against the lungs, which restricts breathing and eventually causes hypoxia. The functioning of the body’s other organs may be affected by the lower blood oxygen levels. Furthermore, there is a chance that the spinal curvature will result in harmful structural alterations to the heart.
Intervention is frequently advised for people with severe scoliosis for the purpose of encouraging good spine growth.
Very severe scoliosis
Very severe scoliosis is defined as a curvature larger than 100 degrees. Because of the modifications to the structural space in the chest, this frequently has an adverse effect on the heart as well as the lungs. Pneumonia and lung infections are more common in people with this severe type of scoliosis.
Although this degree of malformation is uncommon in modern nations, when compared to other severities, it is linked to noticeably higher death rates.
Prevention
Scoliosis cannot be prevented. So disregard any myths you may have heard about scoliosis being caused by sports injuries suffered as a child.
Similarly, you would worry about your children’s textbook weight if they are in school. Although they might result in neck, shoulder, and back pain, heavy backpacks don’t induce scoliosis.
What about bad posture, too? The incidence of scoliosis is unaffected by an individual’s posture when standing or sitting. However, a visible lean may result from a curved spine. Ask your doctor to examine your child’s spine if they are unable to stand up straight.
When should I visit a healthcare professional?
Contact a healthcare professional if:
- You think you may have scoliosis symptoms or signs.
- It doesn’t seem like your treatment is helping.
- You experience worsening symptoms.
It’s essential for parents or other caregivers to get in touch with a pediatrician if:
- Regular screening indicates that your child might have scoliosis.
- Your youngster shows scoliosis indications and symptoms.
- Your child’s symptoms are not getting better despite treatment.
- Because scoliosis runs in your biological family, you want to monitor your child’s growth.
Conclusion
If your child brings a note home from school stating that a screening revealed probable scoliosis, you should be concerned. Alternatively, perhaps you went to see your doctor and they noted that you had bone degeneration that is affecting your height and posture.
Treatment isn’t usually necessary for scoliosis because the majority of cases are minor. Often, all you need is a brace or other nonsurgical treatment. Surgery is a safe and effective treatment option for severe curvature, though. After diagnosing you or your kid with scoliosis, your provider will advise you on how to take care of yourself and your child and let you know if they suggest treatment.
FAQ
What is the main cause of scoliosis?
Idiopathic scoliosis is the term for the condition in which the cause of scoliosis is unclear in over 80% of cases. In other cases, scoliosis may arise from a congenital disorder that typically runs in families, arthritis, osteoporosis, or degeneration of the spinal discs.
How do you sleep with scoliosis?
The entire spine remains extended while sleeping on the back as opposed to bent or twisted. This neutral posture decreases pain and the scoliotic curve’s progression. For optimum comfort and pressure relief, it’s crucial to have a mattress that supports this position.
Is scoliosis is permanent?
After receiving treatment, individuals with scoliosis can lead active, fulfilling lives. People’s spines often stop curving after they reach adulthood as long as they receive the proper care when they’re still children or teenagers.
Can exercise help scoliosis?
The recommendation for exercise as a treatment for mild to moderate scoliosis is rising. You might be able to reduce the pain you experience from your scoliosis and delay the curvature of your spine by being proactive and doing these exercises.
Is scoliosis 100% curable?
Scoliosis cannot be cured because it is a progressive structural spinal disorder, however it is very treatable. The optimal course of treatment is one that preserves the general health and function of the spine while focusing on conservative chiropractic care.
What organs are affected by scoliosis?
A person with scoliosis may experience symptoms in various organs, such as the heart, brain, lungs, muscles, neurological system, reproductive system, and mental health.
References
- Professional, C. C. M. (n.d.). Scoliosis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15837-scoliosis
- Spinal Anatomy Overview – Scoliosis and Spine Associates. (2018, July 10). Scoliosis and Spine Associates. https://www.scoliosisassociates.com/anatomy-diagnosis-2/spinal-anatomy-overview/
- Scoliosis. (2023, July 27). Yale Medicine. https://www.yalemedicine.org/conditions/scoliosis
- Scoliosis. (n.d.). Physiopedia. https://www.physio-pedia.com/Scoliosis
- Novakovic, A. (2023, April 24). Everything you need to know about scoliosis. https://www.medicalnewstoday.com/articles/190940#causes
- Common Risk Factors for Scoliosis: John Regan, MD: Orthopedic Spine Surgeon. (n.d.). https://www.spinegroupbeverlyhills.com/blog/common-risk-factors-for-scoliosis
- Surgery, C. F. M. I. (2021, March 9). 3 Risk Factors For Scoliosis In Teenagers And How To Decrease Back Pain – The Center for Minimally Invasive Surgery. The Center for Minimally Invasive Surgery. https://cmisurgery.net/orthopedic/3-risk-factors-for-scoliosis-in-teenagers-and-how-to-decrease-back-pain/
- Scoliosis. (2024, March 29). Wikipedia. https://en.wikipedia.org/wiki/Scoliosis#Epidemiology
- Scoliosis Symptoms Types & Treatments | Center for Comprehensive Spine Care. (2023, December 18). Center for Comprehensive Spine Care. https://comprehensivespine.weillcornell.org/conditions-we-treat/scoliosis/scoliosis-symptoms-types-and-treatments/
- Scoliosis – Symptoms, Diagnosis and Treatment. (n.d.). https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Scoliosis
- Novakovic, A. (2023, April 24). Everything you need to know about scoliosis. https://www.medicalnewstoday.com/articles/190940#treatment
- Scoliosis Treatment: Best 5 Non-Surgical Options. (2021, April 30). The Spine Center. https://www.chicagospine.net/news/non-surgical-scoliosis-treatment/
- Scoliosis Treatment – Preferred Surgicenter – Chicago’s Spine & Orthopedic Experts. (2018, June 6). Preferred Surgicenter – Chicago’s Spine & Orthopedic Experts. https://preferredsc.com/spine/disease/scoliosis/treatment/
- What Kind of Pain Does Scoliosis Cause? (2020, December 23). Healthline. https://www.healthline.com/health/scoliosis-pain#treatment
- Ames, H. (2024, March 1). The 7 best stretches and exercises for scoliosis. https://www.medicalnewstoday.com/articles/325385
- 12 Scoliosis Exercises for Pain Relief | Jason Lowenstein, MD. (n.d.). Dr. Jason Lowenstein | Scoliosis & Spinal Deformities Surgeon. https://jasonlowensteinmd.com/12-scoliosis-exercises-for-pain-relief/
- Chavda, V. (2023, April 14). A Look at Potential Complications of Scoliosis. Spine Institute of Nevada. https://www.spineinstituteofnevada.com/blog/a-look-at-potential-complications-of-scoliosis/
- E. (2024, March 31). Scoliosis Complications Later in Life | Scoliosis SOS. Scoliosis SOS. https://www.scoliosissos.com/blog/scoliosis-complications-later-in-life
- Curtis, L. (2023, August 22). What Are the Symptoms of Scoliosis? Verywell Health. https://www.verywellhealth.com/scoliosis-symptoms-7554444
- Scoliosis – Differential Diagnosis in Primary Care, 4th Edition. (n.d.). https://doctorlib.info/medical/diagnosis-primary-care/221.html
- Scoliosis Prognosis. (2022, December 23). News-Medical. https://www.news-medical.net/health/Scoliosis-Prognosis.aspx
- Scoliosis. (2017, January 24). WebMD. https://www.webmd.com/back-pain/causes-scoliosis
- Orthotics, L. (n.d.). Juvenile Scoliosis. https://www.londonorthotics.co.uk. https://www.londonorthotics.co.uk/scoliosis/types-of-scoliosis/juvenile/
- Nalda, T. (2024, March 27). The Different Types of Scoliosis – What Makes Them Unique? Scoliosis Reduction Center. https://www.scoliosisreductioncenter.com/blog/scoliosis-types
- Infantile Scoliosis | Boston Children’s Hospital. (n.d.). https://www.childrenshospital.org/conditions/infantile-scoliosis#:~:text=What%20is%20infantile%20scoliosis%3F,a%20type%20of%20idiopathic%20scoliosis
- Scoliosis Types & More – FREE MRI Review. (2018, June 6). Preferred Surgicenter – Chicago’s Spine & Orthopedic Experts. https://preferredsc.com/spine/disease/scoliosis/types/
- Stitzel, C. (2023, November 28). 7 Types of Scoliosis & Their Differences. Treating Scoliosis. https://treatingscoliosis.com/blog/scoliosis-types-differences/





9 Comments