Sacral Plexus Injury
The sacral plexus is a collection of nerves in the lower back that are near the sacrum. It controls the sensation and movement of the legs, feet, and buttocks. A sacral plexus injury is the result of damage to these nerves.
Sacral nerve pain can be caused by physical trauma, especially if the sacral nerve roots are damaged. A few signs of this damage include lower back pain, side and rear leg pain, and sensory abnormalities affecting the buttocks and groin.
The source and extent of sacral plexus damage determine how it should be treated. Sometimes the nerves heal on their own and no medical intervention is required. In certain situations, surgery could be required to restore injured nerves.
Enhancing the function and strength of the injured muscles is another benefit of physical therapy. Depending on the injury’s severity, there are different outcomes for sacral plexus injuries. While some people heal completely, others could experience long-term nerve damage.
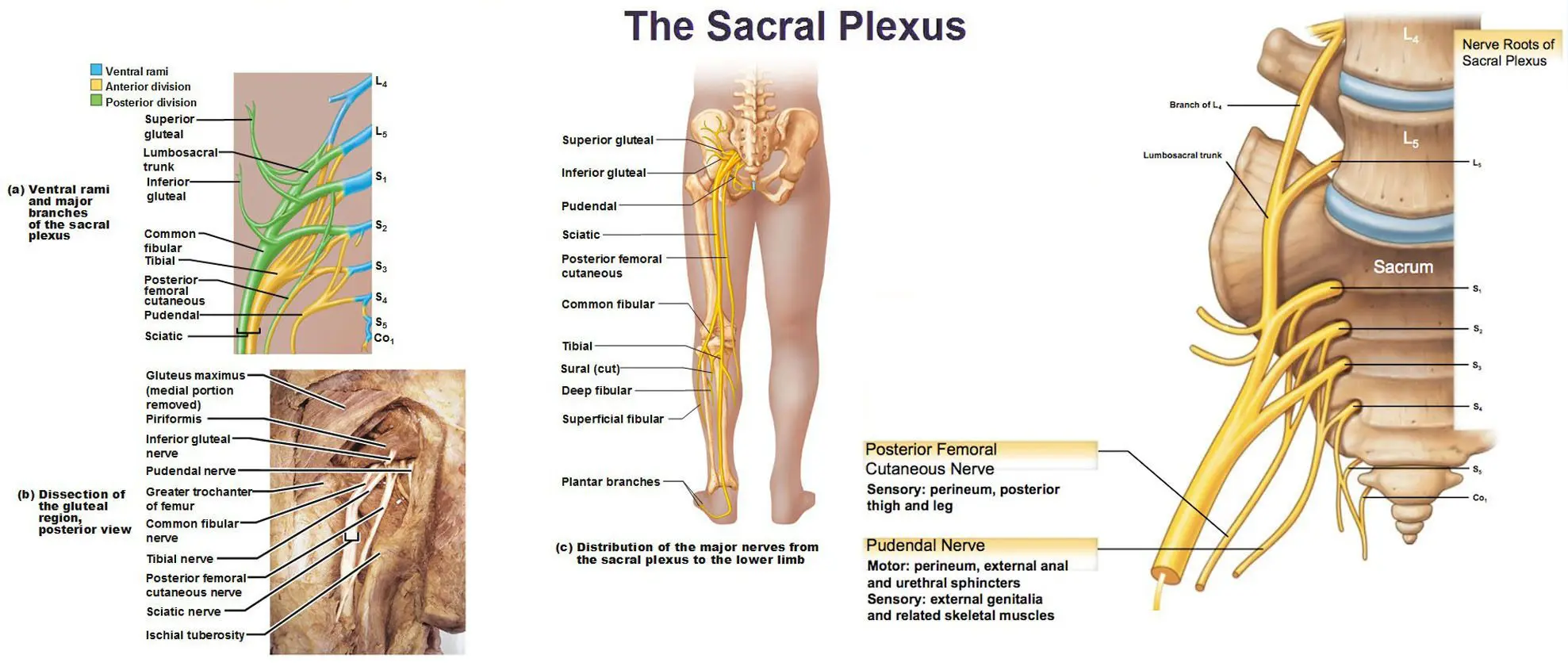
Sacral Plexus: Anatomy and its Function
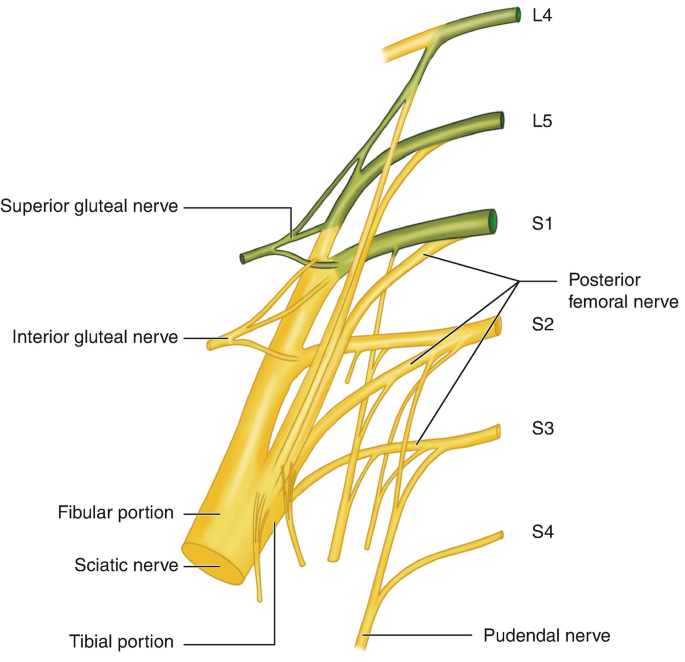
The sacral plexus is a network of nerves made up of the ventral rami (front branches) of the upper sacral spinal nerves (S1, S2, S3, and occasionally S4) and the lower lumbar spinal neurons (L4 and L5). It is essentially a group of nerve fibers that come together to service various lower body parts.
Location: The sacral plexus is situated anterior to the piriformis muscle on the posterior pelvic wall. It lies tucked away near the sacrum, the triangle-shaped bone at the base of the spine, deep within the pelvis.
Function: The sacral plexus is essential for lower body movement and feeling. Serving as a pathway for information, it transmits commands to regulate muscles and receives sensory data related to touch, pain, and temperature from the brain and spinal cord.
Motor Function: The following areas get motor innervation from the sacral plexus:
- The gluteus maximus, medius, and minimus are the buttock muscles.
- Muscles on the back of the thigh called hamstrings
- Muscles of the lower leg (gastrocnemius, soleus, etc.)
- Muscles in the feet (dorsiflexors, plantar flexors, etc.)
Sensory Function: Additionally, the sacral plexus innervates the following sensory areas:
The skin of the lower leg, foot, buttocks, hip, knee, ankle, and foot joints.
Branches of the Sacral Plexus: The sacral plexus splits into several branches, each of which has a distinct purpose.
- The gluteus maximus muscle: which aids in hip extension by straightening the leg back, is supplied by the superior gluteal nerve.
- The gluteus medius and minimus muscles, which aid in hip abduction (moving the leg away from the midline) and rotation, are supplied by the inferior gluteal nerve.
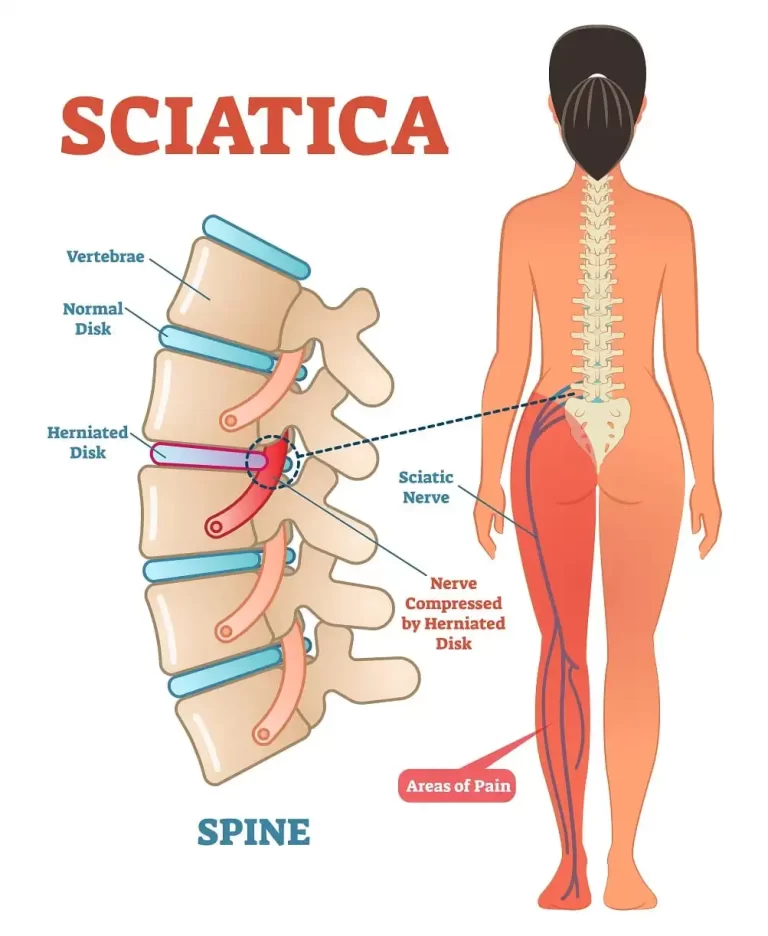
- Sciatic Nerve: The longest and greatest branch of the sacral plexus is the sciatic nerve. It travels along the back of the thigh before splitting into branches that supply innervation to the knee joint, lower leg and foot muscles, hamstring muscles, and leg and foot skin.
- Pudendal Nerve: Provides feeling to the perineum, which is the region between the genitalia and the anus, and innervates the pelvic floor muscles, which are critical for controlling the bladder and bowels.
- Additional Divisions: The quadratus femoris muscle, the piriformis muscle, and the skin on the back of the thigh and leg are innervated by several smaller nerves.
Physicians, physiotherapists, and chiropractors are among the healthcare providers who must comprehend the anatomy and function of the sacral plexus. Significant pain, weakness, and loss of sensation in the lower limbs can result from sacral plexus injuries.
Understanding the sacral plexus’s location and function aids in the diagnosis of these ailments and the development of effective treatment plans.
What is the Sacral Plexus Injury?
- A sacral plexus injury is the result of damage to The sacral plexus (collection of nerves in the lower back that are near the sacrum)nerves. It regulates how the legs, feet, and buttocks feel and move.
- Physical trauma can result in sacral nerve discomfort, particularly if the sacral nerve roots are injured. A few symptoms of this injury are somatic abnormalities affecting the buttocks and groin, side and rear leg pain, and lower back pain.
Causes of the Sacral Plexus Injury
Sacral plexus injuries have a variety of causes, which can be generally divided into traumatic and non-traumatic categories.
Traumatic Causes
- Fractures of the pelvis: A pelvic fracture may compress or harm The sacral plexus nerves. This is a frequent reason for sacral plexus injuries sustained in motorbike crashes, auto collisions, and height falls.
- Hip dislocation: The sacral plexus nerves may be torn or stretched by a dislocated hip.
- Delivery: Rarely, a painful delivery may cause sacral plexus injury in the infant. Obstetric brachial plexus palsy is the term for this.
- Surgical techniques: There are occasions when sacral plexus injury results from hip or pelvic surgery.
Not-Traumatic Reasons
- Diabetes: Diabetes can harm nerves in the sacral plexus as well as other parts of the body.
- Cancer: The sacral plexus may be compressed or invaded by a pelvic tumor.
- Radiation therapy: The sacral plexus may be harmed by radiation therapy administered to the pelvis.
- Infections: The sacral plexus may become inflamed and harmed by a pelvic infection.
- Autoimmune illnesses: The sacral plexus may sustain injury from autoimmune diseases that target the nerves.
- The degree of nerve damage determines how severe a sacral plexus injury will be. Sometimes the damage to the nerves is temporary, and sometimes it takes time for them to repair.
Symptoms of the Sacral Plexus Injury
Different symptoms can result from damage to the sacral plexus, depending on which nerves are impacted. Among the most typical symptoms are:
- The legs, buttocks, and lower back hurt. This pain may radiate down the sciatic nerve down the leg and feel burning, acute, or painful.
- Hips and legs feeling weak. As a result, walking, getting up from a seated posture, and climbing stairs may become challenging.
- Tingling or numbness in the feet and legs. This may impact the entire leg, the tops of the feet, or the soles of the feet.
- Lack of bladder or bowel control. This is a dangerous symptom that has to be treated right away by a doctor.
- Abnormal sexual dysfunction.
Risk Factors of the Sacral Plexus Injury
The following are a few Sacral Plexus Injury risk factors
- Pelvic fractures: A pelvic fracture may compress or harm The sacral plexus nerves. This is a frequent reason for sacral plexus injuries sustained in motorbike crashes, auto collisions, and height falls.
- High-energy impacts: Activities that entail a high risk of falls or collisions, such as contact sports, riding a motorbike, and horseback riding, can increase the risk of a sacral plexus injury since pelvic fractures are more likely to develop in these types of hits.
- Osteoporosis: This disorder weakens bones and increases their vulnerability to fractures. Osteoporosis increases the likelihood of pelvic fractures, which can lead to sacral plexus injuries.
- Certain difficulties during childbirth: Although rare, difficult deliveries, particularly those involving large babies, breech presentations, or the need for forceps or vacuum extraction, can raise the newborn’s risk of suffering damage to the sacral plexus.
- Hip surgery: The sacral plexus may occasionally sustain damage from hip surgery, such as hip replacement surgery.
- Diabetes: Nerves in the sacral plexus are among the many parts of the body that can be harmed by diabetes. Peripheral neuropathy, which can weaken muscles and make them more prone to injury, is more common in people with diabetes.
- Cancer: The sacral plexus may be compressed or invaded by a pelvic tumor.
- Radiation therapy: The sacral plexus may be harmed by radiation therapy administered to the pelvis.
- Infections: The sacral plexus may become inflamed and harmed by a pelvic infection.
- Autoimmune illnesses: The sacral plexus can sustain injury from autoimmune diseases that target the nerves, such as Guillain-Barre syndrome.
It is noteworthy that not all individuals exhibiting these risk factors will get a sacral plexus injury. On the other hand, being aware of the dangers can enable you to take precautions, such as wearing the appropriate safety gear during activities when there is a high risk of falls or collisions and, if you have diabetes, keeping appropriate blood sugar control.
Diagnosis for the Sacral Plexus Injury
Imaging studies, a thorough medical history, and a physical examination are usually used to diagnose a sacral plexus injury.
Medical History: Your doctor will probably ask you about your symptoms during the first appointment, including:
- When did your symptoms start?
- The location and intensity of your discomfort
- Have you ever experienced back or pelvic trauma?
- What underlying medical conditions you may have, such as diabetes or cancer?
Physical Examination: Your leg and foot sensitivity, reflexes, and muscle strength will all be evaluated during the physical examination. Additionally, your physician might look for symptoms of nerve injury like:
- Weakness or atrophy of the muscles
- Reduced or nonexistent reflexes
- Sensitivity or tingling
- lack of bladder or bowel control
Imaging Tests: Your doctor can see the sacral plexus and spot any nerve injury with the use of imaging techniques. The following imaging studies are frequently used to identify sacral plexus injuries:
- X-rays: X-rays can be used to diagnose pelvic fractures, which can cause the sacral plexus nerves to become compressed or injured.
- Magnetic resonance imaging (MRI): MRI scans can produce finely detailed images of the sacral plexus and the tissues around it, including the nerve roots and spinal cord. The most useful imaging test for identifying sacral plexus injury is frequently an MRI.
- Computed tomography (CT) scan: The sacral plexus and surrounding bones can be imaged with a CT scan. But when it comes to seeing nerves, CT scans are not as useful as MRIs.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): Tests that are used to evaluate the condition of the muscles and nerves include nerve conduction studies (NCS) and electromyography (EMG).
- EMG: To assess the electrical activity of a muscle, a tiny needle electrode is placed. This can assist in identifying any injury to the nerve that supplies the affected muscle.
- NCS: NCS gauges the electrical impulses’ intensity and speed as they pass through nerves. This can assist in determining the nerves that are impacted and how severely they are damaged.
These tests can be useful in certain situations, particularly if the diagnosis remains uncertain after the physical examination and imaging testing. However, they are not usually required to diagnose a sacral plexus injury.
Differential Diagnosis for the Sacral Plexus Injury
Various disorders share symptoms with a sacral plexus injury. A physician will make a differential diagnosis to separate a sacral plexus injury from these possibilities to guarantee appropriate therapy. The following are a few of the most typical ailments taken into account when making a differential diagnosis for a sacral plexus injury:
- Lumbosacral Radiculopathy: A single nerve root leaving the lower spine might become inflamed or compressed, resulting in lumbar radiculopathy. Similar to a sacral plexus injury, it can produce pain, paralysis, and numbness, but usually affects a smaller area.
- Sciatic Neuropathy: The main branch of the sacral plexus, the sciatic nerve, is the focus of this particular ailment. The sciatic nerve’s route causes discomfort that radiates down the back of the leg. Sciatic neuropathy alone may not always indicate damage to the complete sacral plexus, even though it can accompany a sacral plexus injury.
- Cauda Equina Syndrome: This dangerous disorder is characterized by compression of the spinal cord’s bottom nerve bundle. Unlike sacral plexus injuries, which may only affect one side, it results in paralysis, numbness, and bowel/bladder dysfunction in both legs.
- Conus Medullaris Syndrome: Symptoms of this disorder are similar to those of cauda equina syndrome, however, they usually appear more gradually. The condition is caused by damage to the spinal cord itself.
- Spinal Stenosis: When the spinal canal narrows, spinal nerves may be compressed, resulting in pain, weakness, and numbness in the legs. Still, the way these symptoms are distributed can help distinguish it from sacral plexus damage.
- Peripheral neuropathy: This broad term describes damage to nerves anywhere in the body, resulting from a variety of conditions such as vitamin shortages or diabetes. Similar to a sacral plexus injury, it can cause widespread weakness, numbness, and discomfort, although the pattern might not be limited to the legs or buttocks.
- Musculoskeletal Conditions: Some symptoms of a sacral plexus injury, such as pain and weakness, can be mimicked by muscle strains, ligament tears, or even bone fractures in the leg or pelvis. Differentiating between these disorders can be aided by imaging studies and a comprehensive physical examination.
A physician can determine the most accurate diagnosis and suggest the best course of therapy by taking into account these alternative diagnoses in addition to the patient’s symptoms, history, and test results.
Treatment and Management for the Sacral Plexus Injury
The degree of nerve damage determines the therapy and treatment plan for a sacral plexus injury. Below is a summary of the many methods:
General Measures:
- Pain Management: Pain management throughout the early phases is essential for comfort and healing. Prescription drugs may include non-steroidal anti-inflammatory drugs (NSAIDs), opioids (use with caution as there is a risk of dependence), or pharmaceuticals specifically designed to treat nerve pain, such as gabapentin or pregabalin.
- Physical Therapy: Physical treatment is essential to the healing process. A program to enhance muscle strength, flexibility, and coordination in the impacted limb or legs will be created by a therapist. Neural regeneration can also be aided by methods such as electrical stimulation.
Treatment Dependent on Severity of Nerve Injury
Non-surgical Treatment for Mild to Moderate Injuries: A conservative approach is advised for injuries where there is a possibility of the nerves recovering on their own. This entails physical therapy, pain management, and sometimes bracing or splinting to support weakening muscles.
Surgical Intervention (For severe Injuries): Surgery may be required if there is substantial nerve damage or if the injury isn’t getting better with conservative therapy. There are primarily two surgical methods:
- Nerve Repair: Direct reattachment of severed or injured nerves is the goal of surgery. To fill in the spaces between damaged nerve terminals, nerve grafts from other body regions may be utilized in specific situations.
- Nerve Transfers: If direct repair is not achievable injured nerves can be replaced by healthy nerves from neighboring regions.
Physical Therapy for the Sacral Plexus Injury
After suffering a sacral plexus injury, physical therapy (PT) is an essential part of the healing process. A physical therapist can create a customized plan to meet your unique needs and goals, to enhance:
- Muscle Control and Strength: One common side effect of sacral plexus injuries is weakness. Physical therapy (PT) enhances stability, gait, and general function by strengthening weak muscles in the hips, legs, and core.
- Range of Motion and Flexibility: A sacral plexus injury may result in hip and leg rigidity. Stretching exercises are incorporated into physical therapy to increase the range of motion and flexibility, enabling more effective movement.
- Balance and coordination: These two skills might be impacted by nerve injury. Exercises designed to test your balance system and enhance your coordination will lower your chance of falling.
- Pain Management: PT modalities, such as electrical stimulation, manual therapy techniques, and therapeutic ultrasonography, can aid in the management of pain and facilitate the healing process.
- Gait Training: PT can assist you in relearning how to walk safely and effectively, depending on the extent of your injury. This could entail gait retraining exercises, starting with walking assistance like crutches or canes, and working your way up to independent walking.
- Functional Activities: Enhancing your capacity to carry out everyday tasks is the ultimate aim of physical therapy. To help you become more independent, the therapist will integrate exercises that mimic everyday motions like getting out of a chair, ascending stairs, or getting dressed.
The following describes some particular PT methods that can be applied to an injury to the sacral plexus:
- Strengthening exercises: To target weak muscles, these workouts use weights, resistance bands, body weights, or other equipment. As you advance, the therapist will progressively up the level of difficulty and intensity of the workouts.
- Range-of-Motion Exercises: Targeting tight muscles and increasing hip, leg, and core flexibility are the goals of stretching exercises. This could be using yoga straps or other props, or it could just be mild manual stretches.
- Balance Training: Activities that test your balance system include wobble boards, standing on one leg, and other balance-related exercises.
- Gait Training: The therapist will watch how you walk and look for any weaknesses. After that, they will lead you through gait-improvement exercises like practicing correct heel-toe strikes and stepping over obstacles.
- Neuromuscular Re-education: After an accident, muscles that have lost contact with the nerves can be retrained using methods such as electrical stimulation or biofeedback.
- Assistive Devices: To support weak muscles and enhance walking, a physical therapist may initially advise utilizing assistive devices like crutches, canes, or ankle-foot orthoses (AFOs).
Additional Things to Consider About:
- Timeline: Depending on your injury’s seriousness, the PT program’s length will vary. After suffering a sacral plexus damage, recovery might take months or even years.
- Exercise Programme at Home: To supplement the in-clinic sessions and encourage long-term progress, your physical therapist will create a routine at home for you to follow.
- Communication is key. Communicate frequently with your physical therapist. Make sure to let them know about any restrictions or worries you have so they can modify the program.
- Recall that physical therapy is a team endeavor. After suffering a sacral plexus injury, you can increase your chances of regaining strength, function, and independence by fully engaging in your PT sessions and adhering to your at-home exercise program.
Complications for the Sacral Plexus Injury
Damage to the sacral plexus can result in several issues, some of which are lifelong. Below is a summary of the possible issues:
- Weakening and Paralysis of the Muscles: The muscles regulated by the damaged nerves may experience weakening or even paralysis, depending on the extent of the injury. This may have a major effect on everyday activities and movement.
- Chronic Pain: Abnormal pain signals can be sent by damaged nerves, resulting in persistent discomfort in the feet, legs, or buttocks. It can be quite painful and challenging to control.
- Neuropathic Pain: This particular kind of nerve pain can be very difficult to treat and frequently has a burning, tingling, or shooting sensation.
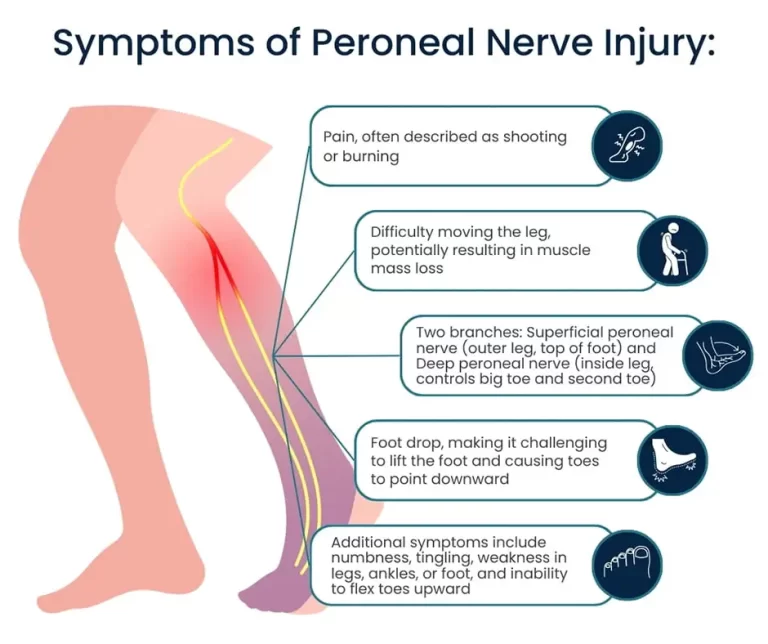
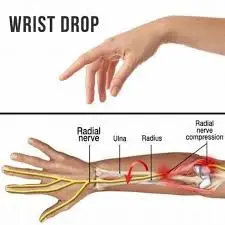
- Movement Disorders: Abnormal movement patterns, such as foot drop or trouble swinging the leg during walking, can be caused by muscle weakness and nerve injury.
- Joint contractures and stiffness: Weakness and pain over time can cause stiffness in the hip and knee joints. If left untreated, this stiffness may develop into joint contractures that impair joint motion permanently.
- Issues with Coordination and Balance: A lesion to the sacral plexus may impair balance and coordination, raising the possibility of falls.
- Bladder and intestine Dysfunction: Severe cases may cause damage to the nerves that regulate the bladder and intestine, which may result in incontinence or constipation.
- Skin Issues: Due to diminished sensitivity and an inability to take proper care of the feet, weakness and numbness in the legs and feet might raise the risk of skin infections and accidents.
- Psychological Distress: Social isolation, anxiety, and despair can result from long-term conditions that require constant care, chronic pain, and incapacity.
Management of Complication:
- Management of Spasticity: In rare circumstances, nerve injury may result in spasticity or uncontrollably stiff muscles. Injections, medications, and physical therapy methods can all be used to reduce spasticity and increase range of motion.
- Bladder and Bowel Dysfunction: If there is an issue with the control of the bowels or bladder, a gastroenterologist or urologist may be consulted to determine the best course of action. This may involve the use of catheters, bowel programs, or medication.
- Psychological Support: Managing a long-term injury to the sacral plexus can be difficult. Support groups or psychological counseling might help manage emotional health.
Prevention for the Sacral Plexus Injury
Although it can be difficult to completely prevent a sacral plexus injury, there are things you can take to lower your risk. Based on the various risk variables, the following strategies are suggested:
Pelvic Fracture Prevention:
- Airbags and seatbelts: When driving, buckle up, and make sure your airbags are working.
- Motorbike Helmets: When riding a motorbike, always wear a helmet that fits properly.
- Fall Protection: If you or someone you know is elderly, weak, or has trouble with their balance, consider taking preventative steps like placing grab bars in bathrooms, upgrading lighting in your house, and dressing appropriately.
Steer clear of high-impact activities:
- Wear the proper protective gear when engaging in high-risk activities such as horseback riding or contact sports.
- Strengthening Exercise: Stability can be increased and the impact of falls may be lessened by routinely exercising the leg and core muscles.
Managing medical Factors:
- Diabetes management: Preventing diabetic neuropathy and indirectly lowering the risk of sacral plexus injury can be achieved by maintaining appropriate blood sugar management through food, exercise, and medication.
- Preserving Bone Health: Appropriate diet, weight-bearing exercise, and medication can help preserve strong bones and reduce the risk of fracture for people who have osteoporosis or are at risk for it.
Considerations for Pregnancy and Childbirth:
- Prenatal Care: Getting regular prenatal care can help detect any pregnancy-related issues that may raise the baby’s chance of suffering sacral plexus damage.
- Delivery Schedule: Speaking with your doctor about your delivery options might help reduce the danger of procedures like vacuum extraction or forceps, which in some situations may raise the risk of sacral plexus injury.
General Safety Procedures:
- Safe Lifting Practices: Use good form when carrying big goods to prevent straining your pelvis and back.
- Sustaining a Healthy Weight: Being overweight puts more strain on the pelvis and lower back, therefore it may be helpful to maintain a healthy weight.
Conclusion
Recovery from a sacral plexus injury can vary widely, ranging from partial to full recovery depending on the extent of the damage and the effectiveness of treatment. Physical therapy and rehabilitation are often crucial components of the recovery process to help regain function and mobility.
In some cases, individuals may experience long-term effects such as chronic pain or weakness despite treatment. Early diagnosis and prompt treatment can improve the outlook for recovery in many cases.
FAQs
What occurs in a case of sacral plexus injury?
Disease, trauma, or cancer can all have an impact on the sacral plexus or portions of it. The symptoms can be confused due to the large number of branches and sections that make up this nerve network. You might have discomfort or sensory loss in some areas of your leg and pelvis, along with or without muscle weakness.
How can injury to the sacral nerve be repaired?
Typical courses of treatment consist of Anti-inflammatory drugs.
To remove any potential pressure on the nerves, surgical decompression is performed.
Regaining normal strength and function requires both physical and occupational therapy.
What signs of compression of the sacral nerve are present?
Lower back pain. ache running down your legs from rear to front. muscle spasms in your body. loss of feeling for cold or heat.
What is the sacral plexus’s primary purpose?
The posterior thigh, most of the lower leg, the entire foot, and a section of the pelvis are supplied with motor and sensory nerves by the nerve plexus known as the sacral plexus (plexus sacralis).
What complications might a sacral injury cause?
Individuals suffering from damage to the sacral nerve roots may encounter:
Loss of bladder or bowel control.
back ache in the lower back.
Leg pain that could perhaps travel down the back of the leg.
problems with the buttocks and groin area.
What is the duration of sacral nerve healing?
For the first two weeks, refrain from taking long showers or baths to allow the wound to heal completely. After a week, you should have your dress changed. Under typical conditions, you should be able to resume your regular activities in two to four weeks.
Which two nerves make up the sacral plexus?
The lumbosacral trunk and sacral spinal nerves make up the sacral plexus, a network of nerves. The lumbar spinal nerves L4 and L5 combine to produce the lumbosacral trunk. The roots of sacral spinal nerves S1 through S4 originate from the spinal cord and are met by the trunk as it descends into the pelvis.
References
- Moawad, H., MD. (2023, April 28). An overview of the Sacral Plexus. Verywell Health. https://www.verywellhealth.com/sacral-plexus-anatomy-4689205
- Mans, C., Steagall, P. V., & Sladky, K. K. (2019). Regional anesthesia and analgesia. In Elsevier eBooks (pp. 475-479.e1). https://doi.org/10.1016/b978-0-323-48253-0.00051-9
- Understanding Sacrum Fractures and Injuries | Shepherd Center. (n.d.). https://www.shepherd.org/programs/spinal-cord-injury/levels-and-types/sacral-spinal-cord-injury
- sacral nerve plexus: Topics by Science.gov. (n.d.). https://www.science.gov/topicpages/s/sacral+nerve+plexus
- Permanent Sacral Nerve Neuromodulation – For the Treatment of Faecal Incontinence Pelvic Floor Disorders | Hull University Teaching Hospitals NHS Trust. (2023, January 26). Hull University Teaching Hospitals NHS Trust. https://www.hey.nhs.uk/patient-leaflet/permanent-sacral-nerve-neuromodulation-treatment-urinary-disorders-faecal-incontinence-constipation-pelvic-floor-disorders pain/