Restless Legs Syndrome (RLS)
What is The Restless Legs Syndrome?
Restless Legs Syndrome (RLS) is a neurological disorder characterized by an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations like tingling, itching, or aching.
Symptoms typically worsen during rest or inactivity, especially in the evening or at night, leading to disrupted sleep. The exact cause is unknown, but it is linked to dopamine dysfunction and may have genetic, iron deficiency, or other underlying factors. Treatment includes lifestyle changes, iron supplementation (if deficient), and medications in severe cases.
All ages can be affected by RLS, however middle-aged and older adults are more likely to have it. It is also known as “pregnancy-related RLS” when it affects expectant mothers. While RLS is normally a non-life-threatening disorder, its impact on quality of life and sleep can be severe, leading to physical and emotional suffering.
Modest lifestyle adjustments and self-care practices may help reduce symptoms. Additionally, a lot more patients with RLS benefit from medications.
The impulse to move the legs (rarely the arms) and strange, unpleasant sensations (paraesthesia) deep in the legs are symptoms of the widespread neurological condition known as restless leg syndrome (RLS). Sensations often diminish with movement and resurface with rest or inactivity, particularly at night and in the evening. Unpleasant paraesthesia can significantly disrupt sleep. People with RLS, sometimes referred to as Willis-Ekbom disease, are compelled to move their legs. RLS is a common, long-term, complex limb movement disorder. Unusual, non-painful sensations that start at rest and get better with movement are commonly associated with RLS. Symptoms tend to worsen at night on a daily basis. There are over three million cases in the US annually.
RLS has been described as either a symptomatic syndrome commonly associated with anemia, pregnancy, or end-stage renal failure, or as an idiopathic illness with no known etiology. But there are underlying genetic, environmental, or both variables that contribute to the condition’s complexity. The fact that the disease initially appears in childhood indicates a significant hereditary component, despite the fact that the start can vary widely, from an early age to over 80 years of life. New epidemiological studies employing community samples have revealed that between 3% and 10% of persons exhibit the primary symptoms of RLS, despite previous underestimations of the condition’s incidence.
Epidemiology of restless leg syndrome:
An estimated 2.5–15% of Americans suffer from RLS. A small percentage of people (about 2.7% of the population) have severe or ongoing symptoms. RLS affects women twice as frequently as it does males, and it is more common in Caucasians than in persons of African origin. RLS affects 3% of people from the Mediterranean or Middle East and 1% to 5% of those from East Asia, suggesting that various environmental or genetic variables, such as nutrition, may contribute to the syndrome’s incidence. The course of RLS is more severe when it is identified later in life. Those with end-stage kidney disease, pregnancy, or iron insufficiency are even more likely to get RLS. According to the 1998 Sleep in America survey by the National Sleep Foundation, up to 25% of expectant mothers experienced RLS in the third trimester. It is also associated with poor general health.
Uremia, familial history, and advanced age are some of the risk factors for RLS. RLS is more common as people age, and its symptoms also tend to get worse and last longer. The prevalence of uremia in patients undergoing renal dialysis ranges from 20% to 57%, but outcomes for kidney transplant recipients are better than those for dialysis patients.
Although it can happen at any age, RLS typically first appears in the third or fourth decade of life. Nineteen risk loci have been linked to RLS by genome-wide association studies. Parkinson’s disease, spinal cerebellar atrophy, spinal stenosis, [specify] lumbosacral radiculopathy, and Charcot-Marie-Tooth disease type 2 are among the neurological disorders associated with RLS.
Pathophysiology
The characteristic of RLS, a neurological condition usually accompanied by unpleasant sensations, is uncontrollable desires to move the legs. Although the precise pathophysiology of RLS is still unclear, a number of processes have been suggested as likely causes. Iron levels in the brain are known to have a major impact on RLS. Iron deficiency has been linked to blood-brain barrier (BBB) dysfunction, which can lead to altered iron conduction across the BBB and reduced iron storage in brain endothelial cells. This deficiency can affect a number of processes, including neurotransmitter synthesis and metabolism, and result in oxidative damage.
Dopaminergic cells are especially susceptible to iron shortage because of their role in controlling movement, which might interfere with dopamine transmission and potentially result in RLS symptoms. The dopaminergic system, which is essential for controlling movement and rewarding behavior, is intimately associated with RLS. It has been demonstrated that medications that change dopamine levels can change the symptoms of RLS. By altering the action of specific enzymes involved in the synthesis of dopamine, iron deficiency may result in dopaminergic dysfunction. Dopaminergic A11 cells in the midbrain are thought to play a key role in the pathophysiology of RLS because they appear to be engaged in the spinal cord’s dopamine production. Changes in thalamic activity caused by dopaminergic input are also connected to RLS.
RLS susceptibility is significantly influenced by genetic factors. It has been discovered that a number of genetic variants, including MEIS1, BTBD9, PTPRD, and MAP2K5, increase the incidence of RLS. These genes include examples of those linked to iron homeostasis, dopamine synthesis, sleep regulation, and the development of embryonic neurons. These genes’ interactions with the dopamine and iron metabolism pathways may have an impact on the development of RLS. Research on the pathophysiology of RLS has focused on regions of the brain like the basal ganglia, dopaminergic A11 cell group, and substantia nigra. A11 cells, which regulate sensory, motor, and autonomic processes, send dopaminergic impulses to the spinal cord. RLS has been associated with changes in cerebral and thalamic activity as well as hyperexcitability in the spinal cord.
Mechanism of the Restless Legs Syndrome (RLS)
The pathogenesis of restless legs syndrome may involve abnormalities in the dopamine and iron systems, though this is yet not fully understood. Additionally, it has a widely accepted explanatory mechanism that can be clinically demonstrated by body temperature and other circadian rhythm biomarkers. The development of RLS is influenced by the interplay between decreased neuronal iron uptake and the activities of the neuromelanin-containing and dopamine-producing cells, suggesting that iron deficiency may have distinct effects on brain dopaminergic transmissions.
Along with the limbic system, which is influenced by the dopaminergic system and may impact pain perception, medial thalamic nuclei may also play a function in RLS. Patients on low-dose dopamine agonists experience an improvement in their RLS symptoms.
What are the types of restless legs syndrome?
Principal RLS and secondary RLS are the two principal forms of RLS.
Although the exact cause of RLS is unknown, it might have something to do with the way the body handles dopamine, a neurotransmitter involved in muscle contraction regulation. Pregnancy is also connected to it.
Primary or idiopathic RLS
- Idiopathic denotes an unidentified etiology. In between 25% and 75% of cases, there may be a familial connection, suggesting that it has a genetic origin.
- Usually, primary RLS starts before the age of forty.
Secondary RLS
The cause of secondary RLS is another condition. The following are some examples of situations that can result in secondary RLS:
- diabetes
- iron deficiency
- kidney failure
- Parkinson’s disease
- peripheral neuropathy
- venous insufficiency
- pregnancy
- fibromyalgia
- celiac disease
Secondary RLS can also result from certain drugs, especially those that interfere with dopamine action. The following are some examples of drugs that may induce or exacerbate secondary RLS:
- selective serotonin reuptake inhibitors (SSRIs)
- serotonin-norepinephrine reuptake inhibitors (SNRIs)
- tricyclic antidepressants
- beta-blockers
RLS and periodic limb movement disorder (PLMD) can coexist. A related sleep condition called PLMD makes the limbs jerk or twitch uncontrollably while you’re asleep.
Causes of the Restless Legs Syndrome (RLS)?
Restless Legs Syndrome (RLS) frequently has no identified etiology. Researchers believe that a discrepancy in the brain chemical dopamine, which sends impulses to regulate muscle action, may be the cause.
Heredity
RLS can occasionally run in families, particularly if it first manifests before the ages of 35 to 40. Researchers have identified potential locations for Restless Legs Syndrome (RLS) genes on the chromosome.
Pregnancy
Signs and symptoms of Restless Legs Syndrome (RLS) may be momentarily exacerbated by pregnancy or hormonal changes. Some pregnant women experience their first episode of Restless Legs Syndrome (RLS), particularly in the final trimester. till the symptoms often go away after giving birth.
Symptoms of the Restless Legs Syndrome (RLS)?
The RLS has a long history, but Ekbom was the first to recognize it as a distinct clinical entity in 1944. The factors that are essential for diagnosing this illness, however, have not yet been agreed upon by a large worldwide study group. The following four clinical characteristics of RLS were determined by this study to be the least requirement for diagnosis. When patients are impelled to move and employ different motor strategies to alleviate discomfort related to their restless legs, motor restlessness must also be present. The affected limbs must move at least partially and severely, and the symptoms must be more severe in the evening or at night or only present when at rest (i.e., sitting or lying down).
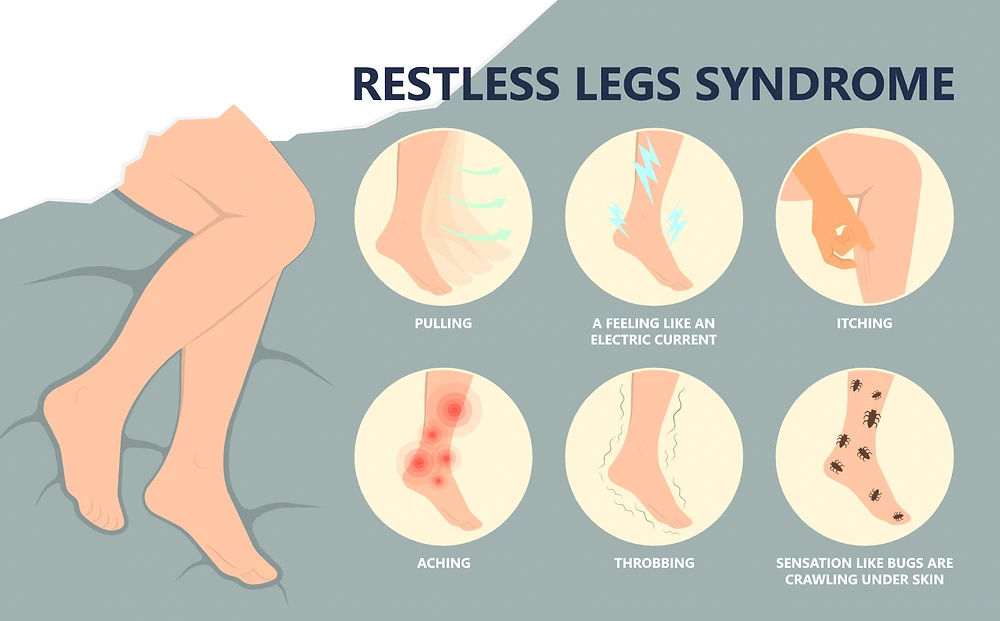
The urge to move the legs is the main symptom. The following are typical symptoms that accompany restless legs syndrome (RLS):
- Feelings that start while you’re sleeping: These sensations typically start after you’ve been sitting or lying down for a time, such as in a theater, an automobile, or an airplane.
- Movement-induced relief: Walking, stretching, or jiggling the legs can all help reduce the symptoms of restless legs syndrome.
- Symptom worsening in the evening: The majority of symptoms occur at night.
- Leg twitching at night: Periodic limb movement of sleep, a much more common condition that may be linked to restless legs syndrome (RLS), is characterized by the legs kicking and twitching, possibly during the night, while you sleep.
- The symptoms of restless legs syndrome (RLS) are typically described as strong, disagreeable feelings in the legs or feet. Usually, both sides of the body experience them. The arms are frequently affected by the sensations.
The following are some descriptions of the sensations, which typically occur inside the limb rather than on the skin:
- Crawling,
- Creeping,
- Pulling,
- Throbbing,
- Aching,
- Itching,
- Electric.
The feelings can be difficult to describe at times. RLS sufferers typically don’t characterize their symptoms as numbness or cramping in their muscles. They do, until they often talk about wanting to move their legs.
It’s common for the intensity of symptoms to change. Symptoms can occasionally disappear for a while before returning.
Risk factors
Even in childhood, restless legs syndrome (RLS) can strike at any age. The illness is more common in women than in males, and it becomes considerably more common as people age.
Typically, there is no significant underlying medical issue linked to restless legs syndrome (RLS). Until it occasionally comes with additional conditions, such as:
- Peripheral neuropathy: Chronic conditions like diabetes and alcoholism can occasionally cause damage to the nerves in the hands and feet.
- Iron deficiency: Iron deficiency can induce or exacerbate restless legs syndrome (RLS) even in the absence of anemia. You may be at risk for iron insufficiency if you have a history of gastrointestinal bleeding, have heavy periods, or donate blood frequently.
- kidney failure: Iron deficiency, frequently accompanied by anemia, may also be present in individuals with renal failure. Iron levels in the blood may decrease as a result of renal dysfunction. RLS may be caused by or made worse by these and other alterations in bodily chemistry.
- Spinal cord disorders: Restless Legs Syndrome (RLS) has been connected to spinal cord lesions caused by injury. Restless Legs Syndrome (RLS) is also less likely to occur after spinal cord anesthesia, such as a spinal block.
- Parkinson’s disease: Individuals with Parkinson’s disease who use certain medications known as dopaminergic agonists are more likely to get RLS.
Diagnosis
To diagnose RLS, the clinical history is evaluated. If there is a medical possibility of sleep apnea or if sleep issues persist even after RLS symptoms have been treated, polysomnography should be done. Iron status (the serum ferritin level and iron saturation) should be evaluated because RLS frequently happens without anemia and may be a sign of iron shortage. Additional laboratory tests ought to be performed. essential requirements for RLS diagnosis. the International Restless Legs Study Group’s criteria for RLS.
The desire to move one’s legs due to discomfort that radiates from the legs to the feet is one of the symptoms of the diagnosis. It is possible that painful sensations in the arms will accompany the need to move the legs. During periods of idleness or sleep, there may be a desire to move the legs. Movement may or may not completely alleviate the restlessness. Unpleasant feelings or the need to move may only happen at night or be worse at night than during the day.
After reviewing your medical history, your doctor will ask you to describe your symptoms. The following standards, developed by the International Restless Legs Syndrome (RLS) Study Group, are necessary for a diagnosis of RLS:
- You have a powerful, frequently alluring need to move your legs, which is frequently accompanied by unpleasant feelings.
- Resting, such as sitting or lying down, is when your symptoms start or worsen.
- Activity, such as stretching or walking, can temporarily or partially alleviate your discomfort.
- The severity of your symptoms increases at night, and they cannot be well explained by another behavioral or medical issue.
- Your physician may do neurological and physical examinations. In order to rule out further potential reasons of your symptoms, blood tests may be conducted, especially for iron deficiency.
Additionally, you may be sent to a sleep specialist by your provider. If another sleep condition, such as sleep apnea, is suspected, this may include an overnight stay and a study at a sleep clinic. However, a sleep study is typically not required for a diagnosis of restless legs syndrome (RLS).
History and Physical Examination:
Sensations that are localized to deep structures rather than the surface, such as crawling, creeping, pulling, itching, drawing, or stretching, are described by patients. Typically, there is no sensitivity to skin contact and no pain or tingling paresthesia of the kind seen in severe peripheral neuropathy.
Some patients may have relatively minor issues, while others may have significant sleep disturbances and quality of life deficits. The symptoms usually peak at night, within 15 to 30 minutes of lying down in bed, and they usually get worse toward the end of the day. In extreme situations, the patient may have symptoms earlier in the day when seated, making it difficult for them to participate in activities like going to meetings or watching movies.
In less severe situations, people will shift about in bed, kick, or massage their legs to feel better. On rare occasions, the arms could be impacted. In order to alleviate their symptoms, patients with more severe ones feel compelled to get out of bed and pace the floor. Involuntary, strong dorsiflexion of the foot lasting 0.5 to 5 seconds, occurring every 20 to 40 seconds during sleep, is a characteristic of periodic leg movements of sleep. While you sleep, you might twitch your limbs. Eighty percent of RLS sufferers experience them. Patients with RLS typically have normal physical examination results. The purpose of it is to find secondary causes.
Essential diagnostic criteria (all must be met):
- Unpleasant and uncomfortable sensations may accompany an insatiable desire to move the lower extremities.
- During the day, the impulse to move the extremities is less intense, but it gradually gets worse at night and in the evenings. Additionally, the symptoms manifest while at rest or during times of inactivity and sleep.
- Walking or stretching the legs can help to partially or totally reduce the urge to move the lower extremities. As long as the activity is continuing, the symptoms are either negligible or nonexistent.
- In the evenings, the impulse to move the lower extremities intensifies, making it impossible to fall asleep. As a result, the patient frequently feels exhausted during the day.
- It is important to rule out other behavioral disorders including tardive dyskinesia, leg cramps, muscular spasms, or positional pain when these symptoms are present.
During sleep, the leg movements, which are typically involuntary, may include abrupt dorsiflexion motions that last one to five seconds and repeat every thirty to forty seconds. Children typically have a positive family history. The physical examination is typically routine. To rule out a neurological condition, radiculopathy, or Parkinson’s disease, the patient must be examined.
Evaluation
Other than tests to rule out secondary causes, there are no tests to diagnose RLS. Additionally, blood tests is performed to rule out other causes. If neuropathy or radiculopathy is suspected, nerve conduction tests and electromyography are performed. To measure the frequency of leg movements and describe the sleep pattern, polysomnography is frequently used. Every patient with RLS symptoms should have an iron study completed. Serum iron, ferritin, transferrin saturation, and total iron-binding capacity are all important components of detailed iron investigations. If a full iron panel is not available, at least a ferritin level should be performed. When a patient’s RLS is under control but their symptoms reappear or worsen, they should once more undergo an evaluation of their iron status.
- The onset of symptoms sooner in the evening
- Morning symptoms are more severe.
- Upper body symptoms are also present.
A complete blood count and an assessment of the following levels should be performed, among other laboratory tests, if a secondary cause is suspected:
- Blood urea nitrogen
- Fasting blood glucose
- Creatinine
- Magnesium
- Vitamin B-12
- Thyroid-stimulating hormone
- Folate
Regarding the nervous system, if radiculopathy or polyneuropathy seems likely based on clinical examination, nerve conduction investigations and needle electromyography should be taken into consideration, even if the neurological examination is normal.
Differential Diagnosis
Leg cramps, positional pain, local leg injuries, arthritis, leg edema, venous stasis, peripheral neuropathy, radiculopathy, repetitive foot tapping/leg rocking, anxiety, myalgia, and drug-induced akathisia are the most prevalent disorders that should be distinguished with RLS.
Leg discomfort can also be caused by peripheral artery disease and arthritis, but it usually gets worse as you walk.
Among the less frequent differential diagnoses are myelopathy, myopathy, hypotensive akathisia, vascular or neurogenic claudication, orthostatic tremor, aching legs, and wiggling toes.
- Tardive dyskinesia
- Akathisia
- Leg cramps
- Vascular disease
- Muscle spasms
- Radiculopathy
Treatment of Restless Legs Syndrome:
RLS is no known cure, however there are a number of therapy options that can help control the symptoms and enhance the general health of those who are impacted. The discomfort linked to restless legs syndrome can be reduced by medication, lifestyle modifications, and avoiding specific triggers. For those with RLS symptoms to receive an accurate diagnosis and a customized treatment plan, speaking with a healthcare expert is crucial.
RLS symptoms can occasionally be significantly reduced by treating a primary illness, such as iron deficiency. Oral or intravenous iron supplements may be necessary to treat an iron deficiency. However, only use iron supplements under medical supervision and following a blood iron level test from your healthcare professional.
The goal of treatment for restless legs syndrome (RLS) without an accessory ailment is to modify one’s lifestyle. Your healthcare professional may suggest medication if those don’t work.
Reducing or eliminating the patient’s leg discomfort when they sleep or rest is the major objective. Resolving sleep disturbances caused by RLS is also crucial. Patients will feel more refreshed if they can manage their daily weariness and fatigue caused by sleep disruption. The main goal is to enhance the patient’s quality of life. Techniques for managing RLS include both pharmaceutical and non-pharmacological therapy. Non-pharmacological Other options for managing RLS include changing one’s lifestyle to abstain from substances that aggravate the condition, such as alcohol, coffee, and nicotine; engaging in activities that stretch the muscles in the back of the legs; and using heat to relieve pain by applying hydrocollator packs or warm baths. Iron replacement therapy may be helpful for people with low serum ferritin levels.
Medical Treatment of Restless Legs Syndrome:
There are numerous prescription medications available to reduce leg anxiety, the majority of which were created to treat other illnesses. These include:
- Drugs that increase dopamine in the brain: These drugs have an impact on the brain’s dopamine levels. The Food and Medication Administration has approved rotigotine (Neupro) and pramipexole (Mirapex) for the treatment of moderate to severe RLS.
- These drugs often have modest short-term side effects, such as weariness, lightheadedness, and nausea. However, they can also result in daytime sleepiness and impulse control problems like compulsive gambling.
- Calcium channel-affecting medications: Some persons with RLS respond well to certain drugs, such as pregabalin (Lyrica), gabapentin enacarbil (Horizant), and gabapentin (Neurontin, Gralise).
- Muscle relaxants and sleep aids: These medications help you sleep at night, but they don’t stop leg pain and may make you drowsy throughout the day. Usually, these medications are only used when no additional therapy is effective.
- Opioids: Narcotic drugs are primarily used to treat acute symptoms, but excessive use of them can lead to addiction. Examples include codeine, hydrocodone (Hysingla ER), oxycodone (Oxycontin), tramadol (Ultram, ConZip), and more.
- Finding the ideal medication or drug combination for you may need a number of trials between you and your healthcare provider.
Caution about medications
Restless legs syndrome can occasionally be treated with dopamine medications that must work for a while, or you may discover that your symptoms, including those in your arms, return earlier in the day. We refer to this as augmentation. To address the issue, your doctor may recommend a different prescription.
Pregnancy is not advised when using the majority of medications used to treat restless legs syndrome (RLS). Alternatively, your doctor may recommend self-care techniques to alleviate symptoms. However, your doctor may authorize the use of specific medications if the symptoms are especially unpleasant during your last trimester.
Certain medications may exacerbate restless legs syndrome (RLS) symptoms. A few antidepressants, antipsychotics, nausea-relieving medications, and cold and allergy medicines are among them. If at all feasible, your doctor may advise you to stay away from these medications. However, if you must take these drugs, discuss with your doctor the possibility of taking other medications to help control your restless legs syndrome (RLS).
Physical Therapy Treatment of Restless Legs Syndrome:
Yoga and Pilates
Numerous other experts recommended yoga, Pilates, and aerobics as ways to help with the symptoms of restless legs syndrome (RLS), but they also advised against doing Ashtanga, hot yoga, or any other pose that is particularly troublesome or puts undue strain on the body.
Cycling
Another activity that helps reduce discomfort is cycling. Aim for 8 to 10 miles per hour or a little bit slower if you want to ride at a leisurely pace.
Swimming
Swimming In a warm pool, swimming or water aerobics helps you relax your muscles while gaining strength and improving your range of motion.
Stretching may help prevent the symptoms of Restless Legs Syndrome (RLS). To help you get started, here are some stretches.
Calf stretch

- Extend your arms until your elbows are almost straight and your hands are flat against a wall.
- Your left leg is stepped back a foot or two and your right knee is bent to a small degree, placing your foot and heel flat on the ground. For 15 to 30 seconds, hold.
- Then, with your heel and foot flat on the floor, bend your left knee.
- Move your foot back a little bit for a deep stretch.
- Repeat with a different leg.
Front thigh stretch
- Pull one ankle across your back while maintaining a straight leg while standing with your back to a wall for balance.
- For 15 to 30 seconds, hold.
- Repeat with a different leg.
Hip flexor stretch

- For assistance, position the back of a chair across from the wall and face the chair.
- With your knee bent, elevate your left foot and lay it flat on the chair. (Alternatively, attempt to balance by placing your foot on a stair while maintaining the guardrail.)
- Maintaining a neutral spine, gradually push your pelvis forward until you feel a stretch at the top of your right thigh. Your pelvis will just slightly advance.
- For 15 to 30 seconds, hold.
- Repeat with a different leg.
You can alleviate the symptoms of Restless Legs Syndrome (RLS) by engaging in mild to moderate exercise. Discuss effective weekly daily routines that will work best for you with your physician. Make sure to ask them about safe activities for you if you are pregnant.
Lifestyle and home remedies of Restless Legs Syndrome:
Simple lifestyle adjustments can help reduce restless legs syndrome (RLS) symptoms:
- Try massages and baths: You can relax your muscles by rubbing your legs and soaking in a warm bath.
- Put on cool or warm packs: Applying heat or ice, or switching between the two, may lessen the symptoms in the limbs.
- Start practicing good sleep hygiene: It’s important to maintain good sleep hygiene because fatigue can exacerbate symptoms of restless legs syndrome (RLS). Get at least 7 (seven) hours of sleep every night, ideally in a calm, peaceful, and well-sleeping environment, and go to bed and wake up at roughly the same time every day.
- Exercise: Regularly engaging in moderate exercise may help reduce the symptoms of restless legs syndrome (RLS); but, overdoing it or exercising too late in the day may make them worse.
- keep away of caffeine: Reducing caffeine intake can help with restless legs. For a few weeks, stay away from anything that contains caffeine, such as chocolate, coffee, tea, and soft drinks. See if this helps.
- Think about applying a vibrating pad or a foot wrap: Wearing a foot wrap applies pressure to the foot, potentially alleviating symptoms of restless legs syndrome. Applying a vibrating pad to the back of your legs may also help.
Coping and support
The disorder known as restless legs syndrome (RLS) frequently lasts a lifetime. It could help you create coping mechanisms that are effective for you, such as:
- Inform them that you suffer from Restless Legs Syndrome (RLS): Giving your friends, family, and coworkers information about restless legs syndrome (RLS) will help them understand you when they watch you go to the water cooler, pace the halls, or stand in the back periodically.
- Avoid putting up with your need for mobility: You may notice that your symptoms get worse if you try to stop the impulse to move.
- Maintain a sleep log: Keep a record of the tactics and medications that help you fight restless legs syndrome, and let your doctor know about them.
- Massage and stretching: Stretching and a light massage are good ways to start and end the day.
- Ask for assistance: Family members and individuals with restless legs syndrome (RLS) get together in support groups. By participating in a group, your insights can benefit both you and perhaps someone else.
Key points about Restless Legs Syndrome (RLS)
- When you have Restless Legs Syndrome (RLS), you feel a compelling need to move the affected limb.
- Although there is no surefire test to identify Restless Legs Syndrome (RLS), your doctor can make the diagnosis based on your medical history, symptoms, and physical examination.
- Changes in medication and lifestyle can help reduce the symptoms of restless legs syndrome (RLS).
- Understand why you are there and what you hope to achieve.
- Write down the questions you would like answered before your appointment.
- Remember what your healthcare practitioner tells you, ask questions, and have someone with you to help.
- During the visit, make a note of any new diagnoses, prescriptions, tests, or therapies. Take note of any instructions your physician gives you as well.
- Understand the benefits of a medication or treatment and why it is recommended. Be aware of the adverse consequences as well.
- Find out whether there are other methods to handle your circumstance.
- Understand the rationale behind a recommended test or operation and the potential consequences.
- Be aware of what to anticipate if you choose not to take the medication or undergo the test or operation.
- Note the time, date, and purpose of any follow-up appointments you may have.
- If you have any questions, know how to get in touch with your healthcare practitioner.
Restless legs syndrome in children
The same tingling and tugging feelings that adults with RLS experience in their legs can also affect children. However, they can find it difficult to explain. They may refer to it as a “creepy crawly” sensation.
A strong desire to move their legs is another symptom of RLS in children. Compared to adults, they are more prone to experience symptoms during the day.
Sleep disturbances caused by RLS can have an impact on many facets of life. A youngster with RLS may exhibit signs of fidgeting, irritability, or inattention. They could be classified as hyperactive or disruptive. Addressing these issues and raising academic achievement can be achieved through the diagnosis and treatment of RLS.
The adult criteria must be fulfilled in order to diagnose RLS in children under the age of twelve:
- strong want to move, typically accompanied by odd feelings
- The feelings get worse at night and are caused by attempting to unwind or fall asleep.
- When you move, the symptoms subside.
- The youngster must also be able to use their own words to explain the sensations in their legs.
Two of these must be true otherwise:
- Age-related sleep disruption is present.
- RLS was present in a sibling or biological parent.
- A periodic limb movement index of five or higher per hour of sleep is confirmed by a sleep study.
- It is necessary to correct any nutritional deficits. Children with RLS should learn excellent nighttime routines and abstain from caffeine.
- Benzodiazepines, anticonvulsants, and dopamine-affecting drugs may be provided if needed.
Dietary guidelines for individuals suffering from restless legs syndrome
For those who have RLS, there are no particular dietary recommendations. To make sure you’re getting enough vital vitamins and nutrients, it’s a good idea to evaluate your diet. Reduce your intake of processed foods that are high in calories but have little to no nutritional value.
Certain vitamin and mineral deficiencies are seen in certain RLS sufferers. You can take dietary supplements or alter your diet if that’s the case. It all depends on the findings of your tests.
Try increasing your intake of these iron-rich foods if you’re iron deficient:
- dark green leafy vegetables
- peas
- dried fruit
- beans
- red meat and pork
- poultry and seafood
- foods enriched with iron, such bread, pasta, and several cereals
Since vitamin C aids in the body’s absorption of iron, you may also wish to combine foods high in iron with these vitamin C sources:
- citrus juices
- grapefruit, oranges, tangerines, strawberries, kiwi, melons
- tomatoes, peppers
- broccoli, leafy greens
Caffeine is a complex substance. For some, it can exacerbate RLS symptoms, but for others, it is beneficial.
In addition to being known to interfere with sleep, alcohol can exacerbate RLS. keep away of it, especially at night.
Restless legs syndrome and sleep
You may experience pain or discomfort from those odd sensations in your legs. Additionally, it may be nearly tough to get to sleep and stay asleep with those symptoms.
Fatigue and lack of sleep are harmful to your health and wellbeing.
There are a few things you may do to increase your chances of getting a good night’s sleep in addition to consulting your doctor to find relief:
- Examine your pillows and mattress. It could be time to replace them if they are old and bumpy. Investing in cozy clothes, blankets, and sheets is also worthwhile.
- Make sure that outside light is blocked by curtains or window coverings.
- Clocks and other electronic devices should be put away from your bed.
- Clear the clutter in the bedroom.
- To prevent overheating, keep the temperature in your bedroom cool.
- Establish a sleep schedule for yourself. Even on the weekends, make an effort to go to bed and wake up at the same time every day. It will assist in maintaining a healthy sleep schedule.
- At least one hour before going to bed, stop using electronics.
- Give your legs a massage or have a hot bath or shower right before bed.
- Consider placing a pillow between your legs as you sleep. It may lessen the likelihood that your nerves would compress and cause problems.
Restless legs syndrome and pregnancy
RLS symptoms typically appear for the first time in the final trimester of pregnancy. Pregnant women may be two or three times more likely to have RLS, according to data.
This is due to poorly understood factors. Hormonal fluctuations, nerve compression, and vitamin or mineral deficits are a few potential causes.
Leg pains and trouble sleeping are other side effects of pregnancy. It can be challenging to differentiate these symptoms from RLS. Consult your physician if you suffer RLS symptoms while pregnant. Testing for iron or other deficiencies can be necessary.
Some of these home care methods are also available for you to try:
- keep away of prolonged periods of inactivity, particularly in the evening.
- Even if it’s simply a stroll in the afternoon, make an effort to get some exercise each day.
- Before you go to bed, stretch your legs or give them a massage.
- When your legs are irritating you, try applying heat or cold.
- Maintain a consistent sleep routine.
- keep away of alcohol, tobacco, caffeine, and antihistamines.
- Verify that your diet or prenatal supplements are providing you with all the nutrients you require.
- It is not safe to use some of the drugs used to treat RLS while pregnant.
During pregnancy, RLS typically resolves on its own in the weeks following delivery. Consult your physician about alternative treatments if it doesn’t. If you are nursing, make sure to mention it.
Prognosis:
Though more slowly for those with the idiopathic form of RLS than for those with a related medical illness, RLS symptoms may progressively deteriorate with age. The disease can be managed with current therapies, which reduce symptoms and lengthen sleep duration. Furthermore, some people experience remissions, which are times when their symptoms lessen or go away for a few days, weeks, or months, though they typically return in due course.
RLS is not a sign of or a portent of another neurological condition, such Parkinson’s disease. When dopamine-related medications are taken for treatment, RLS symptoms may get worse with time. This phenomenon is known as augmentation, and it may mimic symptoms that happen all day long and impair all limb movements. RLS has no known cure.
- If an underlying cause can be addressed, the symptoms of restless legs syndrome will typically go away.
- However, if the cause is not recognized, the symptoms may worsen over time and have a significant impact on the individual’s life.
- Although severe cases of restless legs syndrome can cause anxiety and sadness in addition to disrupting sleep (insomnia), the condition is rarely life-threatening.
- For those who suffer from restless legs syndrome, the charity Restless Leg Syndrome UK (RLS-UK) offers support and information.
Complications:
The disease’s own complications are restricted to affecting quality of life because of weariness and sleep disturbances. For the majority of patients, the symptoms worsen over time and significantly impair their quality of life.
Conclusion:
Before they consider seeking a diagnosis, people may be exhibiting signs of restless legs syndrome. Extreme exhaustion, irregular limb sensations, and poor sleep patterns are typically the initial signs. Although medication interventions are the first line of treatment, it has been demonstrated that modest to moderate exercise can help reduce symptoms of RLS.
It is advised to perform the various targeted, low-intensity exercises covered in this article since they offer relief from RLS symptoms without causing any negative side effects, unlike when medications are used to treat the condition.
- Legs that suffer from restless legs syndrome (RLS) feel heavy. When the legs are moved or stretched, the symptoms normally go away.
- Although the etiology of primary RLS is unknown, symptoms may be lessened with the use of both medical and home therapies.
- Entering a time of remission is another possibility. where symptoms subside over the course of weeks or months.
- An underlying condition, such as diabetes, iron deficiency, kidney illness, and others, might result in secondary RLS.
- Pregnancy can potentially result in secondary RLS.
- If you have any concerns regarding RLS, get in touch with a physician.
- In addition to ordering tests to rule out other potential reasons, they can evaluate the symptoms to help confirm the diagnosis.
FAQs
Does consuming water ease tense legs?
Dietary adjustments may also aid in lessening restless legs syndrome symptoms: keep away of stimulants like alcohol, nicotine, and coffee, especially right before bed. Keep yourself hydrated by drinking lots of water.
Which workout is ideal for restless legs?
Pilates and yoga
RLS symptoms can be soothed, stress can be decreased, and flexibility can be increased with gentle yoga and Pilates exercises. keep away of vigorous or taxing motions and concentrate on positions that encourage relaxation. Child’s pose, seated forward folds, and gentle twists are a few examples.
Which sleeping posture is ideal for people with restless legs?
How you sleep is crucial to reducing RLS symptoms, in addition to getting a new mattress. For example, resting on your back is the best option since it allows your back muscles to relax and distributes your body weight evenly.
What should I drink to calm my restless legs?
Low blood iron levels are common in people with RLS. Iron is necessary for your body to produce dopamine, a neurotransmitter that aids in motor coordination. Consult your physician about the potential benefits of taking an iron supplement. If so, to aid in the body’s absorption of the iron, take it with a glass of orange juice or another vitamin C-rich beverage.
Are you serious about restless legs?
Although severe cases of restless legs syndrome can cause anxiety and sadness in addition to disrupting sleep (insomnia), the condition is rarely life-threatening. For those who suffer from restless legs syndrome, the charity Restless Leg Syndrome UK (RLS-UK) offers support and information.
What lack results in restless legs?
A lack of iron.
RLS can be caused by or made worse by iron insufficiency, which is the body’s insufficient supply of iron. Individuals with a history of bowel or stomach bleeding may be iron deficient. Those who frequently donate blood or have heavy menstrual cycles may also be impacted by deficiencies.
Does restless leg syndrome improve with walking?
Moving may help with the syndrome’s symptoms, which tend to manifest or aggravate during periods of immobility and rest. As a result, modest exercise may be beneficial. Walking, massage, stretching, swimming, and stationary cycling are among exercises that can help reduce symptoms.
What relieves twitchy legs?
You can lessen your symptoms by engaging in relaxation-promoting practices like yoga, meditation, or other methods. This method works particularly well right before bed. Reducing alcohol and caffeine intake and quitting smoking can exacerbate RLS symptoms. You might be able to help your RLS by abstaining from these substances.
Why does restless leg syndrome occur?
The cause of restless legs syndrome (RLS) is mostly unknown. However, families of gene variations have been linked to Restless Legs Syndrome (RLS), which frequently runs in families. Restless Legs Syndrome (RLS) may potentially be caused by low brain iron levels. A malfunction in the part of your brain that regulates movement may also be linked to restless legs syndrome (RLS).
What is the onset age of restless legs syndrome?
The early-onset type can begin as early as childhood and occasionally before the ages of 40 to 45. This form’s symptoms typically get worse gradually over time. The signs and symptoms of the late-onset variety typically worsen quickly and begin after the ages of 45 to 50.
Is it mental health issues that cause restless legs?
A neurological sleep disorder known as restless legs syndrome frequently has concurrent psychiatric comorbidities (40%) with it. During sleep, patients with any mental comorbidity experienced sporadic leg movements. Patients with restless legs syndrome should be evaluated for psychiatric illnesses.
How can someone with restless legs sleep?
To keep your blood sugar stable, consume a protein snack before bed, such as beef, hard-boiled eggs, or a little amount of poultry. Restless Legs Syndrome (RLS) is caused by low blood sugar, and protein stabilizes. keep away of carbohydrates and sweets right before bed because they raise blood sugar levels and subsequently cause them to plummet.
Can restless legs be stopped by walking?
For the majority of people, regular exercise that includes aerobic and lower-body resistance training can clearly reduce the symptoms of restless legs syndrome. Pick workouts that you like, particularly those that focus on using your legs.
Which vitamin prevents the symptoms of restless legs?
Supplementing with magnesium and vitamin B6 can improve the quality of sleep and lessen the intensity of symptoms in those with restless legs syndrome (RLS).
How can my restless legs be stopped?
The limb feelings may be lessened by using heat or cold packs, or by switching between the two. Start practicing good sleep hygiene. It is crucial to maintain proper sleep hygiene because fatigue tends to exacerbate the symptoms of restless legs syndrome (RLS).
Which major factor contributes to restless legs syndrome?
The cause of Restless Legs Syndrome (RLS) is unknown in the majority of individuals. On the other hand, RLS frequently runs in families, and certain gene variations have been linked to the condition. Restless Legs Syndrome (RLS) may potentially be caused by low iron levels in the brain. Another possible cause of restless legs syndrome is a malfunction in the part of the brain that regulates movement.
References
- Dr.RaviPatel. (2023, July 29). Restless legs syndrome – Symptoms, cause, treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/restless-legs-syndrome/
- Restless legs Syndrome. (2025, February 11). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9497-restless-legs-syndrome
- Citra, W. (2024, February 23). Driving smarter to avoid neck pain. Elevate Physiotherapy. https://elevatephysio.com.sg/the-role-of-physiotherapy-in-managing-restless-leg-syndrome/
- Pietrangelo, A. (2023, June 20). Everything you need to know about Restless Legs Syndrome (RLS). Healthline. https://www.healthline.com/health/restless-leg-syndrome
- Felman, A. (2025, February 5). Everything to know about restless legs syndrome (RLS). https://www.medicalnewstoday.com/articles/7882
- Department of Health & Human Services. (n.d.). Restless legs syndrome (RLS). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/restless-legs-syndrome-rls