Proximal Interphalangeal Joint
The proximal interphalangeal joint (PIPJ) is the hand’s articulation between the proximal and middle phalanx. It is found in every digit except for the thumb.
The bending and extension of the fingers in the middle are made possible by this synovial hinge joint, which aids in fine motor control.
Introduction
The fingers’ proximal interphalangeal (PIP) joints play a crucial role in hand gripping, particularly in the so-called “power” grip. The articular surface and soft tissue of the joint, being a hinge joint, prevent lateral mobility.
Its uniaxial design permits a good range of motion, but only in one plane; for a more diverse range of motion, including adduction and abduction, it depends on the more proximal metacarpophalangeal joint.
During flexion, the ligaments that surround this joint become tense, forming a useful grasping mechanism. Consequently, the PIP joint plays a vital part in the “power grip,” which, in conjunction with the “precision grip,” allows humans to discover how to make and use tools.
Anatomy
The finger’s proximal interphalangeal (PIP) joint’s structure and function are closely linked. The PIP joint, which is far more intricate than a basic mechanical hinge, is essential to the hand and fingers’ regular operation. The relative lengths of the phalanges and metacarpals in the hand are accurately described by the Fibonacci series, as noted by Littler and Thompson. Fibonacci, also known as Leonardo of Pisa (1170–1230), defined the mathematical series where each number is equal to the sum of the two numbers before it.
When the Fibonacci sequence is applied to the hand, the length of the metacarpal is equal to the sum of the lengths of the middle and proximal phalanges, and the length of the proximal phalanx is equal to the sum of the lengths of the middle and distal phalanges. Due to these length correlations, the PIP joint is positioned in the middle of the finger, halfway between the metacarpophalangeal joint and the fingertip.
Our hands’ strength and versatility determine their utility. Due to our extreme adaptability, humans can grab items with uneven shapes. We can adapt our hands to surface imperfections. A spiral arc is followed by metacarpointerphalangeal flexion and extension. As we grip or encircle an object, the PIP joint accounts for 85% of total encompassment, while the distal interphalangeal (DIP) joint only contributes 15%.
This fact is demonstrated by the fact that DIP joint fusion is far more well tolerated in terms of finger function than PIP joint fusion. The hand’s PIP and DIP joints’ distinct architecture allows for such precisely coordinated functions.
Hard tissue
The proximal phalanx’s head and the intermediate phalanx’s base articulate to produce the PIP joint. A transversely directed apex and a lateral pit, into which the collateral ligaments are attached, are features of the head of the proximal phalanx that result in an inter-condylar concavity on the articular surface.
Two articulation-oriented concavities, separated by a saddle-shaped ridge and a tubercle for attachment to the extensor slip of the extensor expansion, are seen in the intermediate phalanx. Additionally, the distal palmar plate has an attachment site, surrounded by tiny palmar tubercles that serve as attachment points for flexor sheath and joint capsule components.
Soft tissue
The PIP joints are surrounded by several soft tissue structures that serve to both protect them and prevent undesired movement. This protective envelope’s primary constituents are the:
- Joint capsule
- Palmar (volar) plate
- Collateral ligaments (true and accessory)
- The extensor tendon hood’s central slip
Due to their malleability, the palmar plate, collateral ligaments, and extensor tendon all contribute to the joint’s increased surface area and improved joint congruence. The flexor digitorum profundus and superficialis flex the joint, whereas the extensor digitorum, lumbricals, and interossei stretch it in terms of soft tissue-producing movement. There is a synovial membrane in the PIP joint as well.
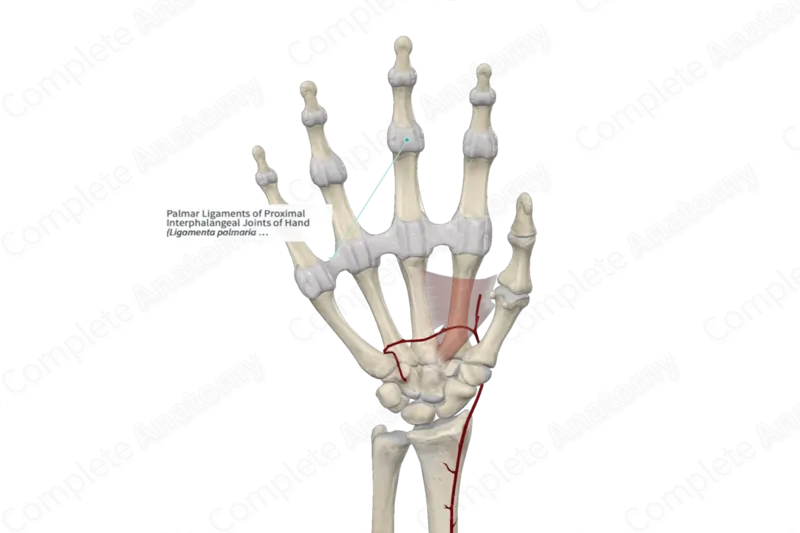
Articulating Surfaces
The articulation between the base of the middle phalanx and the head of the proximal phalanx forms the proximal interphalangeal joint:
- The head of the proximal phalanx is made up of two condylar processes that curve and create a shallow groove in the center.
- Two opposing concave portions that form an elevated ridge make up the base of the middle phalanx. This ridge offers excellent intraarticular stability and slides smoothly into the proximal groove.
Joint Capsule
Every proximal interphalangeal joint has a little fibrous capsule enclosing it. A synovial membrane lines it, and synovial fluid fills it.
Ligaments
The ligaments that surround the proximal interphalangeal joint capsule provide strength:
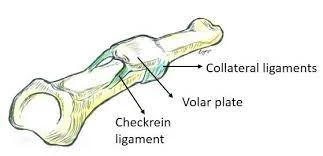
Proper and accessory collateral ligaments:
- The radial and ulnar aspects of the joint are home to the collateral ligaments. At the PIPJ, they stop over abduction and adduction.
- Along the lateral aspect of the joint, they emerge from the head of the proximal phalanx and voluntarily move onto the middle phalanx.
- An accessory collateral ligament arises from the same location as the collateral ligament and extends anteriorly to connect to the volar plate.
Volar plate:
- A thick fibrocartilaginous structure called the volar plate forms a “U”-“-shaped arch over the base of the PIPJ. It keeps the joint from being overextended.
- It attaches to the head of the proximal phalanx through the checkrein ligaments and inserts into the middle phalanx’s volar base distally.
Blood supply
The superficial palmar arch (provided by the ulnar and radial arteries) is the source of the appropriate digital arteries, which branch off to deliver blood to the proximal interphalangeal (PIP) joint of the fingers.
- Branches from the superficial palmar arch are known as common palmar digital arteries.
- The proper palmar digital arteries run along the sides of the fingers and are derived from the common palmar digital arteries.
- Branches from the dorsal metacarpal arteries (from the radial and ulnar arteries) that contribute to the dorsal aspect are known as dorsal digital arteries.
- The PIP joint is encircled by a robust vascular network that consists of both dorsal and palmar anastomoses, which guarantees adequate collateral circulation.
Movements
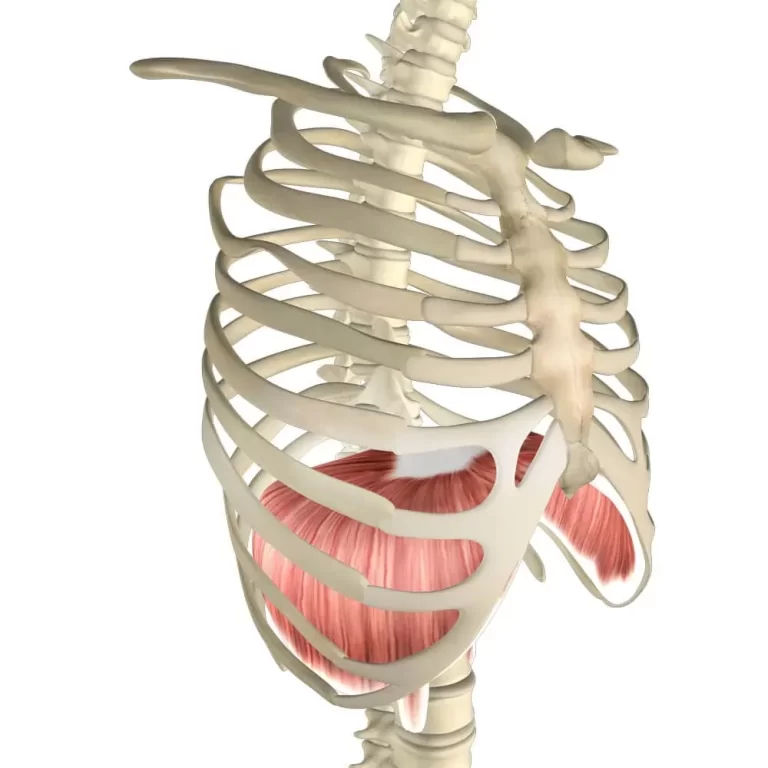
The proximal interphalangeal joint only moves in one plane, flexion, and extension, due to the nature of hinge joints and their stability.
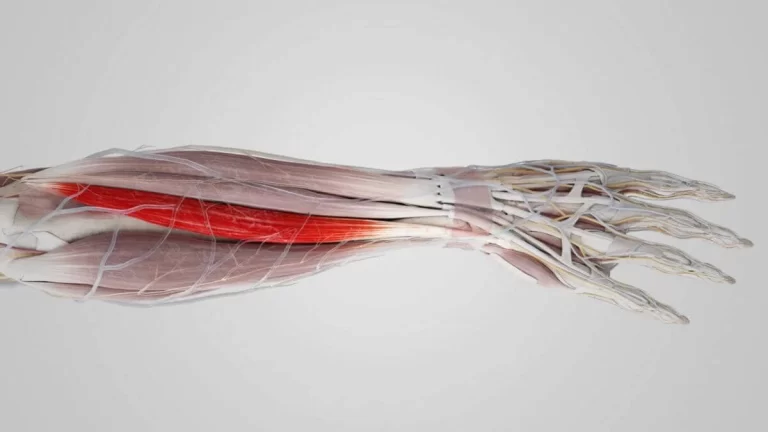
Flexion:
- The range of flexion for a healthy PIPJ is 100–110°.
- PIPJ flexion is primarily driven by the flexor digitorum superficialis muscle.
- The flexor digitorum profundus is the secondary driver of PIPJ flexion, mainly flexing the distal interphalangeal joint.
Extension:
- The interossei, lumbricals, and extensor digitorum muscles are responsible for extending back to 0°.
- Further support for the index finger PIPJ is provided by the extensor indices.
Clinical significance
An important junction in the fingers, the proximal interphalangeal (PIP) joint is situated between each finger’s proximal and middle phalanx (except the thumb, which does not have a middle phalanx). It is essential for gripping, hand function, and fine motor motions. Clinical implications of the PIP joint include the following:
1. Arthritis
- The PIP joint is frequently affected by osteoarthritis (OA), which can cause discomfort, stiffness, and abnormalities including Bouchard’s nodes.
- Rheumatoid Arthritis (RA): RA can cause swan-neck deformity, which is characterized by hyperextension of the PIP joint and bending of the distal interphalangeal [DIP] joint.
2. Injuries & Dislocations
- PIP Joint Dislocation: Hyperextension injuries, which are frequently observed in sports injuries, can cause dorsal dislocations of the PIP joint.
- Volar Plate Injury: In hyperextension injuries, the ligamentous structure known as the volar plate may sustain injury, resulting in long-term instability.
- Boutonnière Deformity: Causes PIP flexion and DIP hyperextension as a result of a central slip injury to the extensor tendon.
3. Trigger Finger (Stenosing Tenosynovitis)
- Finger locking or snapping in flexion may result from inflammation surrounding the flexor tendon sheath close to the PIP joint.
4. Dupuytren’s Contracture
- The PIP joint is frequently affected by fibrotic thickening of the palmar fascia, which causes gradual flexion contractures.
5. Mallet Finger vs. Jersey Finger
- Mallet Finger: Damage to the extensor tendon at the DIP joint that can occasionally impair the operation of the PIP joint.
- Jersey Finger: Avulsion of the FDP tendon, which affects grip strength at the PIP joint but causes loss of flexion at the DIP joint.
6. Stiffness & Contractures
- The PIP joint’s intricate ligamentous nature makes it vulnerable to post-injury contractures, which can cause post-traumatic stiffness.
- Prolonged immobility or circumstances such as spasticity in neurological illnesses can result in flexion contractures.
7. Infections
- Septic Arthritis: Failure to treat an infection in the PIP joint might result in fast joint deterioration.
- Pyogenic Flexor Tenosynovitis: Pain, edema, and reduced range of motion are symptoms of an infection in the flexor tendon sheath that indirectly affects the PIP joint.
8. Gout & Pseudogout
- Acute inflammation and pain in the PIP joint may result from the deposition of calcium pyrophosphate crystals (pseudogout) or urate crystals (gout).
9. Congenital & Developmental Disorders
- A congenital disorder known as camptodactyly causes a permanent flexion deformity of the PIP joint.
- Lateral displacement of the finger, occasionally including the PIP joint, is known as clinodactyly.
Daily activities can be greatly impacted by injuries or diseases affecting the PIP joint because it is crucial for hand function. Depending on the severity, treatment options may include physical therapy, corticosteroid injections, splinting, or surgery.
FAQs
The proximal interphalangeal joint: what is it?
The ‘power’ grip, which is a type of hand grip, depends heavily on the proximal interphalangeal (PIP) joints of the fingers. The soft tissue and articular surface of the joint, being a hinge joint, prevent any lateral movement.
Which proximal interphalangeal joint is the first?
The PIP joint, the finger’s first joint, is situated between the finger’s first two bones. The finger can bend and extend at the PIP joint. After injury, it easily becomes stiff.
At the proximal interphalangeal joint, what happens?
The hand’s articulation between the proximal and middle phalanx is known as the proximal interphalangeal joint (PIPJ). Except for the thumb, it exists in every digit. It is a synovial hinge joint that helps with fine motor control by allowing flexion and extension in the middle of the fingers.
What are the proximal interphalangeal joint’s nodes?
The symptoms of Bouchard’s nodes include inflammation and pain. Proximal interphalangeal (PIP) joints, the finger joints closest to the knuckles, are the middle joints of the fingers, and the nodes are bony enlargements of those joints. The hand’s nodes are a classic indicator of osteoarthritis or joint degeneration.
When the proximal interphalangeal joint is injured, what happens?
The following categories can be used to grade a PIP joint injury: Sprains occur when some of the fibers are torn or the ligament(s) are stretched. In a rupture, the ligament or ligaments are torn. When the ligament is ripped away from the bone, a piece of the bone is taken with it, causing an avulsion fracture.
References
- TeachMeAnatomy. (2024, October 28). The proximal interphalangeal joint – articulation – TeachMeAnatomy. https://teachmeanatomy.info/upper-limb/joints/proximal-interphalangeal/
- Proximal interphalangeal joints of the hand. (2023, November 9). Kenhub. https://www.kenhub.com/en/library/anatomy/proximal-interphalangeal-joints-of-the-hand




One Comment