Pott’s Paraplegia
What is Pott’s paraplegia?
Pott’s paraplegia, which causes severe spinal deformity, is a major complication that is challenging to cure with surgery and treatment alone. It has become accepted that chemotherapy alone can effectively cure Pott’s paraplegia in cases of early spinal TB.
The most prevalent location for musculoskeletal tuberculosis is the spine, and symptoms such as paraplegia, lower limb paralysis, and back pain are frequently associated with this condition.
Spinal tuberculosis (TB) was formerly known as “Pott’s Disease” since it was initially described by Percival Pott in 1779. One of the earliest known diseases in human history is tuberculosis (TB) of the spine, which is the common extrapulmonary type of the disease.
Spinal TB most commonly affects the lower thoracic and lumbar vertebrae, then the middle thoracic and cervical vertebrae. According to reports, 3 to 5% of instances involve the second cervical to seventh cervical localization, and atlantoaxial articulation is less frequent. The most often affected region was the lamina, which was followed by the transverse, articular, spinous, and pedicle processes.
It results in an intervertebral joint form of tuberculous arthritis. Through the intervertebral disc gap that separates two neighboring vertebrae, the infection may spread. The disc is normal if only one vertebra is impacted; however, if two vertebrae are impacted, the avascular disc collapses due to a lack of nutrients. The disc tissue dies in a condition known as caseous necrosis, which causes vertebral constriction, vertebral collapse, and eventual spinal injury. Superinfection is uncommon and a dry soft-tissue tumour usually develops instead.
One to two percent of patients with tuberculosis also have osteoarticular tuberculosis, which is invariably a secondary infection in patients who have primary tuberculosis elsewhere in the body. Pott’s paraplegia is the most severe form of bone TB. Compression of the spinal cord, progressive loss of neurologic function, and possible deformity result from the infection, which often begins from the vertebral body with visible damage and the formation of a cold abscess.
Epidemiology
Although Pott’s sickness is more common in countries with high incidences of HIV/AIDS and tuberculosis, a definitive diagnosis is still difficult to get. One to two percent of patients have osteoarticular tuberculosis, which is invariably a secondary infection in those with primary tuberculosis elsewhere in the body. While the disease is always present, in the great majority of cases (80%), it may be difficult to pinpoint the exact area of the ailment at first. One localized sign of a disease that affects the entire body is osteoarticular tuberculosis.
One-third of people worldwide contract tuberculosis (TB) as a result of the bacteria M. tuberculosis, which is primarily located in the lung. Based on data from 200 nations, the World Health Organisation (WHO) has published statistics on the prevalence and mortality rates of tuberculosis (TB) worldwide. The data shows a decline in prevalence since 1990, indicating a notable advancement in tuberculosis control.
A 2013 study that was previously completed claims that there was an almost 40% decrease in TB-related deaths between 1990 and 2010. There has been a recent rise in the number of TB cases migrating from endemic to non-endemic parts of the world, despite major efforts to avoid TB infection. The TB control tactics were complicated by the rise in unemployment, poverty, AIDS infections, and drug resistance to anti-TB chemotherapy.
Pathogenesis
Other mycobacteria that cause tuberculosis in humans include Mycobacterium microti, Mycobacterium bovis, and Mycobacterium africanum. Mycobacterium is a slow-growing, careful aerobic bacterium. The majority of these microbes are destroyed. Very few are able to live and multiply in macrophages, triggering a type IV inflammatory response that leads to the development of granulomas. Bacteria in this granuloma have the ability to lie dormant for many years.
The effectiveness of the immune response mediated by host cells determines whether an infection can be controlled or not. If there is insufficient immune response to the pathogen, mycobacterium may be able to escape from granuloma. An escaping mycobacterium can travel by hematogenous and lymphatic pathways to infect other organs, or it can create an active lung infection. Spinal involvement often occurs after hematogenous spread of infection from a source place. The genitourinary system or the lungs are the source of spinal involvement.
Since the intervertebral disc does not have its own blood supply, the infection moves from the neighboring vertebra to that location. Through the venous or arterial channel, mycobacterium reaches the highly vascular cancellous bone of the vertebral body. When the infection spreads through the vascular plexus created by the arterial arcade made up of the posterior and anterior arteries, it causes parodialysis. Blood can flow freely via the valveless Batson’s paravertebral venous plexus system, albeit this is pressure-dependent.
What are the causes of Pott’s Paraplegia?
- Mycobacterium is a slow-growing, careful aerobic bacterium. The majority of these microbes are destroyed. Few are able to endure and multiply in macrophages, resulting in a type IV inflammatory response that gives rise to granulomas.
- The degree of success of the host cell-mediated immune response determines whether an infection heals or not. If there is insufficient immune response to the pathogen, Mycobacterium may be able to escape from granuloma. An escaping mycobacterium can travel through hematogenous and lymphatic pathways to other organs, or it can create an active lung infection. Spinal involvement usually follows the hematogenous spread of infection from a primary site. The genitourinary system or the lungs is when spinal involvement begins.
- The infection spreads from the vertebra proximal to the intervertebral disc to that location since it does not have its own blood supply. Mycobacterium enters the vertebral body’s highly vascular cancellous bone through the venous or arterial channel. When infection spreads through the vascular plexus created by the arterial arcade produced by the posterior and anterior arteries, it results in parodiasal involvement. The unrestricted flow of blood via Batson’s paravertebral venous plexus system is dependent on pressure and is made possible by a valveless system.
What are the symptoms of Pott’s paraplegia?
- While there are a number of early indicators of tuberculosis, such as fever, weight loss, and night sweats, the disease can also cause significant back pain, which can make it difficult for the patient to walk and stand. Although the most prevalent symptom of Pott’s disease is severe back pain, other systemic symptoms like anorexia, fever, exhaustion, night sweats, weight loss, etc. are also frequently observed.
- Leg weakness or numbness could be caused by the infected site’s swelling. Patients with complex tubercular spine disease may exhibit deformity, instability, and pain at rest, and sometimes the primary symptom is radicular pain. A neurologic deficit is not very prevalent in Pott’s paraplegia, and the incidence varies widely depending on the stage of the disease. Therefore, paralysis of the limbs and a considerable curvature of the spine are possible outcomes of Pott’s sickness. Direct pressure from the formation of an abscess and bone sequestra may result in spinal cord involvement in Pott’s sickness.
- The main clinical features include spine abnormalities, neurological impairments, tenderness, and spasms. The patient also had sensory deficiencies, paraplegia, and nerve root pain. He even reported having trouble breathing, having trouble carrying out everyday tasks, and having bowel and bladder incontinence.
- There may be some neurological deficiency during or after the healing phase of active Pott’s paraplegia. The anterior spinal tract would get involved as a result of the TB-related vertebral collapse. Later, the lateral spinal pathways gradually become involved after the absence of the posterior column. The modified Tuli classification is the most helpful classification for Pott paraplegia with spinal cord involvement. When motor fibers are not positioned identically, as in the case of anterior spinal TB or typical Pott’s paraplegia, they are initially crushed. Consequently, the sensory fibers are only subsequently implicated.
- It appears dubious that Bosworth et al. claimed that a substance in the tubercular pus inhibits appropriate spinal cord conductivity. Regardless of whether anterior or posterior spinal TB is the cause of Pott’s illness, the degree of motor involvement that determines the degree of cord compression should be the primary criterion for classification. Motor recovery follows sensory recovery.
- At initial observation, an intraspinal tuberculous granuloma frequently presents with compressive myelopathy or a cauda equina lesion involving the sphincter. Since there is no obvious clinical spinal deformity, they are diagnosed with “spinal tumor syndrome,” which comprises both tumorous and non-tumorous diseases of the spinal cord and meninges.
Classification of Pott’s paraplegia:
- Negligible: oblivious of neurological deficiency.
- Mild: aware of the deficit but able to walk with assistance; the doctor finds plantar extensor or ankle clonus.
- Moderate: nonambulatory paralysis with a 50% sensory deficiency in extension.
- Severe: 3+flexor spasm/flexional paralysis/flaccidity, sensory impairment greater than 50% sphincter involvement.
What is the diagnostic procedure for Pott’s paraplegia?
The gold standard for diagnosing tuberculosis is mycobacterium culture; however, because this bacteria is meticulous, relying only on positive cultures for diagnosis may not be very sensitive. Additional laboratory reference standards, including hematological, immunological, microbiological, serological, and other diagnostic investigations, should be used to confirm the diagnosis. The most common method for diagnosing cold abscesses with ultrasound is MRI. Myelography plays a critical part in the diagnosis of patients who do not heal neurologically and in determining which of several skipped multifocal spinal lesions is compressing a patient.
Imaging modalities:
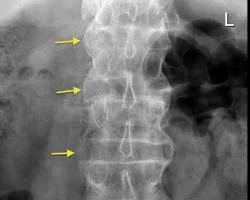
- Radiography
It was originally recommended to use plain radiographs as an imaging modality for Pott’s illness. Conventional lateral radiographs are used as a first-stage diagnostic tool to check for tuberculosis infection. Usually, diffuse osteopenia and osteolysis involving the entire vertebral body are shown on these radiographs. - CT (Computerised Tomography) scan
Computed tomography (CT) is a highly sensitive diagnostic tool that can assist far earlier than standard X-rays (100%). When Pott’s disease is present, computed tomography (CT) is a useful and often-used diagnostic technique that can clearly show the extent of soft tissue involvement. CT scans can also be used in conjunction with image-guided biopsies to aid in the diagnosing process. - Magnetic Resonance Imaging.
MRI is the most effective method of identifying the abscess site, the level of soft tissue enhancement, and spinal canal damage. In cold abscesses, MRI can also show the number of lesions and where they are located. T2 STIR pictures could guarantee the early diagnosis of inflammatory edema. - Nuclear imaging
Descriptive evidence of the activity in the affected tissues can be obtained using nuclear imaging. - Laboratory tests
There are several limitations to the serological tests. Antibody test results for IgG and IgM cannot distinguish between a person who has recovered from a natural tuberculosis infection and those who have been vaccinated against the disease. BACTEC test, Acid-fast Bacilli Staining, and Traditional TB Culture are a few common laboratory procedures. A reliable diagnosis can be obtained by isolating Mycobacterium tuberculosis by open surgical surgery or needle biopsy guided by computed tomography (CT). Hematoxylin-eosin staining of normal acid-fast bacilli is difficult to show in cases undergoing anti-TB treatment prior to surgery, and TB cultures usually have negative results in these cases. Formalin-fixed and paraffin-embedded tissue specimen blocks often exhibit a granulomatous pattern with caseating necrosis and giant-cell granuloma upon histological analysis. - Molecular diagnosis
Numerous molecular approaches are employed to achieve excellent sensitivity and specificity in diagnosis. A 75% sensitive and 97% specific polymerase chain reaction (PCR) is used to diagnose paucibacillary extrapulmonary tuberculosis infections. High sensitivity and specificity fully automated Gene Xpert MTB/RIF aid in the identification of antibiotic resistance. Histopathological tests reveal particular characteristics such as Langhans big cells, epithelioid cell granuloma, and caseating necrosis in 72% to 97% of patients. - Tests to detect latent tuberculosis
Although the skin hypersensitivity test has been promoted as an inexpensive diagnostic, people with impaired immune systems should not use it.
Treatment
- Prior to beginning Pott’s paraplegia treatment, it’s critical to assess the spinal TB disease’s severity based on presentation and symptoms. Chemotherapy or antitubercular therapy is used to treat uncomplicated cases of the disease, but chemotherapy and surgery are typically required for complex cases. There are many different kinds of surgical procedures accessible.
- The modified Tuli classification, which consists of five stages, is the most helpful classification for Pott paraplegia with spinal cord involvement. Ankle clonus, plantar or Babinski extensor, and strong tendon reflexes are all present in the first stage. The patient has spasticity and a motor impairment (UMN-type) during the second stage. Stage three sees the patient becoming bedridden and spastic. In the fourth stage, the patient develops pressure sores and a significant sensory impairment, rendering them bedridden.
- Pott’s paraplegia, which was derived from clinical and radiological state, was categorized into three groups (IA/B, II, and III). A new classification method that is easily adjusted based on the GATA system was introduced by M. Turgut et al. (2017). For aspiring spine surgeons, the updated method serves as a straightforward reference for treatment strategies for patients with Pott’s disease.
Medical treatment for Pott’s paraplegia:
The majority of antituberculous medications enter tuberculous spinal abrasions with ease. The assessment of antituberculosis medications, including pyrazinamide, isoniazid, and rifampin, was conducted on the vertebral tissues associated with spinal tuberculosis.
The lowest inhibitory concentrations of pyrazinamide and rifampin, respectively, were matched by the levels of these drugs in foci. One factor preventing the antituberculosis medication from penetrating the affected vertebra was its sclerotic bone. The result suggested that during the procedure, osseous tissues 4 mm surrounding the sclerotic wall should be removed.
Antituberculous treatment:
- The majority of patients (82–95%) with spinal TB respond extremely effectively to medical treatment, according to several studies. Pain relief, a reduction in neurological deficiency, and even the correction of spinal deformity are all clear signs of the treatment’s effectiveness.
- Medical treatment is well-received by patients with potentially serious craniovertebral junction TB. Before surgery is scheduled, patients with medically resistant spinal TB need to have their differential diagnosis carefully reevaluated.
Therapeutic regimen:
- The World Health Organisation (WHO) supports treating tuberculosis depending on categories. Under the WHO treatment categorization, spinal TB falls under the category. There are two phases to the category-1 antituberculosis treatment program: the first, or intensive phase, and the continuation phase. Four first-line medications are used in conjunction during the 2-month intense phase of antituberculous therapy: isoniazid, rifampicin, streptomycin, and pyrazinamide.
- The World Health Organisation recommends nine months of treatment for tuberculosis of the bones or joints due to the significant risk of disability and mortality as well as the challenges in evaluating treatment response.
- For adults with spinal TB, the American Thoracic Society advised chemotherapy for six months, and for children, for twelve months.
- Regardless of age, the British Thoracic Society recommends a 6-month course of daily treatment consisting of rifampicin and isoniazid, augmented in the first two months by pyrazinamide and either ethambutol or streptomycin.
- Even if six months of treatment is thought to be adequate, many specialists still recommend waiting 12 to 24 months, or until pathological or radiological evidence of disease regression is obtained. Short-term regimens and directly observed treatment may be used to prevent low compliance. With the exception of spinal arachnoiditis and spinal TB, corticosteroids have no specific function in spinal tuberculosis.
Supportive measures:
- Nowadays, ambulatory care which does not require prolonged recumbency and rest cures most patients with bone TB. Immobilization with a cast or brace was common, however it was eventually proven to be ineffective and was typically dropped.
Surgical Treatment for Pott’s Paraplegia:
- It promoted conservative care with chemotherapy that included many drugs and surgery that were saved for certain conditions.
- Nonetheless, in certain cases, surgery seems helpful and may be necessary. Fast pain alleviation, less kyphosis, instant reduction in symptoms of compressed neural tissue, a larger percentage of bony fusion, faster bony fusion, less recurrence, early return to prior normal. If fusion does not take place, it may also prevent neurological issues that arise later on due to spinal kyphosis. Pan-vertebral injury, severe kyphosis, refractory disease, a developing neurological deficit, and clinical worsening or less clinical improvement, according to one expert, should be considered reasons for surgery.
- There is no attempt made to stabilize the spine during this kind of surgery. Debridement with spinal stabilization is the second procedure. This is a more involved procedure, and bone grafts are used in the reconstructions. Fabricated materials such as titanium, steel, or carbon fiber can also be used for stabilization.
- Following substantial posterior decompression instrumented fusion and three-level posterior vertebral column resection, anterior debridement fusion with cage reconstruction is the surgical course of treatment.
- Early detection and prompt, wise surgical intervention are essential for successful treatment; the choice of surgery must be made with consideration for the patient’s age, and the antitubercular therapy’s response.
Physical Therapy Treatment for Pott’s Paraplegia:
The goals of treatment are to cure the illness and to avoid and identify any complications, such as paraplegia, as soon as possible.
Rest: Administer bed rest to alleviate pain and prevent more vertebral collapse and dislocation.

Orthoses of the spine:
- Taylor’s brace,
- Collar, and
- Minerva jacket.
Early therapy is the most crucial component of the SCI rehabilitation approach. Positioning the patient during the acute period and initiating passive, active-assisted, and active workouts early on will significantly help the patient stand up sooner and become more mobile. For these patients, standing and mobilization are not advised during the acute phase. Bracing with a conforming orthosis in conjunction with antituberculous medications has been utilized as an initial treatment for patients with spinal tuberculosis. Three months following the initial radiologic indication of bone fusion, bracing is maintained.
Early on in exercise programs, any pain that appears or becomes more intense should be closely monitored. Exercises that exacerbate pain should be avoided, and the program should be stopped if the patient has a marked increase in pain after completing the rehabilitation program. Exercise and mobilization should not wear the patient out, and they should have enough time to relax afterward. Since metabolic needs rise during illness and the rehabilitation phase, high-calorie meal plans should be implemented.
The patient’s neurologic state is taken into consideration when designing the rehabilitation program. For this reason, prior to program execution, the levels at which spinal cord damage may occur and the segments implicated are identified. Establishing a realistic and optimal rehabilitation program requires determining the region in which the lesion affects the patient’s age, concomitant diseases, urologic and neurologic status, type of paralysis, and involved area after a thorough physical and neurologic assessment.
Patients should be regularly watched after this examination to ensure proper bed hygiene, posture, and positioning during the early stages of recovery. The kind of surgical procedure used and the existence of instability are critical factors in the execution of a rehabilitation program. The prevention and monitoring of musculoskeletal issues and subsequent problems resulting from immobilization is recommended.
There are differences in the rehabilitation approach for individuals with significant neurologic abnormalities due to spinal cord compression based on their acute, subacute, and chronic stages. Even in cases when a paravertebral abscess has compressed the spinal cord, medical treatment should be tried first in cases of spinal infections. Nevertheless, when there is neurologic involvement, both surgery and medication are required.
List of problems and physical therapy techniques:
- Pain: Bilateral lower limb tenses were applied, along with frequent positioning and ergonomic guidance.
- Sensory deficiencies: Both lower limbs received sensory reeducation.
- Reduced Strength: For weak muscles, active range of motion and mildly resistant exercise training were administered.
- Issues with the respiratory system: Exercises for breathing, thoracic expansion, and autogenic drainage were imparted.
Acute stage
Determining the patient’s physical capacity is the most crucial component in determining how long acute rehabilitation will take. Muscle weakness in the lower, upper extremity, and trunk muscles might be observed in varied degrees depending on the severity of the infection. During the acute phase of flaccidity, it is crucial to perform breathing exercises, passive joint movements, and bed placement in appropriate dermatomal areas. Exercises that are isometric, passive, active-assisted, and active are used to increase muscular function. To help prevent contractures, this should be done at least once a day.
Given that contractures are most commonly seen in the shoulder, elbow, hip flexors, and ankles in the acute rehabilitation unit, these joints are the most crucial to the range of motion. The treatment of the colon, bladder, and lungs, deep vein thrombosis, gastrointestinal prophylaxis, and appropriate bed placement with rotating at least every two hours are the most crucial elements during the acute phase. The feet should be supported in a neutral position, and the trunk and extremities should be positioned correctly. Respiratory exercises are recommended if the thoracic vertebrae are affected by the spinal disease.
Every two hours, the patient is rotated from one side to the other while in the supine position to relieve pressure, and they are continuously checked for the development of erythema. By rotating from one side to the other, the patient is helped to become mobile within the bed. The lumbar, thoracic, and sacrospinal muscles are isometrically compressed in the direction of the bed in order to maintain an isometric contraction. Bilateral gluteal muscles are flexed and relaxed, while the pelvic muscular group is isometrically constricted.
Subacute stage
The time when patients are ambulating outside of bed is known as the subacute period. The goal of mobilization is to have the patient back out of bed by then using a walker or crutches, depending on the extent of the infected area. workouts on the side of the mattress must be performed actively, as well as bearing and quadriceps workouts.
In the subacute phase, workouts are done both actively and with assistance. With the feet straight up, the bilateral quadriceps muscles are lifted by about 20 cm, which contracts the hip flexors and lumbar extensors. Using the corset, the patient is assisted in sitting on the bed, either supported or unsupported. This position is used to perform balance exercises. A walker or cane is used to help the patient walk. You can repeat mobilization up to 3 or 4 times a day. When indicators of exhaustion appear, the patient should go to rest. Following the patient’s successful independent mobilization, the assistive equipment is removed.
The patient needs to drink plenty of water, stay constantly mobile, and have a urine infection checked out at specific intervals. High-fiber meals should be given to the patient in order to avoid constipation, which could be a serious issue. To encourage feces, the patient should be brought to the toilet once or twice a day. All upper extremity joints should get active strengthening activities if the upper extremities are preserved.
Chronic stage
The phrase “chronic period” refers to the time when a patient resumes his prior life and achieves maximum independence. Patients should not be near beds for this reason. It is important to provide mobilization with either independent or no support. Active and resistive activities should be included in lying down, sitting, and standing exercises. Lifting-related exercises such as squatting, sitting on the ground, and climbing stairs should be performed.
Exercises include forward flexion-extension, backward, and sideways stepping, as well as neutral position exercises, which are done in a standing position. Dorsal and abdominal muscles are strengthened by the use of cat and camel stretching exercises.
Patients with paraplegia may experience special health issues called decubitus ulcers. individuals with spinal cord compression may experience depression; consequently, psychological help should be given to these individuals.
Home exercise program
A capacity-based home exercise program ought to be created in a language that the patient can comprehend. To enable patients to return home after rehabilitation, a home evaluation is a crucial step in the process. The bedroom, kitchen, bathroom, and entryways are the primary areas of concern in the home evaluation, along with general safety concerns.
To ensure patient independence, the patient’s home environment (toilet, bathroom, bedroom, hallway, etc.) should undergo the greatest amount of ergonomic modifications. Regular evaluations of patients’ overall status and check-ups are necessary. When the patient is close to being able to resume employment, specific recommendations should be made to help with everyday life activities.
Following the conclusion of the hospital’s rehabilitation program, the patient is sent home with an exercise regimen and scheduled follow-up visits. Hand and wrist joint exercises, complete abduction, extension, and flexion exercises for the abdominal, sacrospinal, iliopsoas, gluteus maximus, gluteus minimus, hamstring, and quadriceps muscles, and resistive exercises for the oblique abdominal muscles are advised to be done at home in addition to the exercises done during the subacute and chronic stages.
There are exercises that improve breathing capacity. Exercises for cardiovascular endurance are recommended following the complete healing of the vertebrae. The existence of neurological findings led to the recommendation of a rehabilitation program. During the follow-up appointments, a neurologic examination and laboratory testing are performed. In addition to infectious infections, pulmonary disorders are treated using a multidisciplinary follow-up program.
When we examined motor scores for lower limbs and modified Barthel index (MBI), we found significant improvements in the discharge scores of the patients with tuberculosis and brucella following their admission to the hospital. Patients in the program reported minimal pain and an improvement in their ability to carry out their daily tasks by the end of the rehabilitation.
Degenerative modifications at the pathologic disc space were observed to be smaller than expected in all patients’ final radiological tests. After Yen et al. assessed MBI, they found that patients’ discharge ratings significantly improved in comparison to their admission scores. In terms of the lower limb motor scores, they also discovered a noteworthy improvement in the discharge ratings of the same individuals.
What are the complications of Pott’s paraplegia?
A specific amount of time is spent in bed for patients with spinal infections; this time is extended for those with neurologic impairments or those who were advised to have surgery. These patients need to be thoroughly monitored for any problems and given the appropriate care. Morbidity and mortality are increased when problems like depression, osteoporosis, spasticity, contractures, decubitus ulcers, lung infections, hypertension, hypotension, deep vein thrombosis, urine retention, and infections are not identified and treated. The prolonged length of immobilization results in a higher frequency of complications and a delayed response to treatment.
Conclusion:
Anyone who can treat tuberculosis may also treat spinal tuberculosis. While the treating surgeon assumes the majority of the patient care responsibility, the contributions of health service professionals at all levels are critical to the management of Pott’s paraplegia.
Orthopedic surgeons are usually needed when there is a neurological defect or impairment. The next specific step is to assess the effects of the disease and make an informed decision about whether surgery and long-term treatment are required. The challenges of long-term chemotherapy management, including drug side effects and consequences, noncompliance issues, socioeconomic factors, and others, are also crucial.
FAQs
Can a TB paralysis be healed?
It can lessen impairment and reverse paralysis. For most patients, a combination of conservative care and surgical decompression results in success.
What is the duration of paraplegia?
Some persons may be able to regain some function up to eighteen months following their accident. Many, however, will suffer from a permanent loss of function necessitating long-term care.
What is TB spine late-onset paraplegia?
A well-known condition in old-healed spinal TB is late-onset paraplegia, which can be caused by a bony ridge transposing the cord or by fibrous tissue or granulation constricting the chord.
Can Pott’s disease be cured?
Pott’s illness can be managed with surgery or a strict drug regimen. Pott’s Disease is caused by long-term neglect; on the other hand, a protracted drug regimen is usually required to completely cure the disease.
What is the prognosis for Pott’s disease?
Antitubercular therapy is an effective treatment for Pott’s disease. Neurological impairments and pain improvement are markers of treatment response. All patients have a fair prognosis; however, if progress is not maintained, another differential diagnosis needs to be made.
How long does spinal tuberculosis last?
Spinal tuberculosis progresses slowly and stealthily. The average length of the disease ranges from 4 to 11 months, while the overall duration of the illness varies from a few months to a few years. Patients typically only consult a doctor when they have a noticeable deformity, excruciating pain, or neurological issues.
Is Pott’s disease a serious one?
Since Pott disease can induce bone loss, deformity, and paraplegia, it is the most serious type of musculoskeletal TB. Most frequently, the thoracic and lumbosacral spines are affected by Pott illness. Published series have, nevertheless, demonstrated some variance.
Can TB in the spine result in paraplegia?
In the active stage of spinal TB, early-onset paraplegia occurs and necessitates therapy. This kind of paraplegia is more common in adults with Pott’s spine and has a better prognosis.
References
- Mehta, Y. (2022b, December 14). Pott’s Paraplegia – Cause, Symptoms, Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/potts-paraplegia/
- Ahmed, N., Khan, M. S. I., & Ahsan, M. K. (2022). Pott’s Paraplegia. In IntechOpen eBooks. https://doi.org/10.5772/intechopen.107851