Posterior Tibial Tendonitis
Posterior Tibial Tendonitis: What is it?
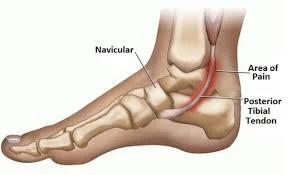
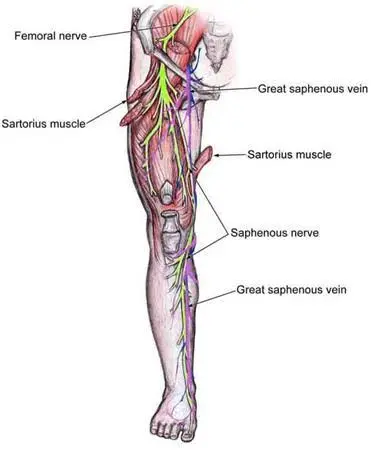
Posterior tibial tendonitis is inflammation of the posterior tibial tendon, which supports your foot’s arch and allows it to bend. It’s also known as your posterior tibialis tendon.
Tendons are thick, rope-like connective structures that link muscles and bones. The posterior tibial tendon connects one of your lower leg muscles to the bones inside your foot and ankle.
When this tendon is inflamed, you may experience pain and soreness around the arch or inside of your foot and ankle. Tendonitis is a type of inflammation that can be either acute or chronic.
Long-term posterior tibial tendinitis can cause the tendon to degrade and weaken. This is known as tendinosis. Posterior tibial tendinosis can cause posterior tibial tendon dysfunction (PTTD).
Causes of Posterior Tibial Tendonitis :
Posterior tibial tendonitis might be caused by:
- Overuse or high-stress repeated motions of the ankle.
- Low foot muscle strength and flexibility
- Having Flat Feet
- Injury of the foot, ankle, or leg
The following activities may increase your chances of sustaining a posterior tibial tendon injury:
- Jumping
- Running, particularly up and down hills or long distances
- High-impact sports, including football
Symptoms of Posterior Tibial Tendonitis:
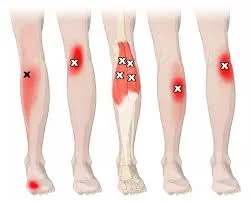
Most typically, persons with posterior tibial tendonitis experience:
- The posterior inside of the ankle is painful or sensitive and can become swollen.
- Pain is felt while standing on the ball of the foot, flexing the foot, or moving the ankle.
- The tendon may generate a snapping sound.
They could also have:
- Weakness while attempting to point their toes inward.
- They have trouble standing on their toes on the affected side.
Many patients with this illness have experienced a recent ankle sprain. Some, however, will not have been injured recently. Overuse can potentially cause injury to the tendon.
Diagnosis:
A podiatrist (a specialist who specializes in foot and ankle disorders) or an orthopedic physician can diagnose posterior tibial tendonitis through a physical examination.
If the examination is unclear or your doctor is considering surgical repair, they may request an MRI scan. The MRI can detect whether and where the tendon has ruptured. It can also indicate inflammation around the tendon.
Stages
Posterior tibial tendonitis is defined by stage. Stages 1–4 indicate growing deformity (abnormal shape) of the foot as the disorder proceeds.
- Stage 1: The initial stage involves pain and swelling along the tendon. The foot may seem entirely normal. However, some people may realize that their foot has a slight flatfoot deformity. This may be something they believe they have always had.
- Stage 2: As the illness advances, the foot arch begins to collapse. When they stand, the foot appears flat on the inner side. People may interpret it as a simple sensation of weakness in the arch. At this point, the flattened arch may be repairable.
- Stage 3: The illness, known as a rigid flatfoot deformity, has advanced to the point where the foot deformity is permanent (rigid).
- Stage 4: In this most severe stage, the deltoid ligament on the inside of the ankle collapses, resulting in an ankle deformity as well as a foot deformity. Ankle arthritis (cartilage wear) may also occur.
Treatment of Posterior Tibial Tendonitis:
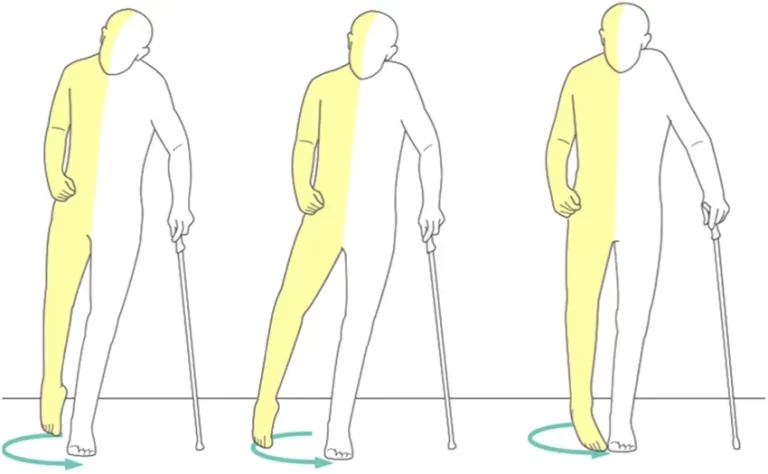
Treatment for posterior tibial tendonitis is determined by its stage. It generally starts with rest and non-surgical therapy. Later on, surgery may be required.
Early Treatment.
The first step in treating posterior tibial tendonitis is to minimize inflammation and stabilize the foot using physical therapy and orthotics. Rest may also be beneficial, although stopping all walking is not recommended as a first-line therapy unless the symptoms are severe.
Early therapy options include:
- Applying ice can help minimize swelling.
- Anti-inflammatory medicines can help decrease inflammation surrounding the tendon.
- Orthotics (shoe inserts, arch supports) limit mobility between the center and rear of the foot, reducing irritation.
- Walking boots and casts can help reduce inflammation.
- Limiting exercise allows the tendon to rest and reduces inflammation around it.
- Physical therapy might involve stretching and strengthening exercises, as well as massage.
According to research, kinesiotaping can assist in minimizing the incorrect movement of a functioning posterior tibial tendon while increasing tibialis anterior muscle activation in the lower leg.
Physical Therapy for Posterior Tibial Tendonitis:
Ankle-toe movement
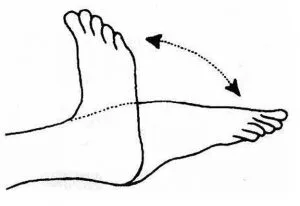
- Begin by lying down on the bed in a comfortable posture.
- Bend your toes as near to your body as possible.
- Hold your position for a few seconds.
- Then Rest.
- Repeat five to ten times.
Ankle inversion
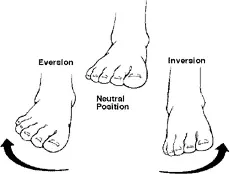
- A chair should enable your feet to touch the ground.
- Place your wounded foot over the other leg, resting on your thigh, while the unaffected leg remains flat on the floor.
- Make a long loop out of the band, tying one end around the inside of the affected foot and the other beneath the foot on the floor.
- Lift the affected foot inward and spin it against the band’s resistance.
- Hold your position for a few seconds.
- Then, return to the neutral position.
- Then rest.
- Repeat the exercise five to 10 times.
Ankle inversion with ball.

- A ball is put between two feet.
- Try to bring your feet closer together by gently pushing your toes into the ball.
- Repeat for the stated number of times.
- Repeat many times, holding for a few seconds each time.
- Then, return to the neutral position.
- Then rest.
- Repeat the exercise 5 to 10 times.
Side-lying leg lift

- Lie down on your right side on the floor or a mat.
- With your feet on top of each other and your legs extended, your body should be in a straight line.
- Either position your arm straight on the floor beneath your head for support or hold it with your elbow bent.
- For further support, place your left hand on your leg or hip, or extend it out in front of you.
- Lift your left leg off the bottom leg as you release the breath.
- Maintain this posture for a little while.
- Stop lifting your leg as soon as it feels constricted.
- After taking a breath, contact the right leg by lowering the leg again.
- Then rest.
- Five to ten times, repeat the procedure.
Towel stretch

- Sitting on the floor or your bed, extend your legs in front of you.
- Use the towel to round out the middle of your foot, just below your toes.
- Gently pull the towel, allowing your foot to slowly bend up towards it while maintaining a straight knee.
- There should be a slight stretch at the back of your lower leg.
- You may feel the stretch below your heel or beneath your knee, depending on which area of the muscle or tendon is stiff.
- Maintain this posture for a little while.
- Then, slowly relax the strain.
- Then return to your neutral position.
- Calm down.
- Five to ten times, repeat this practice.
Prone leg raise

- Place yourself face down on the ground.
- While maintaining the involvement of your abdominal muscles, gradually tighten your core muscles.
- Your respiration should remain Completely while you do this.
- While keeping your knees straight and your abs straight, slowly elevate one leg backward.
- Keep your knee straight as your leg lifts off the floor.
- Hold your leg straight up in the air for a few seconds, then slowly return to the ground.
- Then unwind.
- Be careful not to twist your back or pelvis when raising your leg.
- Five to ten times, repeat this practice.
Heel raise
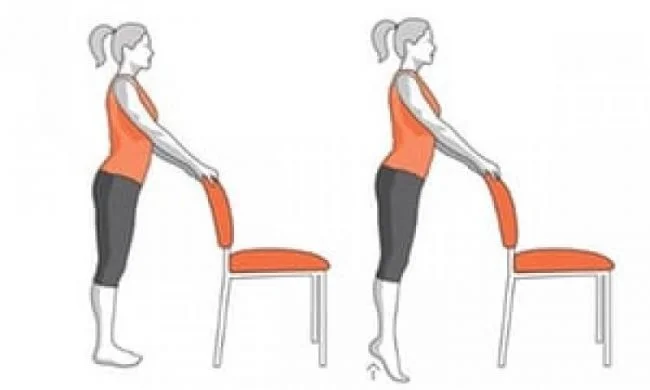
- Take a comfortable standing position to start.
- For support, lean against a wall or grip the back of a chair.
- Raise both heels off the floor to put yourself on the heels of your feet.
- Maintain this position for a brief period.
- To get into the starting position, drop your heels.
- After that, relax.
- You should perform this workout five or ten times.
Step-up

- To start this exercise, you’ll need a step stool.
- Now, place your injured foot on a support that is three to five inches (8 to 13 cm) high, such a small step or wooden block.
- Place the usual foot on the ground gently.
- Use the support and place your weight on the damaged leg.
- Extend the affected leg once the other leg rises off the ground.
- To get your normal leg back to the starting position, bend the affected leg and gradually lower it down to the ground.
- Then rest.
- You should perform this workout five or ten times.
Forward Step Downs
- To begin, place both feet on a box or step.
- Slowly move the unaffected leg down and away from the box or step until it makes light contact with the floor.
- Maintain this posture for a little while.
- Next, use both feet on the step or box to get back to the beginning position.
- Then unwind.
- Five to ten times, repeat this practice.
Surgical Options
The surgical treatment of posterior tibial tendonitis is controversial. Surgical options depend on the severity of the problem and include:
Debridement: In the early stages, some surgeons may propose a surgery to clear the inflammation. Debridement involves the removal of inflammatory tissue and aberrant tendon. This promotes the repair of the injured tendon.
Reconstruction: In more advanced stages, the foot arch collapses, and your doctor may perform surgery to restore the region. This include transplanting a healthy tendon or segment of a tendon from another region of the body to replace the injured posterior tibial tendon. Calcaneal osteotomy is a procedure that involves breaking and reshaping bones in the foot or heel to rectify a deformity.
Finally, in the most severe cases, when the foot’s arch has grown inflexible, doctors frequently recommend a fusion treatment in which the bones and joints of the foot are put in place to restore the arch.
Prevention of Posterior Tibial Tendonitis:
To decrease your risk of posterior tibial tendonitis:
- Before engaging in physical exercise, make sure to warm up and stretch properly.
- You should wear arch supports.
- Take it gently while starting new hobbies.
- Learn the proper skills for playing your sport.
- Rest when you’re fatigued or in pain.
When to See a Doctor
- If you have the symptoms listed above, you should consult your doctor.
- If not addressed, posterior tibial tendon dysfunction might worsen over time.
- As the illness advances, the arch of the foot flattens, causing additional pain.
- A flattened arch may also strain the ligaments inside the ankle and misalign the joints, resulting in ankle arthritis.
Summary
Posterior tibial tendonitis causes pain on the inside of the foot and ankle. It may create instability when walking. Adult-acquired flatfoot deformity (AAFD) is a disorder that occurs when the arches flatten with time.
This issue will be diagnosed by your healthcare professional using a physical exam and imaging methods. It is preferable to treat the problem at an early stage. The severity of the illness determines the appropriate treatment. Orthotics and physical therapy are typical first-line therapies. When the condition progresses to the latter stages, surgery is typically required, and you may lose some foot function.
FAQs
What is the fourth stage of posterior tibial tendonitis?
This is the most advanced stage, and it includes a hindfoot valgus deformity caused by posterior tibial tendon degeneration, as well as valgus tilting of the talus inside the mortise.
Should I massage the posterior tibial tendonitis?
However, don’t massage directly on the aching tendon, even if it feels good in the short term. Again, compression on the wounded tendon frequently exacerbates the problem. Instead, use a massage ball or foam roller to massage your calf muscles while avoiding uncomfortable regions.
What type of doctor manages posterior tibial tendonitis?
It is enough for an orthopedic specialist to diagnose posterior tibial tendonitis and suggest therapy to relieve your pain successfully.
What happens if posterior tibial tendinitis remains untreated?
Adult-acquired flatfoot deformity (AAFD) is a disorder that occurs when the arches flatten with time. This issue will be diagnosed by your healthcare professional using a physical exam and imaging methods. It is preferable to treat the problem at an early stage.
Does tibial tendinitis ever go away?
Early detection and management are critical to halting its development. The early stages of posterior tibialis tendinitis are commonly treated non-surgically. However, if not treated, posterior tibialis tendon dysfunction would increase and lead to serious problems requiring surgery.
How to strengthen the tibialis muscles?
Toe raises (sitting or standing), heel walks, dorsiflexion pulls with band resistance, and calf stretches are all useful exercises for strengthening the anterior tibialis muscle. These workouts specifically target the anterior tibialis muscle, which can help enhance its strength and endurance over time.
What is the discomfort level of posterior tibial tendonitis?
Common characteristics. Most people will feel discomfort after resting and first thing in the morning, particularly on the inside of the ankle of the foot, as well as after strenuous exercise such as walking. People frequently feel that they are walking ‘heavily’ and have no bounce in their step.
Can I ride a bicycle if I have posterior tibial tendonitis?
It is tough to exercise and raise energy expenditure to lose weight while your foot is in pain, but there are various safe sports you may try, such as stationary cycling or swimming.
References
- Posterior tibial tendonitis and posterior tibial tendon dysfunction. (2025, March 18). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/posterior-tibial-tendonitis-posterior-tibial-tendon-dysfunction
- Cluett, J., MD. (2025, March 21). Posterior tibial tendonitis symptoms and treatment. Verywell Health. https://www.verywellhealth.com/posterior-tibial-tendonitis-2548561
- Posterior tibial tendonitis Signs & Treatment | Columbus, OH. (n.d.). OrthoNeuro. https://orthoneuro.com/foot-ankle-podiatry/posterior-tibial-tendonitis/