Plantar Fascia Tear
Introduction:
A partial or whole rupture of the plantar fascia, a thick band of connective tissue on the sole of the foot, is referred to as a plantar fascia tear. Numerous things, such as excessive use, unexpected impact, or pre-existing disorders like plantar fasciitis, can cause this tear.
Sharp and frequently severe heel pain can result from a tear in the plantar fascia, especially when standing, walking, or running activities that put stress on the foot. Swelling, tenderness, stiffness, and pain when flexing or pointing the toes are possible additional symptoms.
Depending on the extent of the tear and the underlying causes, plantar fascia tears can range in severity. A physical examination, a review of the patient’s medical history, and occasionally imaging tests like an MRI or ultrasound.
What is a Plantar Fascia Tear?
Although they are rare, plantar fascia tears can coexist with plantar fasciitis. Plantar fascia tears usually occur after a stressful event, like stepping on something or being hit by a sudden force that puts tension on the plantar fascia.
When they first get out of bed, people with plantar fascia tears, also called plantar fasciitis, typically have a sore heel and pain that goes away with some walking but comes back with more walking.
A tear in the context of the plantar fascia is defined as a rupture or disruption of the tissue fibers caused by tension or damage. The size of tears can range from tiny microtears to more extensive ruptures.
Larger tears can result in severe pain, edema, and restricted movement, whereas smaller tears may just cause slight pain. The plantar fascia may even burst completely as a result of severe injuries.
Anatomy of Plantar Fascia:
The plantar fascia, sometimes referred to as the plantar aponeurosis, is a robust connective tissue aponeurosis that supports the plantar side, or bottom, arch of the foot. According to recent studies, the plantar fascia is not a true fascia but rather an aponeurosis. From the calcaneus tuberosity (heel bone), it travels to the heads of the metatarsal bones, which are the bones between each toe and the bones of the midfoot.
- The plantar fascia then stretches forward in the direction of the toes.
- The thick core tissue that envelops the plantar muscles is called the plantar fascia.
- As the flexor tendons go to the toes, they are surrounded by fibrous sheaths, and the plantar fascia becomes continuous distally. At the anterior extremity of the sole, beneath the metatarsal heads, the plantar aponeurosis forms the superficial transverse metatarsal ligament.
Mechanism of injury of Plantar Fascia Tear:
Plantar fascia tears are frequently caused by abrupt or repetitive stress that is greater than the tissue’s ability to tolerate strain. This tear can be caused by a number of factors, including:
- Overuse: Running, jumping, and standing on hard surfaces are examples of prolonged, repetitive exercises that can progressively compromise the plantar fascia.
- Sudden Impact: The plantar fascia may tear as a result of an abrupt and powerful impact to the heel, such as that which occurs during a fall or an improper landing.
- Excessive Force: The plantar fascia may sustain a tear as a result of activities that require abrupt direction changes, pivoting, or accelerating.
- Improper Footwear: Wearing shoes that don’t provide enough arch support or cushioning can lead to an uneven force distribution on the plantar fascia, which increases the likelihood that it will tear.
- Changes in activity Level: Without adequate training, abruptly increasing the frequency, duration, or intensity of physical exercise can cause tears and stretch the plantar fascia.
- Structural Factors: Foot deformities such as flat feet or high arches can change how the foot moves, putting the plantar fascia under unequal stress and raising the possibility of a tear.
- Tight Muscles: Tight Achilles tendons or calf muscles can put additional strain on the plantar fascia, increasing its susceptibility to tears.
- Age: As people age, their plantar fascia may become less flexible and strong, which raises their risk of injury.
- Pre-existing Conditions: The plantar fascia might become weaker and more prone to tears if you have plantar fasciitis or other foot issues.
- Obesity: Carrying too much weight increases the strain on the plantar fascia and raises the risk of injury.
Depending on the person’s activity, foot structure, and other influencing factors, the mechanism of damage may change.
Causes of Plantar Fascia Tear:
- Overuse: Over time, little tears in the tissue may result from repetitive strain and overuse of the plantar fascia, which is frequently caused by activities involving a lot of running, leaping, or standing.
- Age: As people age, their plantar fascia may become less flexible and weaker, which raises their risk of injury.
- Tight Calf Muscles: The plantar fascia may be subjected to extra strain from tight calf muscles, which increases the likelihood of tears.
- Obesity: Carrying too much weight can put more strain on the plantar fascia, increasing its susceptibility to ripping.
- Structural Factors: Unusual foot arches, such as high arches or flat feet, might cause the plantar fascia to be improperly distributed, which raises the possibility of tears.
- Insufficient Warm-Up: Physical activity without appropriate warm-up exercises might raise the risk of injury, including tears in the plantar fascia.
- Pre-existing disorders: Some disorders, such as inflammation of the plantar fascia, or plantar fasciitis, can weaken the tissue and increase its vulnerability to tears.
- Biomechanical Problems: Excessive inward rolling of the foot, or overpronation, or supination, are examples of abnormal foot mechanics that can put more strain on the plantar fascia.
Symptoms of Plantar Fascia Tear:
- Sharp Heel Pain: A sharp, stabbing pain in the heel’s bottom is the defining sign. When you first get out of bed in the morning or after resting for a while, this pain usually gets worse. Additionally, it could get worse after standing or doing something for extended periods of time.
- Localized Tenderness: The calcaneus, the region where the plantar fascia connects to the heel bone, becomes sensitive to the touch.
- Swelling: Inflammation and irritation of the damaged tissue may cause the affected area to swell. After extended activity, swelling may become more apparent and contribute to pain.
- Walking and other weight-bearing activities may make this pain more noticeable.
- Pain Progression: If treatment is not received, the pain may gradually get worse and become more persistent. Your everyday activities and quality of life can begin to suffer as a result.
- Reduced Range of Motion: Some people with a tear in their plantar fascia may find that they cannot flex and point their toes as much, which can impact their movement and gait.
Risk Factors of Plantar Fascia Tear:
The chance of sustaining a plantar fascia tear can be increased by many risk factors. These consist of:
- Physical Activity: Running, jumping, and dancing are examples of high-impact exercises that can repeatedly strain the plantar fascia and increase its risk of tears.
- Inappropriate Footwear: Wearing shoes with inadequate arch support or cushioning might increase the risk of injury, particularly when engaging in activities requiring extended standing or walking.
- Obesity: Carrying too much weight puts additional tension on the plantar fascia, making tears and other injuries more likely.
- Foot Structure: A person’s plantar fascia is more susceptible to tears if they have flat feet, high arches, or other structural abnormalities that change how weight is transferred across the foot.
- Sudden Increase in exercise: Without adequate training, abruptly increasing the frequency, duration, or intensity of physical exercise can cause tears and stretch the plantar fascia.
- Occupational Factors: Plantar fascia tears may develop as a result of work requiring extended standing or hard surface walking.
- Previous Foot Injuries: If you’ve had previous foot injuries or conditions like plantar fasciitis, your plantar fascia can already be weakened, making it more prone to tears.
- Inadequate Warm-up or Stretching: The risk of injury can be increased by skipping warm-up activities or failing to stretch the plantar fascia and calf muscles before physical activity.
- Genetics: Your likelihood of having tears may be influenced by specific hereditary variables that affect the strength and shape of your plantar fascia.
Differential diagnosis:
Differential diagnosis is the process of determining and differentiating between conditions that may cause heel pain and associated symptoms.
- Plantar Fasciitis: Inflammation of the plantar fascia, commonly caused by recurrent stress, is known as plantar fasciitis.
- Heel Spurs: These are bony growths that can form on the heel bone owing to persistent plantar fasciitis. They might make soreness and heel pain worse.
- Achilles Tendonitis: Because the pain is so close together, it can occasionally be confused with problems with the plantar fascia.
- Stress Fractures.
- Tarsal Tunnel Syndrome.
- Nerve Entrapment: Disorders such as Baxter’s neuritis cause localized pain by trapping nerves in the foot.
- Calcaneal Bursitis.
- Fat Pad Atrophy: Because there is less cushioning as the heel’s fat pad thins, pain may result.
- Gout and rheumatoid arthritis.
- Nerve Impingement.
- Ankle Instability: Chronic ankle instability can result in poor foot mechanics, which can worsen heel pain.
To correctly diagnose the underlying condition, a thorough evaluation of medical history, physical examination, and occasionally imaging tests like X-rays, ultrasounds, or MRIs is required for proper differential diagnosis.
Diagnosis of Plantar Fascia Tear:
A clinical evaluation, a review of the patient’s medical history, and occasionally imaging studies are used to diagnose a plantar fascia rupture.
- Review of Medical History: Your doctor will inquire about your symptoms, such as the type and length of your heel pain, any recent injuries or activities that may have caused it, and your medical background.
- Your physician will check for bruising, pain, edema, and altered foot mechanics.
- Palpation: To determine the location of pain and gauge tenderness, your healthcare professional may apply pressure to various foot parts. It may be especially instructive to palpate the attachment sites of the plantar fascia.
- Clinical Tests: A plantar fascia tear can be confirmed by a number of clinical tests. The “Windlass Test,” which applies pressure to the toes to stretch the fascia and replicate pain, may be one of them.
- Functional Movement Assessment: To evaluate your gait and foot mechanics, the physical therapist watches you walk, stand, and carry out particular motions.
- Examining your foot alignment and posture, as well as measuring things like arch height, can give you hints about how well your plantar fascia is doing.
- Evaluation of Calf Muscle Length: The physical therapist measures the calf muscles’ range of motion.
Imaging studies: To determine the degree of the tear and confirm the diagnosis, imaging studies may occasionally be advised. Typical imaging techniques consist of:
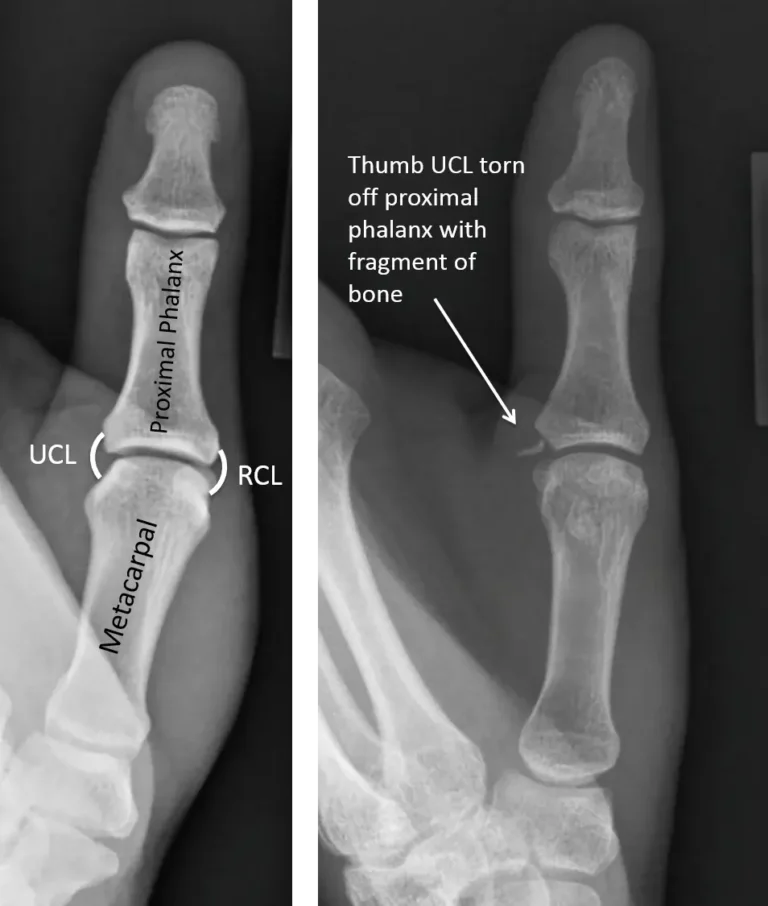
- X-rays: Although they cannot directly view soft tissues like the plantar fascia, X-rays can be used to rule out other disorders, such as heel spurs or fractures.
- Ultrasound: This imaging technique can detect tears, inflammation, and changes in thickness while visualizing soft tissues such as the plantar fascia. Additionally, there are isolated areas of fiber disruption, where bleeding has caused the fibers to separate and expand.
- On some of the more sophisticated MRI sequences, however, we see a very bright signal that is more suggestive of a tear than plantar fasciitis. This strong signal also flows to the heel and soft tissues, signifying bleeding and edema.
Classification:
- Grade I (Mild Tear): Particularly when exercising, it may be irritated and produce slight pain. Although there may be some swelling and pain, the fascia’s fundamental structural integrity is preserved.
- Grade II (Partial tear): Moderate to severe pain may ensue, particularly when engaging in weight-bearing activities.
- Grade III (Complete tear) occurs when the plantar fascia ruptures completely, causing the tissue to be completely torn. Severe pain and functional disability may result from this. The foot’s capacity to move and support weight may be seriously impaired. Bruising and swelling may also be more obvious.
The classification provides a sense of the severity of the tear and aids in guiding treatment recommendations. More structured therapies, like immobilization, orthotics, and sometimes corticosteroid injections, may be necessary for partial tears. More extensive therapies, including immobilization, physical therapy, and perhaps surgical repair, may be required for complete tears.
Special tests:
To determine whether plantar fascia tears or related issues are present, physical therapy practitioners employ a number of specialized examinations. These tests aid in the diagnosis and creation of a suitable treatment strategy.
- Plantar Fascia Palpation: Your doctor will press and feel along the plantar fascia to feel for any sensitive spots, swollen areas, or texture changes that could be signs of a tear.
- Windlass Test: In this test, the foot is passively plantarflexed (pointed) while the toes are dorsiflexed, or pulled towards the shin. Reproducing pain in the plantar fascia region may indicate an inflammation or tear.
- The Silfverskiöld Test: It can be useful to discover tightness that may affect the plantar fascia by performing a calf stretch with your knee straight and then bent.
- Thompson Test: This test evaluates the Achilles tendon’s integrity, even though it has nothing to do with the plantar fascia. It entails applying pressure to the calf while watching for movement in the foot. It may be a sign of an Achilles tendon rupture if the foot remains immobile (no plantarflexion) when the calf is squeezed.
- Plantar Fascia Tension Test: This test stretches the plantar fascia by passively flexing the toes. Inflammation or a tear may be indicated if pain is felt in the fascial area.
- Heel Drop Test: To stretch the calf muscles, the patient lowers their heels while standing on a stair or other raised surface.
- The Navicular Drop Test: The plantar fascia may be experiencing biomechanical problems if there is an excessive navicular drop, or lowering of the arch, when moving from a seated to a standing position.
- Toe Flexor Endurance Test: The patient does toe flexion exercises until they become tired, such as using their toes to pick up marbles. The strength and stamina of the intrinsic foot muscles that influence the plantar fascia can be determined by this test.
- Arch Compression Test: The foot’s medial arch is compressed. Involvement of the plantar fascia may be indicated by pain during this compression.
Treatment of Plantar Fascia Tear:
Medical Treatment:
- Ice: Applying ice to the affected area may help reduce pain and inflammation.
- Orthotics and Supportive Footwear: Custom-made or store-bought orthotic inserts help ease plantar fascia strain by supporting and cushioning the arch. Cushioned, supportive shoes can lessen strain while doing daily tasks.
- Brace or Splint: To support and stop the foot from moving, a brace or splint may be utilized. While providing some flexibility for healing, these devices can aid in stabilizing the wounded area.
- Walking Boot: For plantar fascia sprains, a walking boot is frequently used. As healing advances, it permits moderate weight-bearing and provides superior support compared to a brace. To account for variations in edema, walking boots can be adjusted and may have detachable insoles.
- Night Splints: By keeping the plantar fascia stretched while you sleep, a night splint helps lessen morning pain.
- Corticosteroid Injections: In order to lessen pain and inflammation, medical professionals may occasionally advise corticosteroid injections. Due to possible hazards and adverse effects, these injections should be used with caution and are often not a first-line treatment.
Surgical Treatment:
When conservative measures have failed to relieve a plantar fascia tear and the tear is substantial or significantly impairing function, surgery is typically recommended. Usually used as a last resort, surgery is saved for situations in which non-surgical methods have failed to reduce pain and restore normal foot function.
Plantar Fascia Repair: To encourage healing and restore the tissue’s functional integrity, this entails reattaching it.
Open Plantar Fasciotomy: An incision is created on the bottom of the foot, close to the heel, during an open plantar fasciotomy. To relieve tension, the surgeon reaches the plantar fascia and makes a partial cut or release. This makes it easier for the fascia to stretch and lessens the load on the torn area. It’s an effective method for relieving pain and improving mobility.
Endoscopic Plantar Fasciotomy: Endoscopic surgery is a minimally invasive procedure that makes use of specialized tools, such as an endoscope equipped with a camera, and tiny incisions. The surgeon can see the tight or torn areas of the fascia and release them with the help of the camera.
Ligament Repair or Reconstruction: To give the foot stability again, injured ligaments may be surgically repaired or rebuilt.
Importance of the Rehabilitation Program:
For a successful and thorough recovery following surgery or conservative treatment for a plantar fascia injury, a rehabilitation program is crucial.
After Surgery:
- Optimal Healing: Appropriate wound healing, tissue repair, and scar tissue formation are all facilitated by a well-designed rehabilitation program.
- Restoring Function: Certain exercises aid in regaining joint mobility, muscle strength, and range of motion that have been lost as a result of surgery.
- Supporting Surgical Outcome: Long-term functionality and the success of the procedure are enhanced by active rehabilitation participation.
- Guided Progression: By avoiding overexertion through gradual exercises and controlled movements, tissues can heal without experiencing undue stress.
- Redressing Imbalances: Rehabilitation addresses movement compensations and muscular imbalances that may have worsened the injury.
- Gait Correction: Correcting your gait through gait training helps you avoid bad walking mechanics that could cause your plantar fascia to re-injure.
- Regaining Confidence: Rehabilitation improves psychological health by offering a well-organized strategy and observable results.
After Conservative Management:
- Promoting Healing: In a rehabilitation program, mild workouts and therapies help the injured plantar fascia heal.
- Strengthening: By targeting the muscles surrounding the foot and ankle, strengthening exercises help to maintain stability and reduce the risk of re-injury.
- Range of Motion: By preserving or regaining joint mobility, controlled workouts help to avoid stiffness and enhance general foot function.
- Handling Muscle Imbalances: Rehabilitation takes care of any underlying weakness or imbalance in the muscles that led to the injury.
- Improving Function: A gradual return to everyday tasks, employment, and athletics is supported by progressive exercise.
- Recurrence Prevention: Rehabilitation lowers the chance of re-injury by teaching appropriate foot mechanics and movement patterns.
- Long-Term Foot Health: Participating in a rehabilitation program helps to prevent chronic problems and enhances overall foot health.
- Patient Empowerment: By actively including patients in their recuperation, a structured program empowers them.
Physical Therapy Treatment:
Physical therapists employ a variety of methods and instruments known as physical therapy modalities to treat pain, lower inflammation, encourage recovery, and enhance general function. These techniques can be quite helpful in your recuperation if you have a plantar fascia rupture.
- Ultrasound Therapy: The use of high-frequency sound waves that cause tissue vibrations is known as ultrasound therapy. It can lessen inflammation, encourage healing, and improve blood flow in the plantar fascia. After applying a gel to your skin, the therapist applies a tiny ultrasound wand over the affected area.
- Electrical Stimulation: To target particular muscle groups or trigger sites, electrical stimulation may be employed.
- Cold Therapy (Cryotherapy): The application of cold therapy is usually brief, and the therapist may employ methods such as ice packs or massage.
- Iontophoresis: This method delivers anti-inflammatory drugs through the skin by means of a low-level electric current. It can be applied to the plantar fascia and surrounding tissues to reduce inflammation.
- Laser treatment: To encourage tissue repair and stimulate cell activity, low-level laser treatment (LLLT) employs low-intensity lasers.
- Shortwave diathermy is a medical procedure that produces heat deep within tissues by using electromagnetic waves. It is frequently used in conjunction with other medications, though individual success varies.
Soft Tissue Mobilization:
Blood circulation, muscle tension, and tissue mobility in the foot and calf muscles can all be improved using manual treatments, including massage, myofascial release, and trigger point therapy.
Massage:
Ball massage:
- Locate the region: The back, neck, shoulders, hips, glutes, and feet are common places to receive ball massages.
- To apply pressure, place the ball in the desired location and then lightly push your weight against it.
- Breathe deeply and attempt to relax your muscles as you apply pressure. Avoid holding your breath.
Foot rolling with a frozen water bottle:
- Press the thing softly with your body weight as you roll your foot over it.
- Another option is to twist your entire foot, paying particular attention to the arch and the region next to your toes.
Heel-of-hand massage:
- Start with longer, lower-pressure strokes and work your way up to longer, higher-pressure ones. Lean in for the massage and apply greater pressure by using your whole weight.
Balance and Proprioception Training:
A thorough rehabilitation program must include balance and proprioception training in order to manage plantar fascia pain and avoid injuries. The ability of the body to perceive its position in space and its movements is known as proprioception.
Gait training:
A key component of rehabilitation for people recuperating from plantar fascia injuries or pain is gait training. Good walking mechanics, or gait, can ease plantar fascia tension, encourage recovery, and stop problems from happening again.
Taping or Strapping Techniques:
To support the foot, ease plantar fascia tension, and encourage healthy biomechanics, kinesiology or sports tape may be used. Plantar fasciitis or mild plantar fascia soreness are among the foot disorders for which taping treatments might offer temporary support and relief. Two popular taping methods that can help reduce symptoms are listed below.
- Low-Dye Taping Technique
- Arch Taping Technique.
Home Advica of Plantar Fascia Tear:
The goals of at-home treatment for a plantar fascia tear are to lessen pain, encourage recovery, and stop further damage. Rest is essential; stay away from activities that strain the foot, particularly high-impact exercises or extended standing. Pain and inflammation can be lessened by applying cold packs for 15 to 20 minutes many times a day.
Even inside, arch support and fascia protection can be achieved by wearing supportive shoes or orthotic inserts. Recovery can be facilitated by performing mild calf and plantar fascia stretching exercises as prescribed by a physical therapist. To reduce tension and promote healing, it’s also advised to elevate the foot and refrain from going barefoot.
Prevention of Plantar Fascia Tear:
Maintaining good foot health and preventing undue strain on the fascia are key to preventing a plantar fascia injury. Plantar fascia pain can be greatly decreased by wearing supportive shoes with enough cushioning and arch support. Exercises that stretch and strengthen the calf and foot muscles increase stability and flexibility while reducing the chance of injury.
Additionally, keeping a healthy body weight lessens foot strain. Avoiding abrupt increases in physical activity and adequately warming up before exercise are crucial. To reduce impact, people who stand or walk for extended periods of time should take rests and use insoles or padded mats.
Complications:
Chronic heel pain, decreased mobility, and trouble carrying out daily tasks or exercises are all possible consequences of a torn plantar fascia. Inappropriate treatment of the tear may result in chronic inflammation and the formation of scar tissue, which could make the foot stiff and restrict its range of motion.
Sometimes a serious or untreated tear can change how you walk, which puts more strain on your back, hips, or knees. The development of plantar fibromatosis, a disorder in which benign nodules form on the fascia, or the risk of re-injury, can also be increased by repeated stress or inadequate healing.
Prognosis:
With the right care and rest, a plantar fascia tear usually has a good prognosis. Depending on the extent of the tear and compliance with rehabilitation guidelines, most people recover well in a matter of weeks to months. With few long-term consequences, a complete recovery to regular activities is anticipated in patients with partial tears.
Complete tears, on the other hand, might require more intense rehabilitation and take longer to heal. The prognosis is much improved, and the chance of persistent pain or recurrence is decreased with early identification and adequate management.
Conclusion:
In summary, a plantar fascia tear is a painful but treatable condition that affects the foot’s connective tissue and is frequently caused by excessive use or abrupt strain. Most people can anticipate a full recovery with early diagnosis, enough rest, and a planned course of treatment that may involve physical therapy and supportive footwear. Avoiding re-injury is mostly dependent on preventive measures like stretching, wearing appropriate footwear, and progressively increasing physical activity. In addition to ensuring efficient recovery, prompt and adequate care also contributes to the long-term mobility and health of the foot.
FAQs
Can I treat a plantar fascia tear with over-the-counter pain relievers?
Pain and inflammation can be managed using over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs). However, before taking any medication, speak with your doctor.
Which shoes are best for treating a tear in the plantar fascia?
Wearing supportive shoes with enough arch support and cushioning can help reduce plantar fascia irritation. During your recuperation, stay away from flat or unsupportive shoes.
With a torn plantar fascia, can I still walk or put weight on my foot?
It’s important to refrain from doing anything that wor the paisen. Seek advice from a healthcare professional.
When should I go to the doctor if I have a torn plantar fascia?
It’s best to get medical aid for a proper diagnosis and treatment plan if you have extreme pain, have trouble walking, or find that conservative remedies aren’t working after a few weeks.
Can I treat a plantar fascia injury with over-the-counter orthotics or arch supports?
Orthotics or over-the-counter arch supports may offer some help, but it’s best to get advice from a healthcare provider. For certain foot mechanics, custom orthotics may be more beneficial.
With a torn plantar fascia, should I still exercise?
Certain activities may need to be avoided or modified during the healing period, depending on how severe the tear is.
Can I avoid tearing my plantar fascia?
A plantar fascia tear can be avoided by taking preventative steps such wearing appropriate footwear, stretching before exercise, keeping a healthy weight, and progressively increasing activity levels.
Can a plantar fascia injury be treated with physical therapy?
Indeed, physical therapy plays a crucial role in recovery. Stretching, manual therapy, therapeutic exercises, and techniques like soft tissue mobilization or ultrasound can promote healing, enhance function, and stop recurrence.
Does a torn plantar fascia require surgery?
When conservative measures have not produced relief after a considerable amount of time, surgery is usually recommended. In order to mend injured fascia, surgery may be performed to remove damaged tissue or release tension.
What options are there for treating a tear in the plantar fascia?
Rest, ice, pain relief, physical therapy, orthotics, taping, supportive footwear, and in certain situations, surgery, are all possible forms of treatment.
Is it possible for a damaged plantar fascia to mend itself?
With the right care, conservative therapies, and relaxation, minor tears may heal. However, medical intervention may be necessary for serious tears or those that do not improve with nonsurgical approaches.
Are there any other ways to treat a tear in the plantar fascia?
Even while complementary therapies like chiropractic adjustments or acupuncture may help, it’s crucial to speak with a healthcare professional first and make sure that these treatments are combined with evidence-based ones.
Can a plantar fascia tear be effectively managed with taping?
Low-Dye taping is one type of tape treatment that can assist reduce pain during movement and offer temporary support. To find out the right taping methods, speak with a physical therapist.
How does nutrition affect the healing of a tear in the plantar fascia?
The healing process can be aided by a nutritious, well-balanced diet, particularly one that supports the health of bones and tissues. Protein, calcium, and vitamin D are essential nutrients for healing.
How can I stop a plantar fascia tear from happening again?
After healing, maintaining optimal foot health is essential. This include avoiding activities that could put undue strain on the plantar fascia, wearing suitable footwear, stretching frequently, and performing strengthening exercises.
How is a tear in the plantar fascia diagnosed?
A physical examination, a review of the patient’s medical history, and potentially imaging tests like ultrasound or X-rays are all part of the diagnosis process. The diagnosis may be supported by additional testing and clinical evaluations.
What symptoms point to a ruptured plantar fascia?
Sharp heel pain, particularly with the initial morning steps, pain that gets worse with movement, tenderness, swelling, and trouble standing or walking for long periods of time are common symptoms.
What is a tear in the plantar fascia?
The heel and arch of the foot may experience pain and pain as a result of overuse, injury, or other causes.
References
- Patel, D. (2023g, August 19). Plantar fascia tear – Cause, symptoms, treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/plantar-fascia-tear/