Pain Management
During a pain management plan, medical professionals help you manage pain of all kinds and causes. Medication, surgery, therapy, and complementary medicine methods are some of the methods used to manage pain. People with chronic (long-lasting) pain can feel better and live better thanks to these plans.
Pain management: What is it?
With the use of drugs, treatments, exercises, and therapy, pain management assists you in controlling your pain. To avoid, lessen, or relieve pain, pain management professionals may suggest a single strategy or a mix of several. You might be treated in a hospital, a pain clinic, or the office of your healthcare professional.
Throughout your life, you may encounter thousands of injuries and diseases, with pain being the most common symptom. It may also be the primary symptom of a disease (pain disorder) or the outcome of medical interventions for illnesses and injuries. Acute pain may be temporary and disappear as you recover. Alternatively, persistent pain may persist for months or years.
Everybody experiences pain differently, and it is very complicated. You could be concerned that the pain will never go away or that people won’t take you seriously. Recognize the importance of looking for medical attention. Nobody should have to bear suffering every day.
Finding complete relief might not be achievable, depending on the type and origin of the pain. Furthermore, the pain might not immediately subside. Improving your quality of life and functioning—including carrying out everyday duties, taking pleasure in routine activities, working, and/or going to school—is the aim of pain management. To help you feel better, your healthcare team or physician will work together with you to modify your pain management strategy.
Types of Pain Management
Acute pain
- One common response to a disease or injury is acute pain. It usually lasts only a short time and begins suddenly. In a matter of minutes or months, acute pain can be resolved. It is frequently caused by particular wounds or incidents, like surgery, fractured bones, cuts, or delivery. Opioids and nonpharmacological therapies including physical therapy, ice packs, and heat packs can be used to manage acute pain.
Chronic pain
After the expected healing period, chronic pain continues to exist. In most cases, it lasts longer than three months. Every day, chronic pain varies from mild to severe and lasts more than six months. It frequently results from medical issues like:
- Diabetes
- Cancer
- Fibromyalgia
- Circulation problems
- Back pain
- Headaches
Chronic pain can have a harmful impact on a person’s quality of life if they are not properly treated. Anxiety or depression may result from this. Fortunately, antidepressants, opioids, capsaicin cream, and nonpharmacological therapies can all be used to manage pain.
Neuropathic Pain
Damage to the nerves causes neuropathic pain. It could have a sharp, searing, stabbing, or shooting pain sensation. It may result in uncomfortable touch, cold, and heated feelings.
Even though cancer, alcoholism, stroke, amputation of a limb, chemotherapy, radiation, or diabetes can all cause neuropathic pain. Radicular pain is a form of neuropathic pain, although it is sometimes included as a significant type of pain. Anticonvulsants, antidepressants, capsaicin cream, and nonpharmacological therapies can all be used to treat neuropathic pain.
Nociceptive pain
- Tissue injury is the cause of nociceptive pain. One way to characterize it is as a sharp, aching, or throbbing ache. External injuries like falling, bumping against objects, or being struck are the source of this pain.
- Tendons, muscles, joints, bones, and skin can all experience nociceptive pain. Physical therapy, over-the-counter (OTC) medications, opioids, and antidepressants are some of the treatment options.
Pain can range from mild to severe and can feel like anything from a slight pain to a sharp stabbing. You might experience pain in a single area or across your body.
Benefits of Pain Management
The nature of chronic pain is complicated. Over time, it can alter how your nerve system and brain function. Therefore, a thorough pain management strategy overseen by professionals is probably the most effective way to address it. Complete pain relief isn’t always achievable. However, you might be able to lessen pain or develop new ways of handling it.
With a pain management program, many persons with chronic pain have physical and mental improvements as well as an improved quality of life. Current treatments for chronic pain have been shown to reduce pain scores by roughly 30%.
The Role of Pain Management
For patients with chronic pain in particular, pain management specialists are essential to enhancing their quality of life. Pain management specialists are well qualified to diagnose and treat a wide range of pain conditions. They work together with patients to develop individualized treatment programs that address both the psychological and physical components of chronic pain.
To specialists in pain management, lessen the severity of pain, enhance physical function, and improve a patient’s general health. Medication, physical therapy, and dietary modifications are all possible components of their multidisciplinary approach. In order to properly manage pain, they may occasionally suggest treatments or surgeries.
For people with chronic pain, a pain management specialist can have a profoundly positive impact on their lives. Patients can take back control of their lives with the aid of efficient pain management programs. They might be able to engage in enjoyable activities and feel less stressed both mentally and physically.
The field of pain management is impactful and successful. A person’s quality of life can be enhanced by pain treatment professionals. A job in this area may offer opportunity for ongoing education and professional fulfillment. People with chronic pain might find pause and hope thanks to the knowledge of pain management specialists.
Causes of pain
The following are the most typical reasons why adults experience pain:
Pain caused by tissue damage
Tissue damage, or injury to your body’s tissues, is the main cause of pain. Bone, soft tissue, or organs may sustain the damage. It may result from an illness like cancer. A physical injury, such as a cut or a fractured bone, may also be the cause.
You can experience a throbbing, a severe stabbing, or an ache. It may be continuous or intermittent. When you laugh or move, the pain could seem to worsen. It may seem particularly intense at times if you breathe deeply.
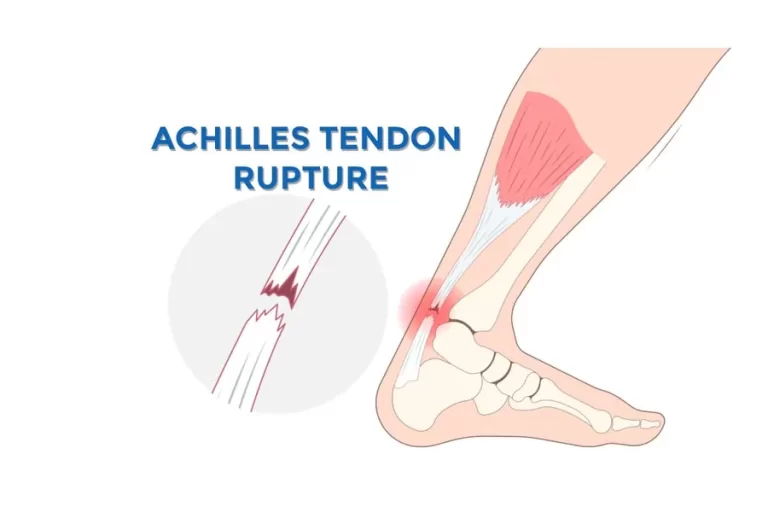
Tissue injury can cause difficult pain. For instance, soft tissue damage frequently results in sports injuries like a sprained ankle or an artificial grass toe. Alternatively, it may be chronic, like arthritis or persistent headaches. Additionally, some medical procedures, like radiation therapy for cancer, can harm tissue, which results in pain.
Pain caused by nerve damage
Nerves function similarly to electrical wires, transmitting and receiving signals from the brain, including pain signals. Nerve damage can challenge the transmission of such signals. This may result in pain signals that aren’t functioning properly. For example, even when there is no heat, you could feel as though your hand or anything else is burning.
Nerve injury can result from conditions. Or they may sustain harm from an injury. Some chemotherapy medications have the potential to harm nerves. HIV infection and stroke are two more conditions that can harm nerves. Damage to the brain and spinal cord, which make up the central nervous system (CNS), may be the cause of pain. Damage to peripheral nerves, which are the nerves in the rest of the body that communicate with the central nervous system, may also be the cause.
Neuropathic pain, which results from injury to the nerves, is frequently characterized as prickly or burning. It is compared to an electrical shock by some. Others describe it as a stabbing sensation or as being like pins and needles. Some individuals with nerve injury frequently have extreme sensitivity to touch and temperature. Light contact, such as rubbing against a bed sheet, can trigger the pain.
Many cases of neuropathic pain are persistent. The following are some instances of pain caused by damaged nerves:
Central pain syndrome. Damage to the central nervous system is the first cause of this persistent pain. Tumors, multiple sclerosis, strokes, and several other illnesses can cause the damage. A vast portion of the body or smaller parts, such as the hands or feet, may be affected by the pain, which is typically persistent and can be extremely severe. Changes in temperature, movement, contact, and emotions all frequently worsen the pain.
Complex regional pain syndrome. After a severe injury, this chronic pain syndrome may develop. They say it burns all the time. Additionally, you may experience unusual perspiration, skin color changes, or swelling in the area of pain.
Peripheral neuropathic pain in diabetics. Diabetes damages the nerves in the hands, arms, legs, and feet. It may have a tingling, burning, or stabbing sensation.
Postherpetic neuralgia with shingles. It is a localized infection that can cause difficult pain and redness. It occurs along a nerve’s route on one side of the body. A typical issue that arises when shingles pain persists for more than a month is postherpetic neuralgia.
Trigeminal Neuralgia. Severe, lightning-like pain is the result of inflammation of a facial nerve. On one side of the face, it may occur in the lipstick, scalp, forehead, eye, nose, gums, cheek, and chin. Even small movements or touches might trigger the pain.
How pain affects the body?
Pain is a advanced defense system. It is a vital component of evolution that shields the organism from harm and danger. Two primary nerve kinds that sense danger are connected to pain receptors in the body. A sharp, unexpected pain is caused by a neuron type that transmits messages swiftly. The other produces a dull, throbbing pain as it sends messages slowly.
There are more pain receptors in some parts of the body than in others. For instance, the skin has many receptors, making it simple to pinpoint the precise place and kind of pain. It is more difficult to determine the exact location of a stomach ache because the stomach has significantly fewer sensors.
The spinal cord and the thalamus, a region of the brain, receive messages from pain receptors in the skin that are triggered by touching something harmful, such as something hot or sharp. Occasionally, the muscles receive an instantaneous signal from the spinal cord to contract. By doing this, the affected bodily portion is moved away from the danger or injury.
This is a reflex response that stops additional harm from happening. It takes place before experiencing pain. The thalamus sorts the information given by the nerves after receiving the “alert!” signal, taking into consideration your past experiences, beliefs, expectations, culture, and social standards. This explains why people react to pain in very diverse ways.
The information is subsequently transmitted via the thalamus to other brain regions associated with emotion, thinking, and bodily reaction. At this point, you can experience pain and think, “That hurt!” “What was it?” and become irritated. The thalamus also plays a role in mood and arousal, which helps to explain why your mental state influences how you perceive pain.
Managing pain without medicines
There are numerous non-pharmacological ways to assist you in controlling your pain. Often, a mix of therapies and treatments works better than a single one.
Among the alternatives to medicine are:
Use ice packs, either hot or cold, as soon as possible after an injury to minimize swelling. For the treatment of persistent joint or muscle problems, heat packs work better.
Walking, stretching, strengthening, and aerobic activities are examples of physical therapy that can help you feel better, stay mobile, and lessen pain. To prevent going overboard, you might need to gradually increase your workout.
Another physical therapy is massage, which is best suited for soft tissue injuries and should be avoided if joint pain is present. Although massage is not advised as a long-term therapy, there is some evidence that it may assist in managing pain.
Methods for stress reduction and relaxation, such as yoga and meditation. Cognitive behavioral therapy (CBT) is a type of psychological treatment that can teach you how to alter your thoughts, which will alter how you feel and act while you are in pain. This is a useful method for developing self-management skills for chronic pain.
One components of traditional Chinese medicine is acupuncture. Thin needles are inserted into predetermined skin sites during acupuncture. By releasing endorphins, which are naturally occurring painkillers, it seeks to bring the body back into equilibrium and promote healing. Acupuncture helps some people maintain function by lessening the intensity of their pain. However, research on acupuncture’s ability to effectively manage pain is opposing.
Transcutaneous electrical nerve stimulation (TENS) therapy, electrodes deliver low voltage electrical currents via the skin, causing the body to produce a pain-relieving reaction. The use of TENS to treat certain chronic pain problems is not well supported by published research. On the other hand, certain chronic pain sufferers who don’t respond to other therapies might benefit.
The optimal course of treatment for you can be discussed with your physician or other healthcare provider.
Pain management programs
Taking part in a pain management program can be a helpful strategy if pain doesn’t go away after three months of treatment. The various components influencing your recovery are specifically addressed by these rehabilitation programs, which include:
- Social aspects include how you handle your home and social activities, your safe return to work, and any psychological problems like your mood, stress, or lack of sleep.
- Health specialists (including physicians, physiotherapists, psychologists, occupational therapists, and nurses) will teach you how to better control your pain with the fewest possible adverse effects during pain management programs.
Managing pain with medicines
Analgesics, or painkillers, are used by many people at some point in their lives.
The primary categories of painkillers include:
- For short-term pain relief, paracetamol is frequently suggested as the initial medication.
- Aspirin is used to treat fever and mild-to-moderate pain, including headaches and period pain, in the short term.
- Ibuprofen is one example of a non-steroidal anti-inflammatory drug (NSAID), which reduces inflammation (redness and swelling) and relieves pain.
- Codeine, morphine, and oxycodone are examples of opioid medications, which are only used to treat extreme or malignant pain.
- When nerves are easily accessible, local anesthetics (drops, sprays, creams, or injections) are utilized.
- Certain antidepressants and anti-epilepsy medications are used to treat nerve pain, a particular kind of pain.
How pain medicines work
There are several ways that painkillers function. NSAIDs, such as aspirin, are painkillers that lower heat and inflammation. They accomplish this by inhibiting substances known as prostaglandins. Prostaglandins can result in pain by causing edema, inflammation, and nerve ending sensitivity.
Because prostaglandins also protect the stomach from stomach acid, some persons may have bleeding and irritation from these medications. Opioid medications function differently. These medications have the potential to become addictive because they alter the brain’s perception of pain.
Choosing the right pain medicine
The following factors will determine which medication is best for you:
- The type, location, length, and intensity of your pain; any activities that help or worsen it; the way your pain affects your lifestyle, including how it impacts your appetite or sleep quality; any other medical conditions you may have; and any medications you take.
- To select the safest and most efficient pain management solution, talk about it with your physician or other healthcare provider.
Managing your medicines effectively
For safe and efficient medication administration, always abide by the directions. By doing this:
- You can lower your risk of side effects and are less likely to require higher dosages of medication if your pain is adequately managed.
- It is best to use chronic pain medications regularly. If your medications aren’t working or are giving you trouble, such as side effects, speak with your doctor or pharmacist. If you have been taking painkillers for a long time, these are more likely to happen.
It’s critical to employ a range of pain management techniques. Don’t depend on just on medications. Individuals can lessen their pain thresholds by:
Maintaining an active lifestyle and balancing their daily activities to prevent pain flare-ups (this comprises striking a balance between doing too little and too much).
Use coping mechanisms to stay away from pain triggers.
Precautions when taking pain medicines
As with all medications, use caution when taking over-the-counter pain relievers. Talking to your doctor or pharmacist about any medications is always a good idea.
Some general recommendations are:
- Avoid using painkillers as a form of self-medication when pregnant because some of them can potentially harm the fetus by crossing the placenta.
- If you are elderly or providing care for someone who is, exercise caution. Side effects are more likely to occur in older adults. For instance, taking aspirin daily to treat chronic pain (like arthritis) can result in a potentially fatal bleeding stomach ulcer.
- Talk to a pharmacist about any prescription and supplementary medications you are taking before purchasing over-the-counter pain relievers so they may assist you in selecting a medication that is safe for you.
- Avoid taking more than one over-the-counter medication at once without first talking to your pharmacist or doctor. Unintentionally taking too much is easier than you might imagine. For instance, a lot of “cold and flu” medications contain paracetamol, thus it’s crucial to avoid taking any other medications that contain paracetamol at the same time.
- For appropriate treatment for sports injuries, consult your physician or other healthcare provider.
- Avoid using painkillers to “tough it out.”
- If you have a chronic (long-term) medical condition, such as diabetes or heart disease, speak with your doctor or pharmacist before using any over-the-counter medications.
Side effects of pain medicines
The following are a few adverse effects of typical painkillers:
- When taken as directed and for a brief period, paracetamol rarely causes negative effects. Long-term usage of high dosages of paracetamol might result in liver damage and skin rashes.
- The most frequent adverse effects of aspirin are stomach ulcers, indigestion, nausea, and vomiting. More severe adverse effects include an asthma attack, tinnitus (ear ringing), renal damage, and bleeding may occur in certain individuals.
- High blood pressure, headache, nausea, upset stomach, heartburn, skin rash, fatigue, dizziness, and ringing in the ears are all side effects of non-steroidal anti-inflammatory medicines (NSAIDs). Additionally, they can worsen kidney or heart failure and raise the risk of bleeding, angina, heart attacks, and strokes. Always use NSAIDs with caution and for as little time as possible.
- Opioid painkillers, including morphine, oxycodone, and codeine, frequently result in constipation, nausea, vomiting, falls, and drowsiness. They may also impair balance and physical coordination. Crucially, these medications limit breathing and can cause dependence, which can lead to an unintentional overdose that is lethal.
- A Consumer Medicine Information guide with contains a more comprehensive list of adverse effects. Before taking any pain medication, see your physician or pharmacist to make sure it’s safe for you.
Managing pain that cannot be easily relieved
Pain can occasionally be difficult to relieve and last a long time. When in pain, it’s normal to feel anxious, depressed, or worried. The following advice can help you deal with chronic pain:
- Instead of trying to eliminate the pain, concentrate on enhancing your daily functioning.
- Recognize that flare-ups may happen and that your pain may not go away. Talk yourself through these situations.
- Learn as much as you can about your disease to avoid worrying about the pain needlessly.
- Get your friends and relatives to help. Find ways to stay in touch and let them know what kind of help you require.
- Use whatever strategies you find most effective to prevent or lessen depression, such as speaking with friends or experts.
- Increasing your dosage could make your pain worse and perhaps hurt you.
- Increase your level of physical fitness, consume a balanced diet, and get enough sleep.
- Try not to let the suffering prevent you from leading the life you desire. Try reintroducing things you used to appreciate gently. If pain flares up, you may need to reduce some activities, but gradually resume your previous level of activity.
- Focus on engaging in enjoyable and fulfilling activities that don’t worsen your pain.
Diagnosis
Your doctor can determine the cause of your pain in several ways. Your symptoms and medical history, including any illnesses, injuries, or surgeries, will be questioned.
In addition to examining you, your doctor might prescribe X-rays or blood tests. The following tests can assist in determining the source of your pain:
- CT scan
Computed tomography scans provide an image of a cross-section of the body using computers and X-rays. You lie on a table as still as you can for the test. Before your scan, your doctor could occasionally inject a solution into a vein. It may make it simpler to see what’s happening within. The majority of CT scans take between fifteen and an hour.
- MRI
Your doctor can see clear images of your internal organs and structures with magnetic resonance imaging. This test creates graphics using radio waves, a computer, and a huge magnet. Depending on how many pictures are taken, an MRI might take anywhere from fifteen minutes to over an hour. A contrast agent shot is required for some MRIs to get sharper images. Some patients, such as those with pacemakers, shouldn’t get an MRI because it involves magnets.
- Nerve blocks
Your pain can be diagnosed and treated with these tests. Your doctor injects an anesthetic (a substance that numbs pain) into certain nerve sites. To determine the ideal location for the needle, they could employ an imaging test. Your reaction to the nerve block could provide insight into the source of your pain.
- Myelogram
Neck and back pain can also be evaluated with this exam. A myelogram involves injecting a dye into your spinal canal. The test aids in detecting nerve compression caused by fractures or herniated disks.
- EMG
Doctors can examine muscle activity with an electromyogram. To evaluate how your muscles react to electrical signals, your doctor inserts tiny needles into them.
- Bone scans
These aid in the diagnosis and monitoring of infections, fractures, and other bone problems. A tiny quantity of radioactive material is injected into your circulation by a physician. The substance will assemble in the bones, especially in abnormal places. Then, a computer can recognize those particular regions.
- Ultrasound imaging
This procedure, also known as sonography or ultrasonic scanning, creates images of the inside of the body using high-frequency sound waves. The echoes of the sound waves are captured and shown as an image in real time.
What kinds of pain management are there?
One strategy or a mix of many pain treatment approaches may be suggested by your healthcare physician or pain management team. It could comprises managing pain as a symptom or treating the underlying source of pain.
Even for the same cause of pain, different people respond differently to different treatments. Before attempting riskier pain treatment techniques, providers usually begin with conservative or minimally invasive ones. However, there isn’t a single “right” way to manage pain for everyone.
Occupational and physical therapy for the treatment of pain
The goal of physical therapy is to help you get better at the physical motions your body does. It may be a specialized treatment for an injury or medical condition, or it may be a component of a broader pain management strategy.
The goal of occupational therapy is to help you become more capable of performing everyday chores. It can assist you in learning how to navigate your surroundings or make use of various instruments to engage in your activities in a way that reduces pain.
Pain management using psychotherapy
The term “psychotherapy” (sometimes known as “talk therapy”) refers to a range of therapeutic approaches intended to assist you in recognizing and altering maladaptive feelings, ideas, and behaviors. It can assist you in controlling or altering your pain perception.
Your doctor might also suggest psychotherapy and/or medicines for your mental health because chronic pain can also result in anxiety and despair.
You can develop coping mechanisms to manage the emotional strain of chronic pain and any related mental health issues, especially with cognitive behavioral therapy (CBT).
These abilities could include mindfulness practices, relaxation methods, and dealing with feelings and ideas that worsen pain. To follow what causes pain to get better or worse, some people keep a pain journal. Your provider can use these details to assist in planning your therapy.
Pain management by Trigger Point Injections
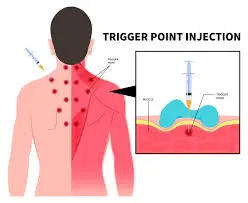
Painful muscle connections known as trigger points, which develop when muscles do not relax, can be treated with trigger point injections. A local anesthetic, occasionally containing a steroid, is injected into a trigger point by a medical practitioner using a tiny needle during this operation (sterile salt water is sometimes administered). The injection relieves the pain and renders the trigger point inert. A short course of treatment will typically provide long-lasting relief.
Injections of trigger points are used to treat neck, lower back, arm, and leg muscle pain. This method has also been used to treat myofascial pain syndrome, which is characterized by persistent pain involving the tissue around muscles that does not improve with other therapies, fibromyalgia, and tension headaches.
The toxin known as nonbotulinum toxin, or Botox, prevents nerve signals from reaching the muscles. Additionally, it can be injected to treat persistent migraine headaches. Pain may be reduced for up to three months with the surgery, which comprises many injections around the head and neck every twelve weeks.
Acupuncture

It is believed that acupuncture reduces pain by promoting the release of endorphins, which are pain-blocking molecules. Nerves are close to a lot of acupoints. These nerves produce a dull pain or a sensation of fullness in the muscle when they are stimulated. Endorphins are released in response to the signal from the activated muscle to the brain and spinal cord, which prevents the brain from receiving the pain signal.
Numerous pain-related illnesses, such as headache, low back pain, menstrual cramps, carpal tunnel syndrome, tennis elbow, fibromyalgia, osteoarthritis (particularly of the knee), and myofascial pain, may benefit from acupuncture as a supplemental treatment. Additionally, acupuncture could be a suitable substitute for or component of an all-encompassing pain management program.
Chiropractic Treatment and Massage

The most popular nonsurgical treatment for back pain is chiropractic care. In certain trials, improvements were shown in patients receiving chiropractic manipulations. However, the bulk of clinical trials have not produced strong data supporting the treatment’s efficacy in treating chronic neck and back pain. The usefulness of chiropractic therapy for pain management is presently being evaluated by more research.
People who are in pain are using massage more and more, primarily to treat persistent neck and back issues. By improving blood flow, massage can ease tension and reduce stress. Additionally, this treatment might lessen the amount of drugs that can cause and maintain pain. The information that is now available indicates that massage treatment, like chiropractic adjustments, has a lot of potential for treating back pain. However, due to the limitations of the research that is currently available, it is not possible to make definitive judgments on how well massage works to relieve pain.
Exercise

Short-term rest can help reduce pain, but prolonged rest might worsen it and raise your risk of damage when you try to move again. Regular exercise can reduce pain over time by increasing muscular tone, strength, and flexibility, according to research. The body’s natural painkillers, endorphins, may also be released as a result of exercise. Exercises including swimming, biking, walking, rowing, and yoga may be easier for some people with chronic pain than others.
Home-based methods for managing pain

Pain from soft tissue and muscular injuries could be manageable at home. Inquire about heat and cold therapy and the RICE method (rest, ice, compression, and elevation) from your healthcare professional.
Pain can be reduced by making certain lifestyle adjustments. Your healthcare professional might advise you to achieve and maintain a healthy weight if you are overweight or obese. Pain may be lessened by eating a healthy diet, staying hydrated, getting enough sleep, and controlling stress.
Strength training and physical activity (such as swimming or walking) may also lessen pain. These exercises can help your body function better overall and aid you with posture. They also help you maintain equilibrium and improve your mental wellness. Before beginning an exercise program, consult your healthcare provider.
RICE protocol
Rest.
- Rest and protect the aching or wounded region. Any activity that might be causing your pain or soreness should be stopped, modified, or stopped for a while.
Ice.
- To avoid or reduce swelling, apply a cold pack or ice immediately. Pain and swelling will be lessened by cold. Three or more times a day, apply the ice or cold pack for ten to twenty minutes. Apply heat to the painful area if the edema has subsided after 48 to 72 hours. Don’t apply heat or cold straight to your skin. Cover the heat or cold pack with a cloth before applying it to the skin. Ice should also be applied after intense exercise or any extended activity.
Compression.
- To help reduce swelling, apply an elastic bandage, like an Ace wrap, to the wounded or sore region. Avoid wrapping it too tightly as this may result in further swelling beneath the affected area. If the bandage becomes too tight, loosen it. Numbness, tingling, increased pain, coolness, or swelling in the area beneath the bandage are all indicators that the bandage is excessively tight. If you believe you need to use a wrap for more than 48 to 72 hours, consult your doctor because there might be a more serious issue.
Elevation.
- While applying ice and while you are sitting or lying down, elevate the damaged or aching area on cushions. To reduce swelling, try to keep the area at or above the level of your heart.
Complication of pain management
Every pain management strategy has potential hazards, adverse effects, and problems of its own. And depending on your medications and other medical problems, these could differ from person to person.
For instance, the most frequent cause of acute liver failure in the United States is excessive use of the over-the-counter drug acetaminophen. Also, using prescription opioids increases your risk of developing an opioid use problem. There are additional dangers associated with surgeries and more invasive procedures, such as infection and irreversible nerve damage.
Before beginning any pain management treatment, discuss the advantages and disadvantages with your healthcare professional. Never be worried to ask questions. Your healthcare provider is there to support you, not to pass judgment.
Who needs pain management?
A pain management strategy can help anyone who experiences pain, whether it be acute or chronic. You can manage pain that lasts a few days (such as following surgery or an injury) with the help of a thorough plan. If you have chronic pain from medical disorders, it may also be helpful.
- Arthritis, muscle and joint injuries.
- Autoimmune diseases, such as fibromyalgia, lupus, and Crohn’s disease.
- Burns.
- Cancer.
- Causes of neuropathic pain, such as peripheral neuropathy, trigeminal neuralgia, and pinched nerves.
- Chronic pain conditions, such as central pain syndrome and complex regional pain syndrome (CRPS).
- Circulatory disorders, like peripheral artery disease.
- Endometriosis.
- Headaches and migraines.
- Spine- or spinal cord-related conditions or injuries.
For pain management, who do I see?
You might choose to start with your primary care physician if you are unsure of the reason for your pain. They can begin the diagnostic procedure and direct you to a clinic or pain treatment team. If you have been diagnosed, discuss beginning a more comprehensive pain treatment plan with your healthcare provider.
To help you manage chronic or severe pain, you might have a group of pain management experts that work together. These experts are employed in pain medicine, a branch of medicine. Your group could consist of:
- Pain management specialists.
- Anesthesiologists.
- Experts in any additional illnesses you may have, such as neurologists or oncologists.
- Nurses.
- Mental health providers, like psychologists and psychiatrists.
- Physical and/or occupational therapists.
- Complementary or integrative health providers.
- Social workers.
Your team may suggest specific tests and examinations to better analyze your pain and determine its origin, such as:
- Physical examination.
- Neurological examination.
- Laboratory examinations (cerebrospinal fluid, urine, and blood tests).
- Imaging procedures such as computed tomography (CT) scans and magnetic resonance imaging (MRI).
- Electrodiagnostic investigations, such as electromyography (EMG) and nerve conduction examinations.
- How pain impacts your emotions, daily functioning, relationships, and employment, among other areas of your life.
How effective are pain management plans?
It could take some time and multiple therapies before you find the one that works for you, depending on the source of your pain and your particular traits. For instance, a single therapy is insufficient to relieve the pain in less than 50% of patients with neuropathic pain.
It may take some time for your pain to subside. Working closely with your provider or team and making necessary adjustments as your needs change can increase the likelihood that your pain management strategy will be successful.
FAQs
What is pain management?
Pain management techniques include physical therapies, pain medications, and complementary therapies (like massage and acupuncture). Research indicates that an individual’s quality of life is impacted by their perspective and how they emotionally handle pain. Seek guidance on new coping mechanisms and techniques.
Which three forms of pain management are there?
Pain & Spine Specialists’ pain management department can provide specialized treatment programs to effectively control your pain. Among the various methods, chronic, interventional, alternative, and traditional pain treatment are the most widely used.
Why is pain management?
Improving your functioning and quality of life—including carrying out daily duties, taking pleasure in routine activities, working, and/or going to school—is the aim of pain management. To help you feel better, your healthcare team or provider will work together with you to modify your pain management strategy.
What is the best drug for pain?
For short-term pain, paracetamol is frequently advised as the first medication to try. The class of medications known as nonsteroidal anti-inflammatory drugs (NSAIDs) relieves pain and reduces swelling and inflammation. They consist of diclofenac, ibuprofen, and aspirin.
What are the advantages of suffering and pain?
Suffering and pain can serve as valuable learning opportunities and opportunities for personal development. There is always a reaction to pain. Growth occurs when we accept and acknowledge suffering, regardless of our attempts to avoid or ignore it.
In what ways does suffering help?
In general, humans consider pain to be undesirable and something to be avoided. In actuality, avoiding pain is a really useful survival strategy for humans. However, it is pain that teaches us to avoid risky situations and to identify bodily danger.
Positive pain: what is it?
We point forth three distinct areas where suffering could be viewed as beneficial. First, by enhancing sensitivity to sensory information, promoting self-rewarding behavior, and offering a significant contrast for enjoyable experiences, pain promotes pleasure.
Reference
- Professional, C. C. M. (2025b, February 5). Pain management. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/21514-pain-management
- Department of Health & Human Services. (n.d.). Pain and pain management – adults. Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pain-and-pain-management-adults#types-of-pain
- Pain Management: Treatment Overview. (n.d.). WebMD. https://www.webmd.com/pain-management/pain-management-treatment-overview
- American University of the Caribbean School of Medicine. (2025, January 7). What are the Different Types of Pain Management? AUC School of Medicine. https://www.aucmed.edu/about/blog/types-of-pain-management
- Backman, I. (2024, November 7). Peripheral sodium channel blocker could revolutionize treatment for nerve pain. Yale School of Medicine. https://medicine.yale.edu/news-article/peripheral-sodium-channel-blocker-could-revolutionize-treatment-for-nerve-pain/#:~:text=A%20novel%20generation%20of%20pain,with%20neuropathy%2C%20or%20nerve%20pain.
- Department of Health & Human Services. (n.d.-b). Treating persistent pain. Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/Treating-persistent-pain
- Diagnostic tools: tests doctors use to pinpoint the cause of pain. (n.d.). WebMD. https://www.webmd.com/pain-management/pain-management-diagnosing
- RICE (rest, ice, compression, and elevation). (n.d.). UK HealthCare. https://ukhealthcare.uky.edu/orthopaedic-surgery-sports-medicine/treatment/rice





7 Comments