Pain Gate Mechanism
What is a Pain Gate Mechanism?
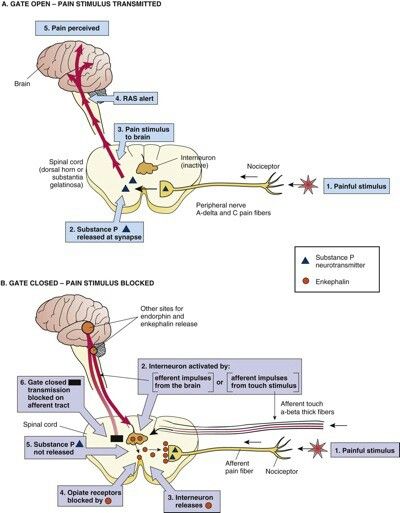
The pain gate mechanism, proposed by Melzack and Wall in 1965, revolutionized the understanding of pain perception and management. This theory elucidates how the central nervous system modulates and regulates pain signals, influencing an individual’s perception of pain intensity.
The concept of the pain gate mechanism suggests that the transmission of pain signals can be inhibited or facilitated by neural mechanisms at various levels of the nervous system.
According to the Gate Control Theory of Pain, the spinal cord system allows pain signals to either intensify or lessen perceived pain at the spinal cord level and then be processed by the brain.
This ‘pain gate’ is the mechanism that allows or restricts pain signals. There are two possible outcomes: the gate may be “open” or “closed.”
The brain will receive pain signals if the gate is open, allowing it to register the pain.
The gate will be closed, preventing pain signals from reaching the brain and preventing the experience of pain.
Applying a non-noxious stimulus, such as soothing or gentle stroking, can help engage the gate control mechanism and lessen pain when someone experiences a painful (noxious) stimulus.
History
Researchers Ronald Melzack and Patrick Wall first presented the gate control theory of pain in a study that was published in 1965. The intention was to contribute to the understanding of how mental states affect pain perception, either by elevating or decreasing pain perceptions.
Melzack and Wall proposed that this mechanism explains our propensity to massage our wounds after they occur. You might rub the damaged area if, for example, your shin bangs against a chair or table. You might rub the damaged area if, for example, your shin bangs against a chair or table. Increased normal touch sensory input contributes to the inhibition of pain fiber activity, which lessens the impression of pain.
Other theories on pain existed before the development of the gate control theory. Among them were:
Specificity theory of pain
According to the specificity idea, every pain pathway is unique and different. Additionally, each sensory fiber and the receptor has a particular stimulus to which it responds.
Intensity theory of pain
According to the theory of pain, some stimuli lack a unique route. Rather, the quantity of brain impulses determines how strong a stimulus is.
Pattern theory of pain
The pattern theory of pain states that the degree to which various sense organs react to stimuli varies.
Physiology
The substantia gelatinosa, which is found in the dorsal horn of the spinal cord, is home to the pain gate mechanism. The gating process takes place in the interneurons of the substantia gelatinosa, which synapse to the primary afferent neurons. Consequently, the sensory data arriving from the primary afferent neurons is modulated by the substantia gelatinosa.
Three types of primary neurons exist:
- Because they are myelinated, A-ß fibers with large diameters transmit impulses quickly. Non-noxious stimuli including gentle touch, pressure, and hair movement activate these types of fibers.
- A-d fibers have a smaller diameter and are triggered by noxious stimuli like pain and temperature, particularly sharp, strong, tingling sensations. They are lightly myelinated.
- Like A-d fibers, C fibers transmit impulses at the slowest rate because they are not myelinated. Pain and temperature—more specifically, chronic burning sensations—activate these fibers.
The ‘pain gate’ is closed when non-noxious large diameter A-ß fibers excite the interneurons in the substantial gelatinous, resulting in an inhibitory response and no pain signals being transmitted to the brain.
An excitatory response is generated when the interneurons are triggered by the A or C fibers with a smaller diameter. Here, the brain receives pain signals, which can be modified, transmitted back down through descending modulation, and experienced as different intensities of pain.
The small diameter A-d and C fibers’ ability to propagate can also be lessened and inhibited by activating the big diameter A-ß fibers.
At the Spinal Cord
From the periphery, the primary afferent neurons synapse with the second-order neurons in the spinal cord’s dorsal horn, releasing the corresponding neurotransmitters or neuropeptides.
Potential neuropeptides or neurotransmitters that could be released include:
Excitatory glutamate: glutamate activates NMDA receptors by enlarging the receptive field, lowering the activation threshold, and prolonging depolarization, all of which result in the activation of dorsal horn neurons.
GABA has its own unique receptors, whereas glycine can bind to NMDA. GABA and glycine are inhibitory chemicals.
Excitatory neuropeptides, such as substance P, are present in peripheral C-fibers and react to tissue damage by inducing vasodilation, inflammation, and/or pain.
In the descending route, endorphins and serotonin are produced to aid in gate control and pain reduction. Wide dynamic range (WDR) neurons and nociceptive specific (NS) range neurons are the two different categories of second-order neurons. Because the WDR neurons synapse on the A-β, A-δ, and C fibers, both noxious and non-noxious stimuli can activate them. Conversely, the NS neurons are only triggered by noxious stimuli because they only form synapses with A-δ and C fibers.
The brainstem and diencephalon include third-order neurons that carry the pain signal to the cerebral cortex. It is there that the A-δ and C fibers of the pain signal can undergo additional modulation.
Useful Applications
In addition to the sensory event, the pain signals that are transmitted from the brain (via the descending modulation) as a result of the thoughts, attitudes, emotions, and sentiments surrounding the painful experience also influence the painful sensation that is observed and experienced.
This has to do with the biopsychosocial model and has the potential to make pain seem worse or better. Pain signals are sent down from the brain through an ‘open gate’, and the pain experienced will be stronger if someone has unsettling or anxious thoughts, unpleasant feelings or recollections, unpleasant prior experiences, or unfavorable social input. However, the gate will close and the individual will basically feel less pain if they have pleasant thoughts, feelings, and recollections about the traumatic event, relax, or receive positive social feedback.
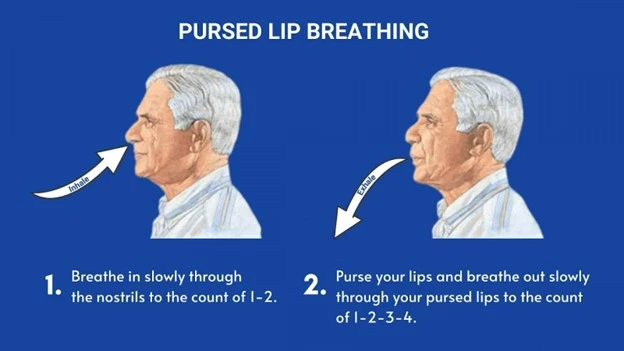
Transcutaneous Electrical Nerve Stimulation (TENS)
Using TENS lowers the perception of pain by activating the pain gate mechanism, which blocks pain impulses from reaching the brain. As previously mentioned, the TENS lessens or lowers perceived pain as output by activating non-noxious afferent fibers, which in turn stimulates “pain-inhibiting” interneurons in the spinal cord. This is so that the gate control mechanism can be facilitated.
TENS has the ability to activate A-β fibers. The input from the irritating A-δ and C fibers will be inhibited by the activation of the A-β fibers.
Physiotherapy treatments also frequently employ the Interferential Current (IFC) modality, which reduces pain through many brain systems, including the gate control mechanism.
Exercise Induced Pain
It was discovered that while TENS alone improved whole-body endurance, IFC and TENS can both significantly lessen exercise-induced pain during single-limb activity. Pain-reduction strategies like this contribute to improved exercise endurance.
Low Back Pain
It was discovered that using TENS alone as an intervention was a very successful way to reduce low back pain.
Painful symptoms and quality of life were further improved by using TENS in addition to other physiotherapy methods such as manual mobilization, massage, stretching, or exercise.
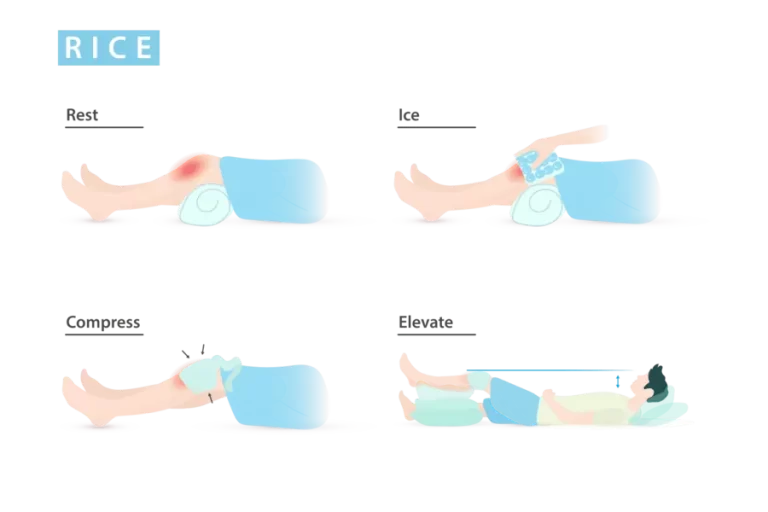
Rubbing and Massage
A common reaction to nociceptive pain is to rub it away. This is especially true when the harm is minor, such as when you strike your thumb with a hammer, burn your hand on your coffee cup, or get your hand trapped in a door. For the reasons outlined above, this soothes and lessens the pain. The pain-producing A-δ or C fibers are inhibited by the activation of the non-noxious A-β fibers.
Activating big diameter A-β nerve fibers is the same rationale used by massage therapy to lessen and suppress pain using the gate control theory. Numerous patient types may benefit from this, as it can aid in the improvement of numerous ailments, including high blood pressure, depression, stiffness, sleep, relaxation, emotional well-being, and recovery time. Cardiac patients may find relief from potential adverse effects and a reduction in or elimination of medication use by getting massages to various uncomfortable body areas.
Other techniques that apply the notion of pain control:
- The descending route is also modulated by acupressure and acupuncture.
- Vibration—akin to a TENS unit
FAQ
Who proposed the gate control theory of pain?
The 1965 Science article “Pain Mechanisms: A New Theory” by Ronald Melzack and Patrick D. Wall (1), which presented the gate control theory of pain and subsequently transformed our knowledge of pain mechanisms and treatment, is becoming 50 years old in November 2015.
What is the gate theory of pain electrical stimulation?
The gate-control theory of pain states that pain that is produced when only C fibers are active should be eliminated by electrically stimulating big nerve fibers. This type of pain was brought on by pressure, a series of pinpricks, heat, and cold in the affected limb.
What are the steps of the pain pathway?
Fundamental Pain Mechanisms
2.1. Nerve cells. It is well recognized that neurons are the main unit responsible for transmitting, receiving, and processing all nociceptive information produced by the three previously mentioned events in the CNS and PNS.
Axons (2.2)…
2.3. Possibility of Action.
Section 2.4: Synaptic Transmission.
2.5. Transmission Route of Pain.
What are the 4 theories of pain?
The Specificity (or Labeled Line), Intensity, Pattern, and Gate Control Theories of Pain are the four most prominent theories of pain perception. According to the Specificity Theory, every somatosensory modality has its own specific pathway.
What is the gate control theory of pain a delta?
Thus, no pain is felt when the interneurons are activated by strong fiber activity because the gate closes. A-delta and C fibers with short diameters are active, and this results in prolonged spinal cord activity. Engaging in such activities fosters sensitivity, which in turn heightens one’s sensitivity to pain.
REFERENCES
Gate Control Theory of Pain. (n.d.). Physiopedia. https://www.physio-pedia.com/Gate_Control_Theory_of_Pain#:~:text=The%20Gate%20Control%20Theory%20of,at%20the%20spinal%20cord%20itself.
MSEd, K. C. (2022, May 19). What Is Gate Control Theory? Verywell Mind. https://www.verywellmind.com/what-is-gate-control-theory-2795208