What is a Soleus Muscle Pain?
Soleus muscle pain often occurs due to overuse, strain, or poor posture during activities like running or walking. It can cause discomfort in the lower calf, especially during movement. Rest, stretching, proper footwear, and strengthening exercises can help alleviate pain and prevent recurrence.
- When you experience pain during active or resistant plantar flexion, or when you feel tenderness when you palpate the back of your lower leg, it’s a sign of soleus muscle pain. You may also have pain when you walk, jump, or run.
- There are numerous causes of this muscle pain, including strains and pain.
- Along with the agony, you can also see the redness and swelling.
- The RICE concept, painkillers, and physical therapy are used to relieve this pain.
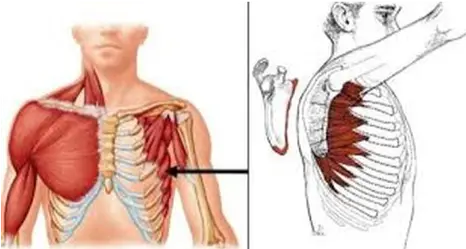
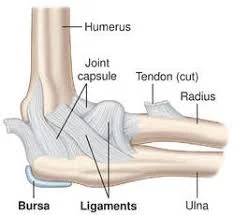
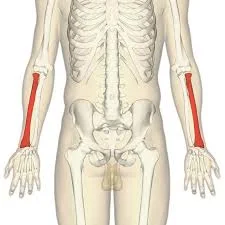
Anatomy of the Soleus muscle?
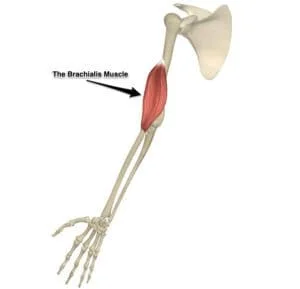
- Large and located on the rear of the lower thigh is the soleus muscle.
- As a component of the Achilles tendon, this strong muscle connects to the heel bone after emerging from the rear of the shin bone.
- Walking, running, and jumping are exercises that activate this soleus muscle.
- The soleus muscles are responsible for plantarflexing the foot.
- Many experts believe that the soleus muscle and the two heads of the gastrocnemius muscle combine to form the triceps surae, a single muscle group.
Causes of the Soleus muscle pain?
- pain to the soleus muscle are somewhat prevalent in runners. An overuse pain is what this runner’s pain is called.
- Fatigue or overuse of the muscle during the activity is the cause of this pain.
- A muscular strain happens when the workload imposed on the muscle during an activity damages the muscle fibers.
- Muscle strain is frequently cited as the cause of the pain when it is progressively raised, and MOI is frequently the lack of a clear mechanism of pain.
- The intramuscular aponeurosis’s restricted sensory innervation may be the cause of this strain.
- Grade 1 muscle strain:
- During the action, you initially experience pain and sharpness.
- You don’t feel pain, but you do experience some mild pain.
- Occasionally, you may also have muscle tightness.
- Grade 2 muscle strain:
- During an activity, you experience pain and sharpness, making it impossible to continue.
- Additionally, you experience pain after any activity and when you walk.
- You notice that the area of muscle soreness is swollen and that the skin there is bruised or discolored.
- Grade 3 muscle strain:
- The anguish you are experiencing is too much.
- Unable to perform the exercise
- Long periods of knee flexion during running exercises might also cause this muscle soreness.
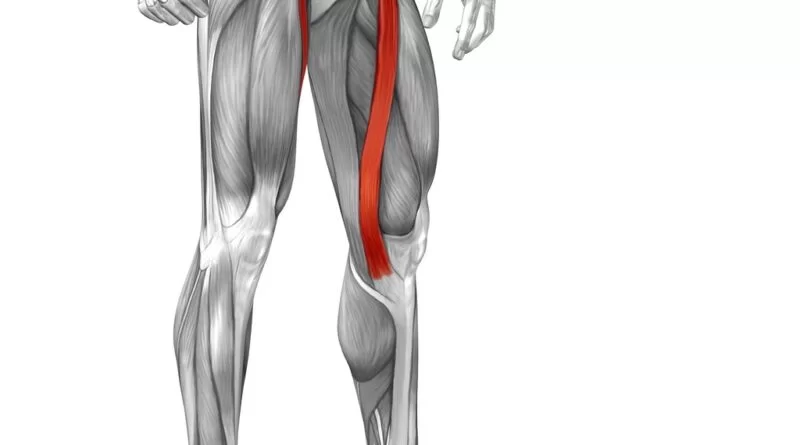
- Other calf muscle pain, such as gastrocnemius muscle strains, which are more common in sports, particularly tennis players, can also cause soleus muscle pain.
Symptoms of the Soleus muscle pain?
- The location of your muscles hurts.
- Additionally, you have pain both during and after the action.
- The walking, leaping, and running exercises also cause this muscle soreness.
- You are seeing that the area of muscle soreness is red and swollen.
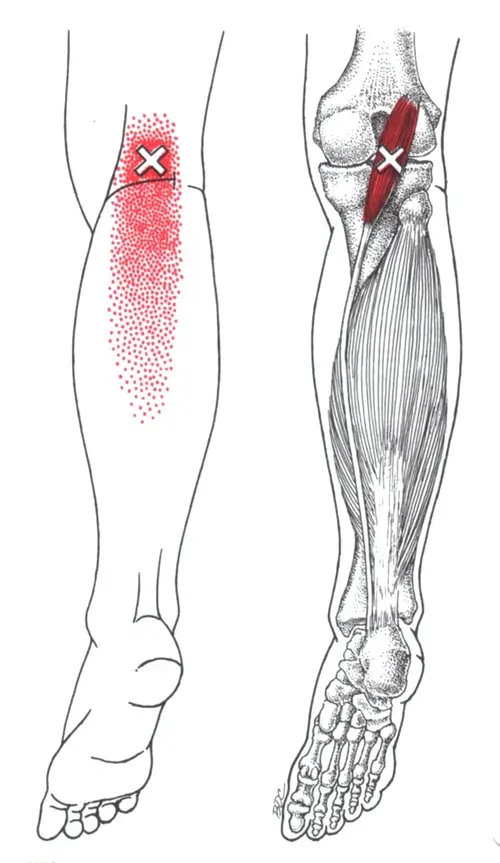
- The location of muscle soreness can occasionally have trigger and sensitivity points.
- Additionally, you get muscle tension.
- During muscle exercise, weakness is also felt.
Diagnosis of the Soleus muscle pain?
- Identifying this muscle pain just through physical examination becomes too difficult.
- Therefore, to confirm the diagnosis of the muscle pain, clinicians usually utilize an MRI and ultrasound.
- USG is less effective in identifying this kind of muscle pain than ultrasound.
- Inquiring into the patient’s symptoms and the reasons behind the pain are other things the doctor does.
What is the treatment for Soleus muscle pain?
The doctor suggests using the RICE method to relieve muscular pain and swelling when you have pain in the soleus muscle during the early stages of muscle pain.
- R-rest = The doctor advises you to take a few days off from activities that cause muscle pain and to use crutches for a few days if you are unable to bear weight.
- I-ice = You can also apply an ice pack and frozen peas to the area of pain, but always use a towel to prevent ice burns.
- C-compression = Compression bandages can also be applied to the area of muscle soreness to reduce swelling and spam.
- E-elevating: To relieve the pain, place pillows beneath your foot to raise yourself to the location.
Pain medication:
- Aspirin and ibuprofen (Advil, Motrin) are examples of non-steroidal anti-inflammatory medicines (NSAIDs) that can assist relieve muscle pain.
- Additionally, you can use volini gel and spray to relieve muscle soreness.
Physical Therapy Treatment for the Soleus muscle pain?
Physical therapy helps you get rid of muscle pain, tightness, edema, and spasms.
Stretching, electrotherapy, massage, and strengthening exercises are all part of the physical therapy treatment.
Massage:
- When soleus muscle pain manifests as trigger points and sore spots during physical therapy, the therapist is recommended to massage the affected area.
- It is applied to the sore spot on the muscle for five to ten minutes using oil and powder. The main purpose of effleurage massage is to relieve muscle soreness.
- A circular motion is used to apply it.
- It is also used with a messenger’s assistance.
Electrotherapy treatment:
- Use US (ultrasound therapy) to relieve muscle pain when trigger points and tender points are present.
- You can reduce pain and swelling with this electrotherapy treatment.
- lessen pain It is recommended that the therapist apply TENS (transcutaneous electrical nerve stimulation), IFT (interferential therapy), and SWD (short wave diathermy) to the painful location.
- Transcutaneous Electrical Nerve Stimulation (TENS) and Interferential Therapy (IFT) are applied to the area of muscle soreness using gel and electrodes.
- Both treatments are given to the painful area for ten minutes.
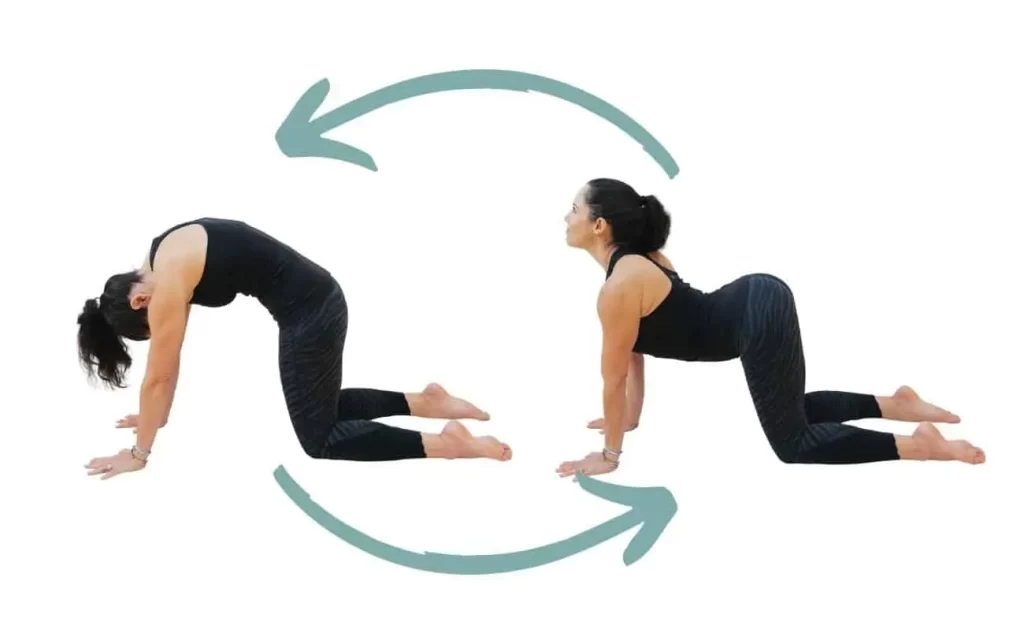
Stretching of soleus muscle:
- Soleus Stretch (Flexibility):
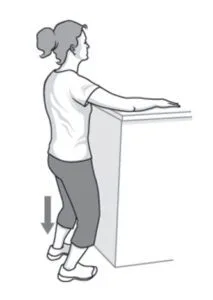
- Standing Soleus Stretch:
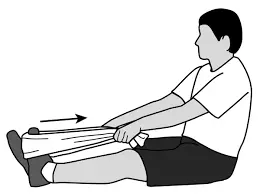
- Soleus seated bent-knee stretch:
- Soleus bent knee standing wall strech:
Soleus Stretch (Flexibility):
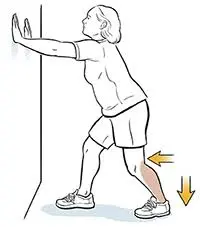
- Next, take a single step with your right foot toward the direction of the wall.
- Touch the wall with both palms.
- Lean forward and bend both knee joints.
- Surely Both heels should remain on the ground.
- For 30 to 60 seconds, hold this position. Then let both legs relax.
- Do the workout three times.
- Next, switch legs and do it again.
- Three times a day, repeat this stretching exercise.
Standing Soleus Stretch:

- For the stretch, you are standing and taking a half-step forward.
- Surely Maintain a balanced weight distribution on the ground across both feet and heels.
- The back leg, just above the heel, should feel stretched in this position.
- Then, to extend the stretch, keep lowering the hip joint gradually.
- After 30 seconds of holding this stretching stance, switch sides.
- The soleus and Achilles tendon are stretched when you bend your knee joint, not your gastrocnemius muscle.
Soleus seated bent-knee stretch:
- Bend one knee joint while sitting on the floor and raise your toes toward the ceiling.
Wrap a towel and band around the foot’s center. - Repeat this exercise on the opposite side after holding it for the desired amount of time.
Soleus bent knee standing wall strech:
- Lean one leg back with the knee straight and place both hands against the wall.
To feel a stretch in your rear leg, bend both knees. - After holding this stretch for the required amount of time, switch sides or do it again.
Exercise:
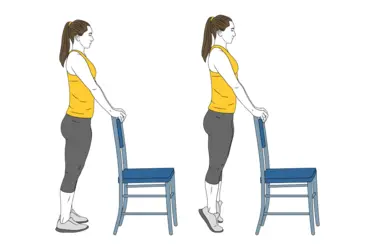
- Calf raises
- Standing heel calf raise
- Soleus bridge
- Squat with soleus raise
- Donkey calf raise
- Standing upright, the patient pushes through the balls of their feet and lifts their heel till they are standing on their toes. Then slowly return to the beginning by lowering.
Calf raise variations:
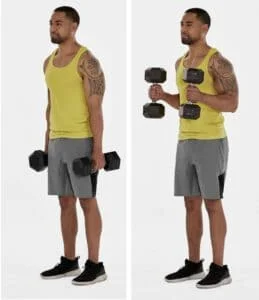
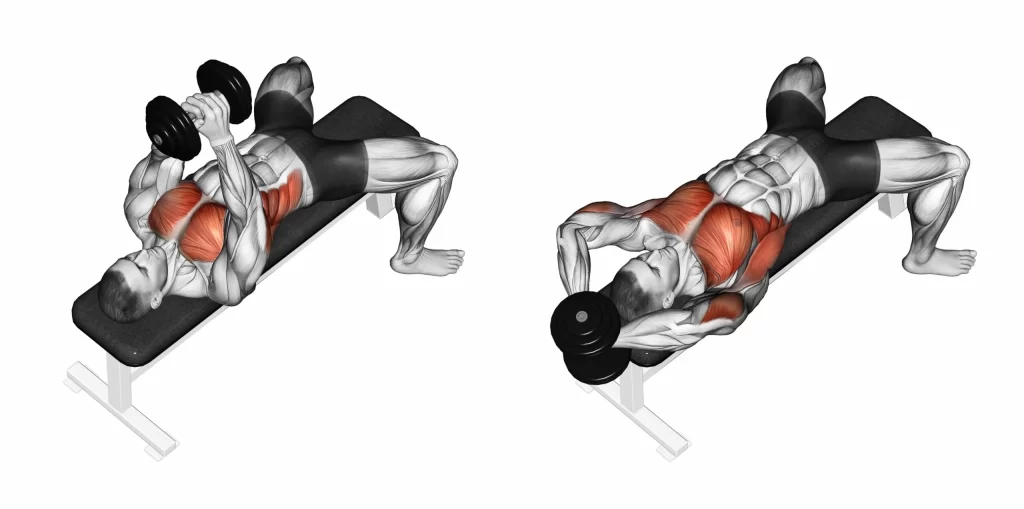
Weighted calf raise:
- Using weights to accomplish the calf raises is a smart way to make the exercise more challenging.
- In order to train the calf muscle to withstand the additional pressure throughout the exercise, the patient is performing calf raises while holding a dumbbell in each hand.
Raised calf raise:
- At the bottom of the movement, you are standing on a step with your heel lowering below the rest of your foot.
- To make this variant more challenging, you can hold the dumbbells, but it is challenging to maintain balance when doing so.
Bent-knee calf raise:
- When performing any type of calf raise, which is primarily employed for the soleus muscle, the knee joint should be slightly bent.
Seated calf raise:

- For the latter, you can increase the movement’s resistance by resting weights on your knee joint.
- The soleus muscles are mostly worked by seated calf raises, which also let you add a lot of weight to the exercise without worrying about losing your balance.
Standing heel calf raise:
- Standing at the beginning of this exercise is followed by holding onto a sturdy surface for support.
- After that, slowly lift your heels as high off the ground as you can and bring them down to the floor.
- Next, perform this exercise three times a day and ten times in a single session.
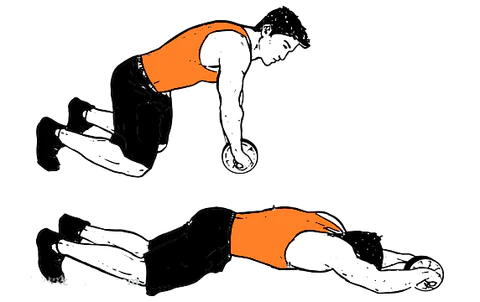
Foam Roller Exercise:

- The roller should then be positioned beneath the calves.
- Support yourself with your hands, then carefully roll from your knee to your ankle, stopping when you reach any tight or painful areas.
- Perform this roll five times in a single session and three times a day for 30 to 1 minute.
Soleus bridge:
- The patient sets the balls of their feet on a raised surface, such as a weight plate or foam roll, while they are supine on the floor.
- Next, extend your hips and compress your glutes to achieve the glute bridge position.
- Perform a calf lift while in the top position and take a little break.
- Next, reset and reverse the movement.
Squat with soleus raise:
- With both hands, your torso upright, your feet hip-width apart, and your toes pointed front, you are holding a squat rack.
- To safely lean back, you can alternatively wrap a band around your waist and hook it to a pole or other substantial object.
- It enables you to squat down while maintaining your shins perpendicular to the floor.
- Next, pull yourself up onto your toes to perform a calf raise.
- After 30 seconds of holding, heel back to the floor.
- After that, get out of the squat and reset.
Donkey calf raise:

- After that, bring the heels as close to the floor as you can and hold them there for 30 seconds.
Strengthening exercise:
- Strengthening exercise for soleus muscle
- Bending the knee on a step
- Seated soleus raises with weight
Strengthening exercise for soleus muscle:
- Your feet are shoulder-width apart when you stand.
- Make sure you are alert and attentive.
- If necessary, use a wall and a chair for support.
- Perform two to three sets of 10 to 20 repetitions per day.
- Try performing this exercise on one leg to make it more difficult.
Bending the knee on a step
- Your heels are dangling over the edge of the stair you are standing on.
- For stability, hold the object.
- Next, bend your knee joint as close to 90 degrees as you can while standing on the leg you wish to use for exercise.
- Then, elevate yourself to your toes and slowly lower yourself back down until your calf muscle stretches, then repeat.
- Add weight to the hand if you are prepared to perform this exercise more than once.
- Next, pick a resistance that is low for endurance and high for strength.
- To build strength, complete this exercise for 6–10 repetitions and 3-5 sets overall.
- You perform this exercise for 15–25 repetitions and repeat for 3–5 sets to build endurance.
- For strength, you must rest for at least three minutes in between sets, and for endurance, you must rest for no more than thirty seconds.
- It is required that you aim the task two or three times a week.
Seated soleus raises with weight:
- There are three ways to perform this exercise: isometric, eccentric, and concentric.
- This exercise’s isometric variant:
- Holding this right foot tiptoe stance for up to 30 seconds is the goal of this exercise.
- The weight must then be sufficiently heavy to permit no more than 30 seconds.
- You will increase the weight after you have completed this exercise for 30 seconds and feel stronger.
- This exercise’s eccentric variation entails maintaining the right foot tiptoe posture for two seconds.
- The heel is then gradually lowered back over the step’s edge for three seconds.
- To repeat, lift the weight with both feet, hold and descend with one foot, and so on.
- The weight must be sufficiently heavy to permit no more than twelve repetitions.
- After completing the 12 reps and feeling more resilient, you can increase the weight.
- This workout in a concentric form
- Exercise entails lifting and lowering the weight with just one foot.
- Surely Use adequate weight and maintain a slow, regulated cadence to allow for no more than 12 repetitions.
- After completing the 12 reps and feeling more resilient, you can increase the weight.
FAQs
How can I make my soleus stronger?
What Are the Bes Exercises for the Soleus? The soleus training regimen isn’t that exciting, to be completely honest. As previously indicated, do calf lifts with your knee bent to 90 degrees to strengthen your soleus. That’s all.
What impact does Soleus have?
The only consequences theory is a school of thought in investment law study and jurisprudence that states that tribunals should base their decisions primarily, if not completely, on how the contested measure affected the investment when evaluating indirect expropriation claims.
Does the soleus muscle get used while you walk?
Each of your lower legs contains two soleus muscles. The soleus muscle is used for walking, running, and jumping, and its pain may impair your capacity to carry out these fundamental movements.
Can someone who has soleus pain run?
Ignoring the pain could make it worse. Walking, jogging, and even running may make your symptoms worse.
Does a soleus strain affect your ability to walk?
Short walks are beneficial for the mending muscle, but stay away from extensive walks and standing for extended periods of time. If there is a handrail, utilize it.
How long does it take for soleus to recover?
It takes roughly four weeks for mild calf strains to heal. It may take more than 12 weeks to resume your normal exercise after suffering from severe calf rips.
How can soleus pain be relieved?
Treatment Rest.
Ice: To lessen pain and inflammation, apply ice to the affected area.
Compression: To stop swelling, apply a medical bandage to the affected area.
Elevation: To lessen pain and bruises, keep the leg as high above the heart as you can.
How is the soleus test conducted?
Test of Soleus increase endurance
Do the wall sit as described above, shift your weight to one leg, stand up on your toes, and maintain this position for as long as you can to complete this test. Take your time on each leg.
Does the soleus muscle get used while you walk?
Each of your lower legs contains two soleus muscles. The soleus muscle is used for walking, running, and jumping, and its pain may impair your capacity to carry out these fundamental movements.
Should a soleus pain be massaged?
Applying massage during the first 24 to 72 hours after a strain will worsen the pain, increase bleeding, and hinder healing. Once the acute healing phase is over, massage can assist relax muscle spasms, mobilize muscle fibers, and increase blood flow.
What signs of a tight soleus muscle are present?
In addition, compared to gastrocnemius pain, soleus strains typically appear clinically as more subacute and less dramatic. Calf pain, stiffness, and tightness that becomes worse over days to weeks is the typical appearance. Jogging or walking frequently causes symptoms.
How much time does it take for a strain of the soleus to heal?
Various grade degrees of strain in the calves
Although the muscle may be sore and provide some slight pain or pain, its strength and range of motion are normal, and the internal bleeding is minimal. The most prevalent kind of strain usually takes one to three weeks to recover from.
How is pain in the soleus muscles treated?
Useful Remedies for Soleus Muscle Pain: Applying ice and resting right away.
targeted stretching of the soleus muscle.
exercises that gradually increase strength.
massage therapy.
References
- Ladva, V. (2022d, May 12). Soleus muscle pain: Cause, Symptoms, Treatment, Exercise – Samarpan P. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/soleus-muscle-pain-treatment/
- Physiotherapy, P., & Physiotherapy, P. (2023, September 25). Soleus Muscle Pain | PrimeCare Physiotherapy. PrimeCare Physiotherapy. https://primecarephysio.ca/soleus-muscle-pain/