Introduction
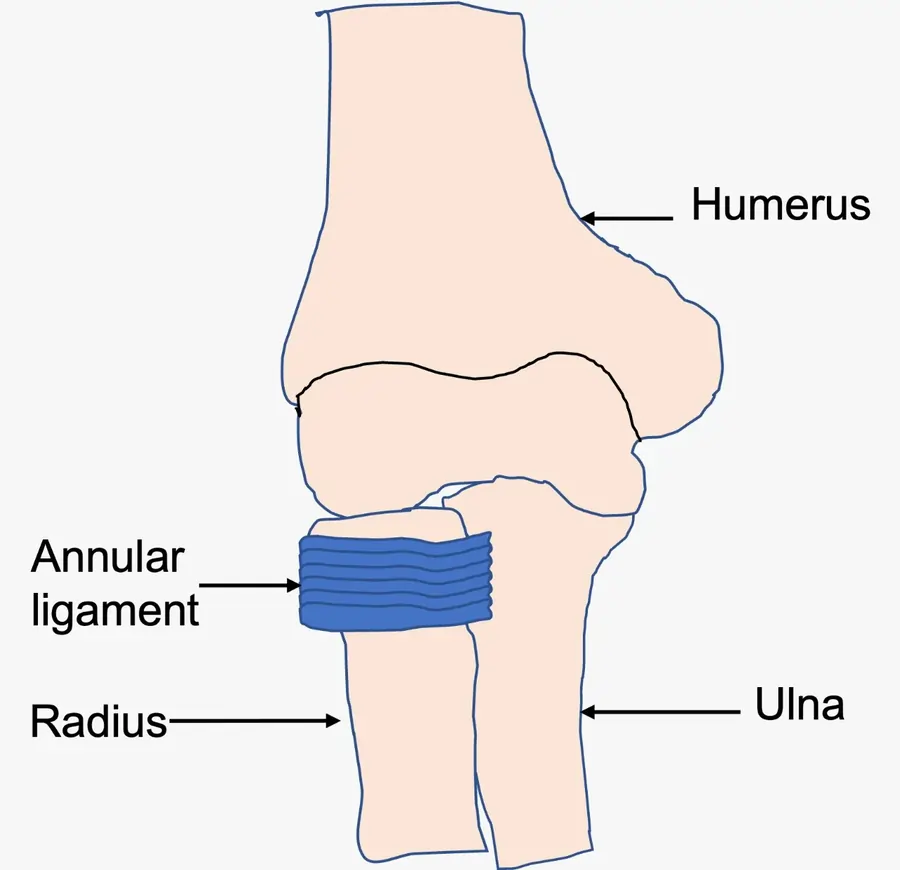
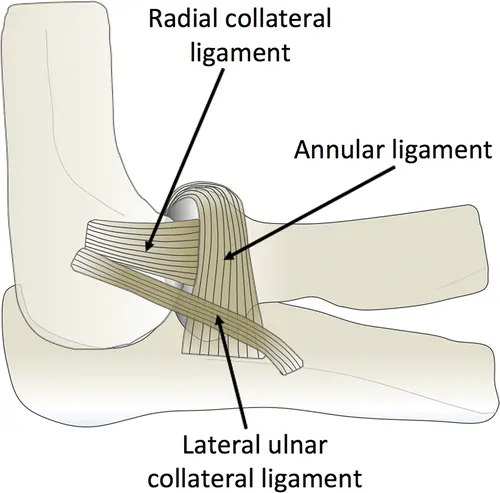
The annular ligament is a strong, circular band of fibrous tissue that wraps around the head of the radius, securing it to the ulna at the proximal radioulnar joint. It allows the radius to rotate smoothly during forearm movements like pronation and supination while maintaining joint stability.
The annular ligament is made of thick connective tissue and is attached to the radius bone on one end and the ulna bone on the other. It is crucial for preserving elbow joint stability and permitting fluid forearm motion. If the annular ligament becomes injured or dysfunctional, the elbow joint may experience pain, instability, and a restricted range of motion.
Structure of the Annular Ligament
In the elbow joint, the head of the radius bone is surrounded by a fibrous band called the annular ligament. Attached to the radius bone on one end and the ulna bone on the other, it is a circular structure. The ligament’s strength and stability come from its dense connective tissue composition.
The radial notch of the ulna bone, a depression on the lateral side of the ulna, is surrounded by the annular ligament. The proximal radioulnar joint is formed when the head of the radius bone slides into this notch. The radius bone’s head is held in place and given rotational motion during forearm movements by the annular ligament.
The proximal and distal portions of the annular ligament are its two components. Attached to the ulna bone, the proximal portion is stronger and thicker than the distal portion. The distal portion, which is connected to the radius bone, is thinner and more flexible than the proximal portion.
Some structures support the annular ligament, which aids in elbow joint stability. These include the oblique cord, which joins the annular ligament to the radius bone, and the quadrate ligament, which joins the annular ligament to the ulna bone.
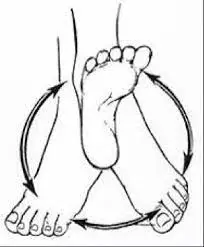
The stability of the elbow joint and the ability to move the forearm smoothly are both dependent on the annular ligament. The annular ligament permits the head of the radius bone to rotate inside the radial notch of the ulna bone during pronation and supination. The elbow joint may experience pain, instability, and a restricted range of motion if the annular ligament becomes injured or dysfunctional.
Attachments of the Annular Ligament
On one end, it is connected to the ulna bone, and on the other, to the radius bone. The quadrate ligament, a thickened band of connective tissue that extends from the medial border of the ulna bone to the annular ligament, is where the annular ligament is attached to the ulna bone. The elbow joint is further stabilized by the quadrate ligament, which supports the annular ligament.
The oblique cord, a thin band of connective tissue that extends from the lateral aspect of the ulna bone to the annular ligament, is where the annular ligament attaches to the radius bone. By supporting the distal portion of the annular ligament, the oblique cord preserves its suppleness and permits fluid forearm movements.
Additionally, the supinator crest, a bony ridge on the lateral aspect of the radius bone, is where the annular ligament attaches to the bone. The radius bone is held in place and given the ability to rotate during forearm movements by the annular ligament, which adheres to this bony ridge and wraps around its head.
Generally speaking, the elbow joint is stabilized and the forearm can move smoothly due to the annular ligament’s attachment to the ulna and radius bones. Elbow joint pain, instability, and restricted range of motion can be caused by injury or failure to any of these attachments.
Functions of the Annular Ligament
The elbow joint’s stability and range of motion are greatly influenced by the annular ligament.
These primary roles are:
- Stabilization: The head of the radius bone is held in place within the elbow joint by the annular ligament. This is significant because when the forearm moves, the radius bone revolves around the ulna bone. The head of the radius bone may slip out of position without the annular ligament, causing pain and instability.
- Flexibility: The annular ligament must be sufficiently flexible to permit fluid forearm movements even though it offers stability. The annular ligament can still flex and rotate as needed thanks to the support of the oblique cord and supinator crest attachments.
- Protection: The joint is shielded from undue wear and tear by the annular ligament. It stops the radius bone’s head from rubbing against other bones or soft tissues in the joint by holding it in place.
- Force transmission: The elbow joint is where forces are transferred during gripping and twisting activities. By distributing these forces uniformly throughout the joint, the annular ligament lowers the risk of injury.
Thus, in general, the elbow joint’s annular ligament is an essential component that offers protection, flexibility, stability, and force transmission. Elbow joint pain, instability, and restricted range of motion can result from injury or dysfunction to this ligament.
Injuries of the Annular Ligament
Numerous activities that strain the elbow joint can result in annular ligament injuries. The following are a few typical reasons for annular ligament injuries:
- Repetitive motions: The annular ligament and surrounding tissues may be severely strained by sports like tennis or baseball that require repetitive motions of the elbow joint. This can raise the risk of injury and cause the ligament to weaken over time.
- Trauma: The annular ligament may be harmed by trauma to the elbow joint, such as a fall or a direct blow to the arm. Activities involving high-impact or contact sports are more likely to cause this kind of injury.
- Overuse: Ankle ligament injuries can also result from excessive elbow joint use, such as lifting heavy weights or typing a lot. This is because these activities continuously strain the ligament, which over time may result in inflammation or tearing.
- Inappropriate technique: Inappropriate technique can also raise the risk of annular ligament injuries when engaging in specific activities, such as lifting weights or playing sports. This is because improper form can cause the elbow joint and surrounding tissues to experience more stress.
Therefore, it’s critical to take precautions against annular ligament injuries by using appropriate techniques when performing tasks, taking breaks to rest and stretch the elbow joint, and getting medical help if you experience any pain or discomfort.
Symptoms of the Annular Ligament Injury
Depending on how severe the injury is, annular ligament injuries can present with a variety of symptoms, but some typical ones include:
- Elbow Pain: One of the most typical signs of an annular ligament injury is elbow joint pain. When engaging in activities that strain the elbow joint, one may experience either dull or sharp pain.
- Swelling: Another typical sign of an annular ligament injury is swelling around the elbow joint. In addition to mild to severe swelling, the affected area may also be warm or red.
- Stiffness: Another sign of an annular ligament injury is stiffness in the elbow joint. It may be challenging to move the arm or carry out specific tasks due to the mild to severe stiffness.
- Weakness: An annular ligament injury can also cause weakness in the affected arm. This can make it difficult to use the arm normally and could be caused by pain or ligament injury.
- Clicking or popping: Another sign of an annular ligament injury is clicking or popping sounds coming from the elbow joint. The joint may move abnormally as a result of a ligament tear or another injury.
Therefore, it is crucial to seek medical attention if you experience any of these symptoms to identify the cause and obtain the proper treatment.
Diagnosis
Imaging tests and a physical examination are usually required to diagnose an annular ligament injury.
The physician will assess the affected arm and elbow joint during the physical examination, looking for indications of discomfort, stiffness, and edema. They might also test for weakness or instability by moving the elbow and arm joints in various directions.
An annular ligament injury may also be diagnosed by imaging studies like MRIs, ultrasounds, or X-rays. While MRI or ultrasound can demonstrate the extent of ligament injury, X-rays can assist in ruling out other disorders such as fractures or dislocations.
A tiny camera is inserted into the joint to assess the annular ligament and surrounding components during an arthroscopy, which the doctor may also do in certain cases. This can provide a more complete diagnosis and help determine the best process of treatment.
An annular ligament injury is therefore usually diagnosed and the best option for therapy is decided by a comprehensive physical examination and imaging testing.
Treatment of the Annular Ligament Injury
Two methods are available for treating the annular ligament:
- Conservative treatment
- Physiotherapy treatment
Conservative treatment
RICE, or rest, ice, compression, and elevation, is the standard conservative treatment for an annular ligament injury. This may lessen the wounded area’s discomfort and swelling.
Avoiding activities that exacerbate the pain and resting the affected arm can help stop the annular ligament from getting worse. To lessen swelling and inflammation, use cold compresses or ice packs on the area for 15 to 20 minutes at a time, multiple times a day.
Using a brace or bandage to compress the injured area can also assist in reducing swelling and provide support. Reducing edema and accelerating healing can also be achieved by elevating the arm above the level of the heart.
To treat pain and inflammation, nonsteroidal anti-inflammatory medicines (NSAIDs) or painkillers like acetaminophen may also be suggested.
To help increase the affected arm’s strength, flexibility, and range of motion, physical treatment may also be suggested. Exercises to strengthen and extend the muscles around the elbow joint may be part of this, as well as manual therapy methods like joint mobilization or massage.
A brace or splint may be advised in some situations to immobilize the affected arm and promote the healing of the annular ligament. If conservative treatment fails to provide sufficient relief or if there is a possibility of more harm, this might be required.
Therefore, minimizing discomfort and inflammation, encouraging healing, and regaining function in the injured arm are the ultimate goals of conservative treatment for an annular ligament injury.
Physiotherapy treatment
Exercises, manual therapy methods, and other modalities are commonly used in physiotherapy treatment for annular ligament injuries to assist in decreasing pain and inflammation, increasing the range of motion, and restoring function to the injured arm.
The physiotherapist will first perform a comprehensive evaluation of the injury to as certain the degree of harm and create a customized treatment strategy. These could consist of:
- Immobilization and rest: To promote the healing of the annular ligament during the acute stage of the injury, the physiotherapist could advise immobilizing that affected arm using a brace or splint.
- Ice therapy: Applying cold compresses or ice packs to the affected region might help to reduce swelling and pain.
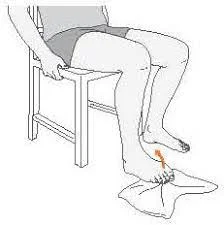
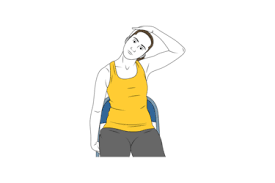
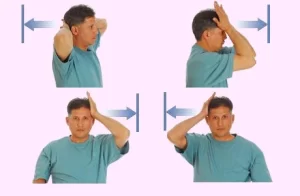
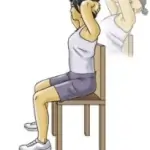
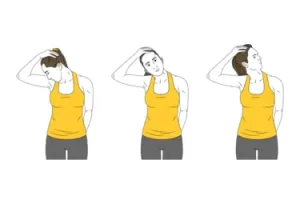
- Manual treatment: Manual therapy methods that help increase the range of motion and ease muscular tension around the elbow joint include massage, joint mobilization, and stretching.
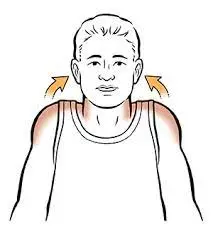
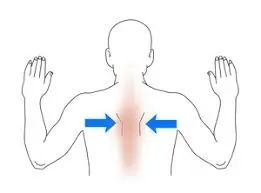
- Strength training: By strengthening the muscles that surround the elbow joint, you can increase stability and stop additional injuries.
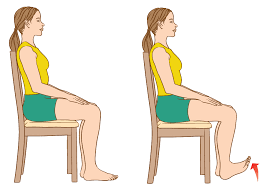
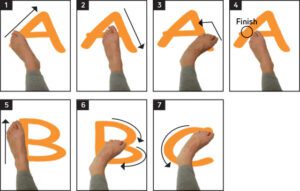
- Exercises for range of motion: These exercises can assist increase the affected arm’s flexibility and range of motion.
- Ultrasound therapy: Ultrasound therapy uses high-frequency sound waves to help the wounded area heal and to lessen pain and inflammation.
- Electrical stimulation: This technique can be used to increase muscular strength and function and lessen pain.
As the process of therapy progresses, the physiotherapist will keep an eye on things and modify the plan as necessary to ensure the best possible outcomes. Most patients with an annular ligament injury can anticipate a major improvement in their quality of life, function, and discomfort with appropriate physiotherapy treatment.
Risk factors of the annular ligament
In the forearm, the head of the radius bone is surrounded by a band of tissue called the annular ligament, which helps hold it in place within the elbow joint. Although the annular ligament is a robust and durable structure, many risk factors might raise the possibility of an injury, such as:
- Overuse: The annular ligament may sustain injury as a result of repetitive motions of the forearm and elbow, such as those found in sports like tennis or golf.
- Trauma: The annular ligament may stretch or rupture as a result of direct trauma to the elbow joint, such as a fall or impact.
- Age: As we get older, our tissues lose their elasticity and become more vulnerable to injury. Older folks may be more vulnerable to annular ligament injury.
- Genetics: Some people may have weaker or more flexible ligaments from birth, which increases their risk of injury.
- Bad posture: Bad posture can increase the strain on the elbow joint and the ligaments that surround it, such as the annular ligament.
- Poor technique: When playing sports or engaging in other physical activities, poor technique might raise the risk of injury to the annular ligament and other elbow joint tissues.
- Medical problems: The annular ligament can become weaker and more prone to injury due to certain medical diseases, such as osteoarthritis or rheumatoid arthritis.
- Poor nutrition: The body’s tissues can become weaker and the risk of injury to the annular ligament and other elbow joint components increases if a diet is deficient in vital nutrients like protein and vitamin C.
Understanding these risk factors and taking action to mitigate them is essential to lowering the risk of an annular ligament injury. Keeping perfect posture, exercising with the right form, and eating a healthy, balanced diet are a few examples of how to do this.
How can injuries in the annular ligament be prevented?
A mix of lifestyle modifications, appropriate form when exercising, and medical treatment of underlying issues are necessary to prevent annular ligament injuries. The following advice can help avoid injury to the annular ligament:
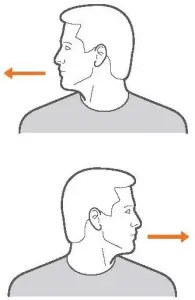
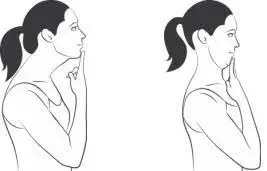
- Maintain proper posture: Bad posture can increase the strain on the elbow joint and the ligaments that surround it, such as the annular ligament. When standing, sitting, and engaging in physical activity, keep your posture correct to avoid injury.
- Employ good form when exercising: Employ good form when exercising: In sports or other physical activities, poor form can raise the risk of injury to the annular ligament and other elbow joint tissues.
- Stretch before exercising: Stretching before exercising can assist your muscles warm up and keep you from getting hurt. Stretching your wrist, elbow, and forearm muscles will help them get ready for action.
- Develop your forearm muscles: Strong forearm muscles can lower the risk of annular ligament injury and support the elbow joint. Incorporate forearm-focused exercises into your training regimen.
- Wear the proper protective equipment: If you play contact sports or other high-risk hobbies like rock climbing, wearing elbow pads or other protective gear can help you avoid getting hurt.
- Handle underlying medical disorders: The annular ligament might become weaker and more prone to injury due to certain medical illnesses including osteoarthritis or rheumatoid arthritis. To manage any underlying conditions that could raise your risk of injury, collaborate with your healthcare physician.
- Keep up a healthy, well-balanced diet: A diet deficient in vital nutrients, such as protein and vitamin C, can weaken bodily tissues and raise the risk of injury to the elbow joint’s annular ligament and other components. Maintain a healthy, well-balanced diet rich in fruits, vegetables, lean protein, and whole grains to help prevent injury.
You can lower your risk of suffering an annular ligament injury or another elbow joint injury by adopting these lifestyle changes. See a doctor right away if you have elbow pain or discomfort to stop further injury and encourage recovery.
FAQs
The annular ligament: what is it?
The head of the radius bone is held in place within the elbow joint by a band of fibrous tissue called the annular ligament.
In what part of the body is the annular ligament located?
The elbow joint contains the annular ligament, which is situated around the radius bone’s head.
What is the annular ligament used for?
Smooth forearm movement is made possible by the annular ligament, which stabilizes the head of the radius bone within the elbow joint.
Which disorders or traumas are frequently linked to the annular ligament?
Chronic elbow joint instability, radial head subluxation (partial dislocation), and annular ligament tears are common injuries or disorders related to the annular ligament.
How are annular ligament disorders and injuries identified and managed?
A physical examination, imaging tests (such as MRIs or X-rays), and occasionally an arthroscopy are used to detect annular ligament injuries or disorders. Depending on the severity of the injury, treatment options may include physical therapy, surgery, immobilization, or rest.
What precautions may be taken to keep the annular ligament from getting injured?
Wearing protective clothing during activities that put the elbow joint in danger, avoiding repetitive actions that strain it, and maintaining strong forearm muscles through training are all ways to prevent injuries to the annular ligament.
References
- Patel, D. (2023e, August 19). Annular ligament – anatomy, structure, function. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/annular-ligament/