Osteoporosis
Osteoporosis is a condition characterized by weakened bones that become fragile and more prone to fractures. It occurs when bone density and quality decrease, often due to aging, hormonal changes, or nutritional deficiencies.
Common risk factors include lack of calcium and vitamin D, sedentary lifestyle, smoking, and genetic predisposition. Prevention and management focus on weight-bearing exercises, a nutrient-rich diet, and, in some cases, medication to maintain bone strength.
Introduction:
The medical disorder known as osteoporosis is defined by the weakening of bones, which increases the risk of fractures. It is frequently called a “silent disease” because, until a bone fracture happens, there usually are no symptoms. This condition is most prevalent in elderly persons, particularly in postmenopausal women. However, people of any age or gender might be affected.
Live tissue, such as bone, is continually being broken down and replaced. When the production of new bone isn’t keeping up with the loss of existing bone, osteoporosis develops.
Men and women of every background are affected by osteoporosis. However, Asian and black women are more at risk, particularly older women who have passed menopause. Weight-bearing activity, a nutritious diet, and medications can help strengthen weak bones or stop bone loss.
What Is Osteoporosis?

Osteoporosis arises from either limited new bone formation or excessive bone mass loss. Due to the loss of bone tissue caused by this imbalance, bones become weaker and more likely to fracture. Bones lose strength and density when the rebuilding process is out of balance, increasing the chance of fractures.
Although any bone can fracture, osteoporosis most frequently affects the wrists, hips, and spine. The quality of a person’s life can be greatly affected by these fractures, which can cause pain, inability, and in extreme situations, death.
Due to lower estrogen levels, osteoporosis mainly affects older persons, especially postmenopausal women, although it may also affect men and younger people, especially if there are additional risk factors.
There are various kinds, which are categorized according to the characteristics and causes of bone loss. The main types are:
Primary Osteoporosis
- Type 1 (Postmenopausal Osteoporosis): This type mainly affects women after menopause because estrogen, which is important for bone density, decreases. Frequently, it leads to wrist and spine fractures.
- Type 2 (senile osteoporosis): This kind usually begins to affect both men and women around the age of 70. It is linked to a slow decline in bone density caused by age, which frequently results in fractures of the hip and spine.
Secondary Osteoporosis
This sort of condition of condition comes from medications or other health issues that restrict bone growth. Among the frequent reasons are:
- Hormonal conditions (such as hyperparathyroidism and hyperthyroidism)
- Medications (such as anticonvulsants and corticosteroids)
- Chronic conditions (such as diabetes, liver disease, and rheumatoid arthritis)
- Factors related to lifestyle (such as smoking and drinking excessively)
- Shortages in some nutrients, such as a lack of calcium or vitamin D
Juvenile Osteoporosis
Children and teenagers are prone to this uncommon type of osteoporosis. It may be caused by medication, genetic disorders, or underlying medical diseases such as juvenile arthritis.
Causes:
Numerous factors could affect bone density and strength, leading to osteoporosis.
- Growing older
Natural bone loss: Bone loss, or the breakdown of bone, usually exceeds bone formation, which causes people’s bone density to decline with age. Beyond the age of 30, this is very common, and women lose more bone following menopause due to a decrease in estrogen.
- Gender
Being a woman increases your risk of getting osteoporosis. Women’s bones are thinner and their maximal bone mass is lower than men’s. However, men are still at risk, especially after the age of 60 to 70.
- Genetics
Family history: You may be more at risk if your parents or grandparents suffer from osteoporosis or bone fractures. Bone strength and density can be affected by genetic factors.
- Changes in Hormones
Menopause: After menopause, women’s estrogen production declines, which significantly speeds up bone loss.
Testosterone deficiency: In men, bone loss may also result from a drop in testosterone levels, which is frequently associated with aging.
Thyroid issues: Too much thyroid hormone treatment or an overactive thyroid (hyperthyroidism) can cause bone weakening.
- Medicines
Long-term use of some medicines: If taken for an extended length of time, certain medications, like corticosteroids (prednisone), can cause bone loss. Bone health can also be affected by other medications, such as specific anticonvulsants or cancer treatments.
- Low Nutrition
Calcium deficiency: Strong bones require calcium. Over time, a lack of calcium can cause bones to break down.
Deficiency of vitamin D: Vitamin D facilitates calcium consumption in the body. Vitamin D deficiency can cause bones to break down.
Poor nutrition: Bone health can be seriously affected by a diet deficient in important nutrients (such as protein, magnesium, and other vitamins).
- Lack of Physical Activity
Sedentary lifestyle: Bone density is maintained by regular exercise, particularly weight-bearing activities like running, walking, or strength training. Bone weakening results from inactivity.
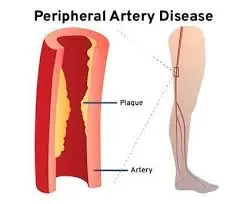
- Factors of Lifestyle
Smoking: Smoking raises the risk of osteoporosis by weakening bones and reducing blood flow to them.
Excessive consumption of alcohol: Excessive consumption of alcohol may affect bone formation and intake of calcium.
- Health Problems
Chronic illnesses: Several illnesses, including diabetes, kidney disease, and rheumatoid arthritis, can raise the risk of osteoporosis.
Gastrointestinal disorders: Disorders such as inflammatory bowel disease (IBD) or celiac disease can interfere with the intake of nutrients, resulting in shortages that affect bone health.
- Minimal Body Weight
Small body: People who weigh less and have a smaller body may have less bone mass in the beginning, which raises their chance of developing osteoporosis as they age.
Signs and symptoms:
There are usually no obvious warning signals in the early stages, but as the illness progresses, certain symptoms may appear.
These include:
- Breaking bones, or fractures
Bone fractures that happen more frequently than expected, even with mild accidents or traumas, are the most common signs of osteoporosis. Typical fracture sites include:
Spine: Vertebral (or spine) compression fractures are frequent. Over time, this may result in a slumped posture or a loss of height.
Hip: People with osteoporosis may find it more difficult to recover from a broken hip, which often happens after a fall.
Wrist: Fractures may result from falls onto an outstretched hand.
- Back Pain
A compression fracture in the spine or a broken vertebra can cause severe back pain. The pain may not go away and may get worse when you move or do specific things.
- Decrease in Height
The vertebrae may collapse as a result of compression fractures when osteoporosis weakens the spine’s bones. Over time, this may cause a progressive decrease in height, frequently several inches.
- Tenderness or Pain in the Bones
In regions of the body where the bones are weak, including the spine, hips, or wrists, bone tenderness or pain may be experienced, especially if the bone is prone to fracture.
- Stooped Posture (Kyphosis)
Osteoporosis patients may experience kyphosis, a hunched or stooped posture. The back is bent as a result of the vertebrae in the spine breaking.
- Having trouble moving or bending
People with osteoporosis may have decreased mobility and find it difficult to bend or move specific body parts painlessly due to degeneration of the bones and potential fractures.
- Weakness in Gripping Power
Fractures or pain in the hands and wrists can cause weakened grip strength, which makes it harder to grasp onto objects or carry out daily duties.
- A Higher Chance of Falls
Additionally, osteoporosis can lead to muscle weakness and balance problems, which can raise the risk of falling, particularly in older persons.
Risk factor:
Osteoporosis risk factors are conditions or actions that increase your likelihood of developing the illness. While you have no control over some risk factors, you can manage many of them with medical treatment and lifestyle modifications.
The following are the main osteoporosis risk factors:
- Age
Due to a natural decline in bone density with age, older persons are more at risk. As testosterone levels drop after menopause, this process quickens for both women and older men.
- Gender
Women are more likely than men to have osteoporosis. This is because menopausal hormone changes cause the bone density to rapidly decrease. Women are more prone to osteoporosis since their bones are often thinner and smaller.
- Family Background
Your risk is increased if you have a family history of osteoporosis or fractures. You might also be more at risk if your parents or grandparents had the illness or were prone to bone fractures.
- Lack of physical activity
Weaker bones might result from a sedentary lifestyle or from not doing weight-bearing activities like strength training, jogging, or walking. Frequent exercise maintains bone strength and promotes bone growth.
- Previous Fractures
An increased risk of future fractures is indicated by a history of previous bone fractures, particularly following a mild accident.
- Excessive Consumption of Alcohol
Excessive alcohol consumption may affect bone growth by interfering with the body’s calcium consumption. Additionally, it affects balance, raising the possibility of fractures and falls.
- Smoking
Smoking increases the risk of osteoporosis and fractures by interfering with bone production and lowering blood supply to bones.
- Some Medicines
When taken over extended periods, corticosteroids (like prednisone) and certain other medications, including anticonvulsants, chemotherapy treatments, and cancer therapies, can cause bone loss. Certain medicines can weaken bones over time and raise the risk of fractures.
- Medical Problems
Gastrointestinal disorders: Disorders such as inflammatory bowel disease (IBD) or celiac disease can cause nutritional malabsorption, which in turn can lead to osteoporosis.
Chronic renal illness can affect bone health by altering the balance of calcium and phosphorus.
Rheumatoid arthritis: Rheumatoid arthritis’s ongoing pain may speed up bone loss.
- Poor Nutrition and Eating Disorders
Low levels of calcium and vitamin D are among the nutritional deficiencies that can result from anorexia nervosa and bulimia, and both conditions raise the risk of osteoporosis.
Bone density loss can also be caused by low body weight and nutritional deficits linked to these conditions.
Diagnosis:
A physical examination, imaging testing, and medical history are frequently used to diagnose osteoporosis. A bone density test is the most popular way to identify osteoporosis.
Medical History
Your physician is going to ask about your family’s and your medical history, particularly concerning:
- Any indications of bone loss or past bone fractures.
- Fractures or osteoporosis in the family history.
- Diseases or medications that may have an effect on bone health (e.g., corticosteroid use, thyroid issues).
- Lifestyle choices (e.g., food, exercise, alcohol, and smoking).
Physical Examination
During a physical examination, your doctor will also check for kyphosis, a stooped posture that may indicate vertebral fractures and any signs of spinal anomalies.
Height measurement: A decrease in height as osteoporosis worsens could be a sign of spinal compression fractures.
Your doctor may evaluate your balance and muscle strength to determine your fall risk.
Bone Density Test (DXA or DEXA Scan)
The most popular and reliable test for identifying osteoporosis is Dual-Energy X-ray Absorptiometry (DEXA or DXA).
This test measures the concentration of a mineral, usually calcium, in a specific bone area, like the wrist, hip, or spine.
T-score: The findings are contrasted with the bone density of a healthy, normal adult. The T-score indicates how much your bone density varies from the average peak bone mass of a young, healthy person.
- Bone density is normal if the T-score is -1.0 or greater.
- T-score in the range of -1.0 to -2.5: Osteopenia (poor bone mass without osteoporosis yet).
- A T-score of -2.5 or less indicates osteoporosis.
X-rays
Although X-rays are not commonly used to check for osteoporosis, they might be recommended if you have a history of fractures or symptoms like back pain. Although an X-ray can reveal bone fractures or structural alterations caused by osteoporosis, it is not as sensitive as a bone density test for identifying the condition in its early stages.
Differential Diagnosis:
Reduced bone strength and density are the indications of osteoporosis, a disorder that raises the risk of fractures. When diagnosing osteoporosis, medical experts investigate several conditions that may resemble the disease or cause similar bone-related issues.
A differential diagnosis for osteoporosis is as follows:
- Osteomalacia: A condition in which the bones become weaker as a result of either a phosphate or vitamin D deficiency. This condition is caused by poor bone mineralization, as opposed to osteoporosis, which is a condition of loss of bone density.
- Bone Disease: Paget’s disease causes abnormal bone remodeling, which weakens bones and increases their risk of fracture or deformity. This is a more localized disorder that frequently causes pain and deformity in particular bones, such as the pelvis, spine, and skull. The two conditions can occasionally be confused with osteoporosis.
- Osteogenesis Imperfecta: A genetic ailment that causes fragile bones, this condition can be mistaken for osteoporosis when fractures happen, particularly in children or young people.
- Rheumatoid Arthritis: Rheumatoid arthritis causes chronic inflammation, which can cause bone loss and joint damage. However, unlike osteoporosis, this bone loss may not be common and is frequently the result of inflammation.
- Cushing’s Syndrome: Bone loss and fractures can result from excessive cortisol production, which can frequently come on by long-term corticosteroid use or anomalies in the adrenal glands. Cushing’s syndrome characteristics, such as weight gain and moon face, can help identify it from osteoporosis.
- Multiple myeloma: Osteolytic lesions that weaken bones can result from this plasma cell malignancy. Multiple myeloma patients may experience bone pain or fractures that were originally misdiagnosed as osteoporosis. Imaging tests and bone marrow biopsies may help in the diagnosis.
Osteoporosis Treatment:
By slowing down bone loss and encouraging bone production, osteoporosis treatment tries to improve bone strength, prevent fractures, and lessen pain. Usually, treatment combines a mix of medication, physical therapy, lifestyle modifications, and taking care of risk factors or underlying illnesses.
Lifestyle Modification
- Diet: Make sure you’re getting enough calcium and vitamin D, as these are essential for healthy bones.
- Calcium: Most individuals should consume 1,000 mg per day, whereas postmenopausal women and older adults should get 1,200 mg.
- Vitamin D: necessary for the taking in of calcium. 800–1,000 Mg per day is the ideal amount, however, higher dosages may be needed if there is a deficiency.
Medicines
There are numerous kinds of medications that can be used to treat osteoporosis:
- Bisphosphonates
The most often prescribed medications for osteoporosis are these. By stopping the breakdown of bones, they help in the prevention of fractures.
Zoledronic acid (Reclast), alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) are examples.
- Modulators of Selective Estrogen Receptors (SERMs)
Without some of the dangers associated with estrogen therapy, these medications simulate the effects of estrogen on bone. They lessen the resorption of bone.
Raloxifene (Evista) is one example.
Use: Usually given to postmenopausal women who are unable to tolerate alternative therapies.
- Menopausal hormone therapy (HRT) or hormone replacement therapy(MHT),
Estrogen, the female sex hormone, is essential for preserving bone tissue strength in women. Menopause raises the risk of osteoporosis and osteoporotic fractures and results in a significant decrease in estrogen levels.
Menopausal hormone therapy (HRT) for menopause has been linked to an increased risk of several illnesses, including breast cancer and venous thrombosis (blood clots in the veins), even though it increases estrogen levels and protects osteoporosis after menopause. On the other hand, Menopausal symptoms such as redness, sweats, and difficulty sleeping can be effectively treated with menopausal hormone treatment (HRT).
Although long-term use is no longer advised for managing osteoporosis, it is still regarded as a first-line treatment for women under 60 who are at risk for osteoporosis and a reduction in bone density.
- Analogs of Parathyroid Hormones
By simulating the effects of parathyroid hormone (PTH), these medications promote the growth of new bone.
Examples include Abaloparatide (Tymlos) and Teriparatide (Forteo).
For people with severe osteoporosis or those who are at high risk of fractures, this medication is usually prescribed.
It is important to remember that every medicine has the potential to have negative side effects. If your doctor prescribes medicine for osteoporosis, go about the advantages and disadvantages of the course of therapy.
Physical Therapy Treatment
Older adults are more likely to have osteoporosis, which frequently causes falls. People 65 and older frequently experience falls. A physical therapist can help you strengthen your balance if you are in danger of falling.
An essential part of managing osteoporosis is physical therapy. Improving strength and balance, lowering the risk of fractures, and maintaining or increasing mobility are the basic objectives of physical therapy for osteoporosis.
People with osteoporosis can live more active and independent lives while reducing their risk of fractures by using physical therapy, which combines focused exercises, posture correction, and fall prevention techniques.
Osteoporosis Physical Therapy Goals:
- Strengthening muscles to protect bones and reduce the risk of falls.
- Improving balance to avoid falls, which are a significant risk factor for osteoporosis patients’ fractures.
- Correcting one’s posture can help prevent compression fractures and preserve a healthy spinal alignment.
- Weight-bearing activities can increase bone density by promoting bone growth and preventing bone loss.
Exercises for Osteoporosis Video
Types of Exercises for Osteoporosis:
Weight-Bearing Activities
Exercises involving weight bearing apply pressure to the bones, which promotes bone growth. These workouts require you to stand and move against the force of gravity.
Example,
- Walking
- Hiking
- Climbing stairs
- Jogging (if tolerated; however, people with severe osteoporosis should be cautiously watched)
Resistance Exercise (Strength Exercise)
Strength training promotes bone health by increasing muscular mass. Strong muscles protect the bones by receiving some of the effects during exercise.
Example,
- Bodyweight workouts include wall push-ups, lunges, and squats
- Using resistance bands or free weights
- Weight-lifting devices
Resistance training can help stop more bone loss, particularly in the wrists, hips, and spine.
Exercises For Range of Motion and Flexibility
Maintaining or increasing flexibility is essential for preserving mobility and lowering joint and muscle stiffness. Stretching helps in this process. To prevent muscle imbalances that may result in falls, these exercises are important.
Example,
- Mild yoga or tai chi (with adjustments to prevent excessive spinal flexion)
- Hip flexor, calf, and hamstring stretches that are easier
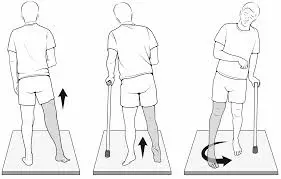
Exercises for Balance and Coordination
Physical therapy must focus on improving balance and coordination because osteoporosis raises the risk of falls. Balance-improving exercises help lower the chance of fall-related injuries.
Example,
- Standing on one leg
- Walking heel to toe, or walking in a straight line while touching the toe of the subsequent step
- Tai chi and other balance-focused exercises that promote slow motions
- Uses of stability balls or balancing boards
Balance and posture also benefit from exercises that strengthen the core, such as pelvic tilts or modified planks.
Posture Correction
Vertebral compression fractures caused by osteoporosis can result in kyphosis, a hunched or stooped posture.
Physical therapists can help patients strengthen the muscles that support the spine and improve posture by teaching them exercises and strategies.
Example,
- Postural exercises include chest openers, shoulder blade squeezes, and seated rows.
- Exercises for breathing: Diaphragmatic breathing to support a straight posture
- Exercises for spinal extension: To prevent spinal flexion, try gentle back stretches or targeted workouts like “back extension” movements.
Physical Therapy Precautions for Patients with Osteoporosis:
Avoid High-Risk Movements: People with osteoporosis should refrain from or alter certain workouts and movements, such as:
- Spinal flexion: Stay away of excessive forward bending as this might strain the vertebrae and cause fractures.
- Twisting motions: To prevent over stressing the spinal discs and joints, the spine should rotate as little as possible.
- High-impact exercises: Stay away of sprinting, jumping, and other activities that put your bones in fast contact.
Progress and Supervision: The physical therapist should be supervised to make sure that exercises are done correctly and safely. It is best to raise the intensity gradually so that the body can adjust without becoming hurt.
Surgical treatment
The main effects of osteoporosis are changes in bone density and structure, which make bones more susceptible to breaking. Although medication, lifestyle modifications, and preventative measures are the core of osteoporosis treatment, surgical treatments may be required in extreme cases when fractures or considerable deformities are present.
In patients with osteoporosis, fractures that do not heal properly, severe pain, or the need to stabilize broken bones are the most frequent causes of surgery. The primary surgical procedures for osteoporosis-related problems are listed below:
Vertebroplasty and Kyphoplasty
In patients with osteoporosis, vertebral compression fractures are frequently treated with minimally surgical procedures such as vertebroplasty and kyphoplasty. By stabilizing damaged vertebrae, these surgeries hope to lessen pain and stop more falls.
- Vertebroplasty: This treatment stabilizes the fractured vertebra by injecting a specific cement into it. Because of the cement’s rapid solidification, the bone is less likely to break down further.
- Kyphoplasty: This procedure compares to vertebroplasty, but before the cement is injected, a balloon is placed inside the vertebra to partially restore its lost height. More pain relief and better spinal alignment can be achieved with this operation than with vertebroplasty.
Indications: Generally speaking, these procedures are advised for people who have:
- Severe back pain due to vertebral fractures.
- Conservatively treated compression fractures that do not heal.
- A decrease in spine height or curvature, such as a “dowager’s hump.”
Spinal Fusion
In cases when vertebral fractures have resulted in severe spinal instability or considerable deformity, such as a misaligned spine or an extreme forward curvature of the spine, spinal fusion is a more invasive surgery.
Procedure: To support the spine, spinal fusion is attaching two or more vertebrae using bone grafts, rods, screws, or plates. By removing motion between the fused vertebrae, this procedure helps lessen the pain that comes with bone fractures.
Signs: There may be a need for spinal fusion when:
- A severe misalignment or deformity of the spine is present.
- Bracing and physical therapy are examples of non-surgical treatments that have not been successful in reducing pain.
- When the vertebrae are unstable, the spinal cord or nerves could be further damaged or compressed.
Prevention of Osteoporosis:
Maintaining a healthy lifestyle and habits that support strong bones throughout your life is essential to preventing osteoporosis. Even though osteoporosis may not be completely preventable, There are several things you can do to reduce your risk and maintain the health of your bones, especially if you have a certain gene or a family history of the condition.
Get Enough Calcium
Calcium is necessary for healthy bones. It helps in maintaining and increasing bone mass.
Calcium-rich foods include:
- Dairy goods (cheese, yogurt, and milk).
- Leafy greens, such as bok choy, broccoli, and kale.
- Foods that have been fortified (certain plant-based cereals, juices, and milk).
- Salmon and sardine fish.
- Consult your physician about calcium supplements if you struggle to obtain enough of it from your diet.
Weightlifting Exercises
One of the most important things you can do to avoid osteoporosis is to exercise. It improves balance and lowers the chance of falls by strengthening bones and muscles.
Exercises with weights include:
- Jogging, hiking, or walking.
- Aerobic or dancing.
- Resistance training or lifting weights.
- Sports that require physical activity, like tennis.
Refrain from smoking
Smoking weakens bones and decreases blood supply to them, increasing the likelihood that they will break. To reduce your chances of osteoporosis and improve your general bone health, think about giving up smoking.
Keep Your Weight in Control
Osteoporosis risk can be increased by being underweight or overweight. Bone health is supported by a healthy weight.
Your bones might not have enough bulk to remain strong if you are underweight. Being overweight can place additional strain on your bones, especially your hips and spine.
Observe and treat the underlying conditions.
Bone health can be affected by certain medical diseases, such as diabetes or rheumatoid arthritis. Follow your doctor’s treatment plan to manage any underlying conditions you may have.
Preventing Falls
For those with weak bones, preventing falls is essential to preventing fractures.
To lower the risk of falls;
- Engage in exercises like yoga or tai chi to improve your balance and coordination.
- To make your house safer, remove dangerous surfaces like loose carpets and make sure there is enough lighting.
- In bathrooms, place non-slip mats and, if necessary, grab bars.
When should I visit my physician?
You should make plans to see your doctor if you think you may have osteoporosis. Your best chance of avoiding broken bones as you age is to treat osteoporosis early. A family history of osteoporosis is possible. If a close relative has the illness, let your doctor know. If you have ever experienced a bone break or fracture as a result of a small injury, you should also disclose this information to them.
Summary:
When bone mass and mineral density decrease, or when the composition and strength of bone change, osteoporosis develops. The risk of fractures (broken bones) may rise as a result of this reduction in bone strength.
Your bones become weaker and thinner than they should be due to osteoporosis. Because it increases your risk of suffering a bone fracture, it may be harmful. Since you usually don’t have any symptoms and might not even be aware that you have osteoporosis until you break a bone, it’s known as a “silent” illness.
Osteoporosis management includes a long-term strategy to care in addition to medication, physical therapy, and lifestyle modifications. To guarantee ideal bone health, this entails routine examinations, bone density tests, and support from medical professionals.
FAQ:
What is osteoporosis?
Osteoporosis is a bone disease that weakens and cracks the bones, making fractures more likely. Even while this disorder may not cause any symptoms, it can lead to fractures, especially in the spine, hips, and wrists.
What is the cause of osteoporosis?
As people age, their bone density naturally declines.
Hormonal alterations caused by reduced estrogen levels, especially in postmenopausal women
Absence of vitamin D or calcium.
A life that is sedentary.
Genetics and family history.
Smoking or drinking too much alcohol.
Certain medications including corticosteroids.
For whom is osteoporosis a risk factor?
Postmenopausal women.
People over fifty, those with a family history of osteoporosis, and those with low body weight.
Individuals who are dehydrated, particularly those who don’t get enough calcium or vitamin D.
Heavy drinkers or smokers.
Individuals with specific medical disorders or those using steroids or other long-term medication.
How can osteoporosis be prevented?
Receiving enough calcium and vitamin D from food or supplements.
Strength training, jogging, and walking are weight-bearing activities that help build stronger bones.
Avoiding heavy drinking and smoking.
Keeping a healthy weight and eating a well-rounded diet.
Those at risk should have regular bone density tests.
How does one diagnose osteoporosis?
DEXA (Dual-Energy X-ray Absorptiometry), a bone density test, is commonly used to diagnose osteoporosis. By measuring bone mineral density, this test may help identify individuals who are at risk for fractures or who have osteoporosis.
Which symptoms of osteoporosis are present?
The reason osteoporosis is frequently referred to as the “silent disease” is that many patients do not show any symptoms until they have a bone fracture. However, typical symptoms include of:
Back pain that could be brought on by a vertebral fracture or collapse
A slow decline in height
A stooped-over position (kyphosis)
Which foods are beneficial to bone health?
Bone health depends on foods high in calcium and vitamin D, such as:
Dairy goods (yogurt, cheese, and milk)
Leafy greens, such as kale and spinach
Fish (sardines, salmon)
Plant-based milk and cereals are examples of fortified foods.
Seeds and nuts (chia seeds, almonds)
Men can develop osteoporosis?
Yes, osteoporosis can affect males as well as women, however, it is more common in women. Although male osteoporosis affects roughly one in four men over 50, it is frequently underdiagnosed.
Which kinds of physical activity are advised for people with osteoporosis?
Exercises involving weight bearing, such as dancing, hiking, and walking
Resistance training (using resistance bands or mild weightlifting)
Balance improving exercises like yoga and tai chi
Exercises for flexibility can help you keep proper posture and lower your chance of falling.
What are osteoporosis complications?
Especially in the wrists, hips, and spine, bone fractures are the most frequent side effect of osteoporosis. These fractures, especially in elderly persons, can cause pain, loss of independence, and damage.
How can osteoporosis affect a person?
Osteoporosis causes weak, broken bones that are easily fractured by small stresses like bending over. Osteoporosis is most frequently associated with fractures of the hip, wrist, or spine. There is a constant breakdown and replacement of bone and other living tissue.
Is it possible to cure osteoporosis?
Although there is no cure for osteoporosis, its symptoms can be managed with medicine and changes in lifestyle. Based on your age, sex, and medical history, your doctor will recommend several treatments to help you. The goal of treatment is to strengthen your bones so that they are less likely to break.
Which organ suffers from osteoporosis the most?
As a result of osteoporosis, bones get weaker. This makes it more likely that the bones may break. The most commonly affected bones are the wrists, hips, and spine. Because of a decrease in estrogen after menopause, males are four times less likely than women to develop osteoporosis.
Does walking help people with osteoporosis?
Examples include walking, dancing, gardening, elliptical training, low-impact aerobics, and climbing stairs. These workouts directly target the legs, hips, and lower spine to reduce bone loss.
What are the osteoporosis risk factors?
Age: The danger is higher for those over 50.
Gender: Osteoporosis is more common in women, particularly after menopause.
Family history: The risk may be elevated if one parent has osteoporosis.
Diet: Insufficient consumption of calcium and vitamin D raises the risk of bone loss.
Alcohol and smoking: Both excessive alcohol consumption and smoking can damage bones.
Physical inactivity: Not exercising may speed up the loss of bone.
Medical conditions: Some illnesses can raise the risk, such as thyroid issues and rheumatoid arthritis.
Which lifestyle modifications are beneficial for osteoporosis?
Exercise more: Resistance training and weightlifting can help preserve bone density.
Increase your nutrition: Consume foods high in vitamin D (from fortified foods to sunlight) and calcium (from dairy products to leafy greens).
Give up smoking and cut back on drinking.
Make sure your house is fall-proof. To prevent accidents, remove any potential risks that could cause falling and use support devices or supports as needed.
References:
- N. S. C. a. O. Branch (2025, January 8). osteoporosis. The National Institute of Musculoskeletal and Skin Disorders and Arthritis. The following URL: https://www.niams.nih.gov/health-topics/osteoporosis#:~:text=Osteoporosis in Men-, Osteoporosis is a bone disease that occurs when bone mineral, pregnancy, breastfeeding, and bone health
- OrthoInfo, AAOS, Osteoporosis (n.d.). Osteoporosis: https://orthoinfo.aaos.org/en/diseases–conditions/
- N. P.-. Physiotherapist (2024, January 22). The causes, symptoms, diagnosis, and treatment of osteoporosis. Mobile Clinic for Physiotherapy. Osteoporosis: https://mobilephysiotherapyclinic.in/
- Osteoporosis. February 7, 2025. Cleveland Medical Center. Osteoporosis https://my.clevelandclinic.org/health/diseases/4443
- Website, N. April 17, 2024. NHS.uk: Osteoporosis. Osteoporosis: https://www.nhs.uk/conditions/
- Health and Human Services Department, n.d. osteoporosis. The Better Health Channel. Osteoporosis: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments
- MacGill, M. November 14, 2023. Information on osteoporosis. Medical News Today: https://www.medicalnewstoday.com/articles/155646
- Image 1, There are six ways to prevent osteoporosis, according to The Orthopedic Institute of New Jersey (n.d.). This article discusses ways to prevent osteoporosis.





6 Comments