Nebulizer
A Nebulizer: What Is It?
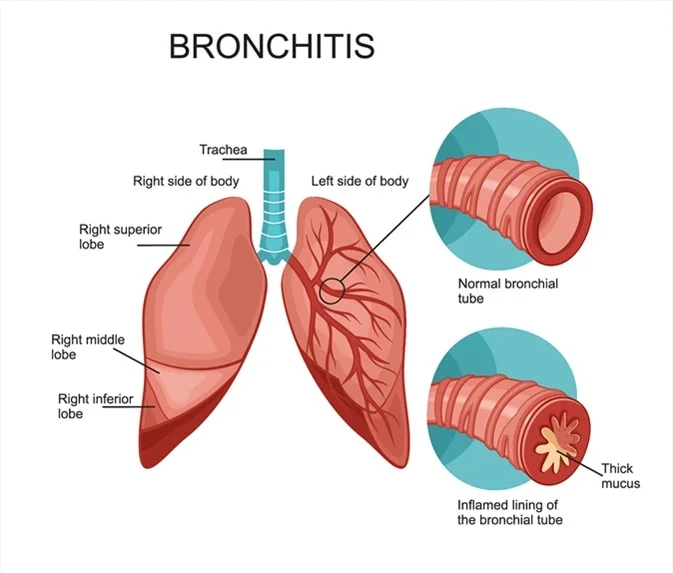
A nebulizer is a medical equipment used to administer medication in the form of a mist inhaled into the lungs. It is commonly used for patients with respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis, and other respiratory diseases.
Nebulizers are available in portable and home (tabletop) varieties. Larger nebulizers meant for use at home require an electrical outlet to be plugged in. Nebulizers that are portable can be powered by batteries or by plugging them into a car socket. You can fit them in a briefcase or purse because some of them are not much larger than a deck of cards
Nebulizers can be obtained through a prescription from a physician or from your pediatrician’s office. In addition, many people receive breathing treatments at their physician’s office.
Nebulizers for use at home can cost up to $50, not including accessories. Nebulizers that are portable typically cost a little more.
Nebulizers are typically covered by health insurance plans under the durable medical equipment section. However, the majority of insurance providers require you to use a specific vendor. Make careful to inquire with your insurance provider before buying or renting a nebulizer. You should be able to get assistance from your medical staff.
How are nebulizers operated?
Pressurized air is used by a nebulizer to deliver liquid medication. Even while most asthmatics use both nebulizers and inhalers, there are times when using a nebulizer might be simpler for small children who might not know how to use an inhaler correctly.
Nebulizers may take a while to work, therefore in cases where airways narrow—like during an asthma attack—an inhaler is typically a preferable choice.
The following substances are frequently used in nebulizers:
- Drugs called bronchodilators aid in clearing the airway.
- Medical-grade saline, or saltwater, solutions aid in the breakdown of lung mucus.
- Antibiotics aid in the prevention or treatment of infections.
The medications you need to take via nebulizer will be determined by your doctor depending on your specific requirements. It’s possible that you’ll receive liquid in pre-made containers that you can just open and use in the machine, or you might need to mix the solution each time it’s used.
Nebulizers are not suitable for delivering all medications. Some drugs, such as steroids, must be inhaled.
Nebulizer types include:
Nebulizers come in three primary varieties:
Jet nebulizers are devices that create an aerosol of medicines by compressing gas, such as air.
Vibrations at high frequencies are used by ultrasonic nebulizers to create aerosol. These are usually not for personal use and are used more frequently in hospitals.
Mesh nebulizers work with a mesh cap that has microscopic pores in it to help deliver medication very effectively. Generally speaking, these are more efficient than jet nebulizers and have been around longer.
Consult your physician to determine if a mask or a mouthpiece is best for you or your kid. Children under five tend to breathe more via their noses than older children and adults do, therefore face masks that cover the mouth and nose are usually preferable for them.
What tools are required to operate the nebulizer?
The following supplies are required:
- portable nebulizer.
- Air compressor.
- mouthpiece or face covering.
Why Would You Apply a Nebulizer?
Nebulizers are particularly useful for administering asthma medicine to newborns or young children. They might be useful as well if you have problems using an inhaler for asthma or require a high dose of an inhaled drug.
One common term for nebulized therapy is breathing treatment. Nebulizers can be used in conjunction with a range of drugs to manage asthma symptoms and provide immediate relief. Among them are:
Corticosteroids (e.g., budesonide, flunisolide, fluticasone, and triamcinolone) for the treatment of inflammation
bronchodilators (such as salmeterol, albuterol, formoterol, and levalbuterol) to widen your airways
How should I apply it?
Your physician will prescribe how frequently you use your nebulizer. They will assist you with any particular instructions related to your treatment as well.
As directed, take your medication at all times. It’s critical that you keep to your doctor’s instructions regarding the best times and methods for using your nebulizer.
Nebulizer use can take ten to fifteen minutes. All that’s required is regular breathing.
The following are basic guidelines for using a nebulizer:
Do a hand wash. Always wash your hands before handling the medication and nebulizer to prevent bacteria from entering your lungs and entering the machine.
Examine the drugs. you are taking. Examine your medication carefully before starting:
Is it past its expiration date?
Is there damage or crushing on the vial?
Is there discoloration on the medication?
Has it ever been in exceptionally high or low temperatures?
Replace the medication if any of these apply to you.
Assemble the tools you need. Most versions consist of a tongue piece, tubing, an air compressor (the basic nebulizer machine), a cup (the nebulizer) with the medicinal product inside, and tubing. Perhaps you’re wearing a mask. The compressor creates an aerosol by pumping air into the medication in the cup. How well the mechanism creates droplets the proper size to enter deep into the airways is determined by the cup design. Medication that is breath-actuated or breath-enhanced is less likely to leak into the atmosphere. Patients who are too old or disabled to utilize a mouthpiece well, as well as very small children, should always wear masks.
Add medication to the cup of the nebulizer. Using unit-dose vials is as simple as twisting off the lid and pouring. Select a nebulizer cup that can be easily poured by sitting flat. Smell the medication as you pour it out; discard any that smell bad, rotten, or like they might contain rubbing alcohol. Avoid overfilling the cup as this could prevent the drug from being aerosolized at the proper particle size.
Sit back and try to keep your cool. Once you have put on the mask or covered your tongue with the mouthpiece, bite your lip firmly and close it, then switch on the nebulizer machine.
Breathe in a regular manner. If you begin to cough, turn off the machine until you are able to breathe normally once again. Once the cup is empty, keep doing the breathing exercise. If the medication foams or bubbles, stop the therapy because there’s a chance the substance or equipment is contaminated. Avoid “blow-bying” or misting the drug in front of the child’s face as this will disperse it into the atmosphere rather than into their lungs. Put on a mask.
Clean up. By following the manufacturer’s directions, you can keep the mouthpiece, cup, and tubing of your nebulizer clean. Anything that gets into your cup, such as dust from the house, medication, or your hands, will enter your lungs. After everything is dry and clean, store the system in a place where dust won’t collect.
Maintenance of nebulizers:
It’s easy to clean and disinfect your equipment, but it’s crucial. After every treatment, the nebulizer cup needs to be cleaned with warm water.
Rinse the mouthpiece, mask, and nebulizer cup in warm, soapy water with a tiny bit of detergent after each use. Give it a thorough rinse, then allow it to air dry. Remark: There is no need to clean the tube that connects the air compressor and nebulizer.
Once a week is plenty to clean your nebulizer; more often if directed. Use one of the following techniques to disinfect the nebulizer after cleaning your equipment.
Use one of the following cold disinfection techniques on disposable nebulizers:
- Soaking for 5 minutes – isopropyl alcohol.
- Spend 30 minutes soaking in 3% hydrogen peroxide.
Soak for thirty minutes in a mix of one part white vinegar to three parts water.
Follow any of these cold disinfection methods with a thorough rinse and let air dry.
Nebulizers that are not disposable can be cleaned as previously mentioned. Any of the following thermal disinfection techniques may also be used to clean them:
Soak for five minutes.
Place in a bowl of water and microwave for 5 minutes.
In the dishwasher, manage at 158 degrees Fahrenheit for 30 minutes.
Use a baby bottle sterilizer.
Storage of medications
Make sure to follow the manufacturer’s instructions and store all of your medications in a cold, dry location.
Examine your medications frequently. Verify that they haven’t developed crystals or changed colour. Discard your medications if you observe any changes in their appearance.
Maintenance on compressors
Make certain that your gadget has been unplugged before disinfecting it. Wipe your air compressor down with a fresh, wet cloth as needed to keep it looking clean.
The compressor that pumps air should not be left on the ground while being treated or stored.
As instructed, check the filter on the air compressor. As instructed by the manufacturer of your device, change or clean the filter.
A backup tongue, mask, and nebulizer cup should always be kept on hand.
You can purchase all the consumables required for your nebulizer therapy from your equipment provider.
Inhaler vs. Nebulizer
Both nebulizers and inhalers have benefits and drawbacks when it comes to administering medication to the lungs. Giving medication takes longer—at least five to ten minutes. Moreover, even lightweight nebulizers may be bulky and challenging to move. However, some patients prefer nebulizers because they can see and feel the drug mist.
Compared to nebulizers, inhalers are frequently less expensive and have fewer side effects. One can fit in your purse or pocketbook. Although using an inhaler can be challenging at first, most people pick it up very quickly. The dosage of the drug is accurate.
How should I use a nebulizer to treat my asthma correctly?
To operate a nebulizer, listen to the following instructions:
- To avoid contamination, start by cleaning your hands.
- Fill the nebulizer cup with the appropriate asthma medication.
- Fasten the mouthpiece or mask and the cup to the compressor.
- To allow for optimal lung capacity, sit up straight. Turn on the compressor after placing the mouthpiece in your mouth or your mask over your face.
- Take deep, focused breaths through your mouth for five to fifteen minutes, or until the drug wears off, without holding your breath.
- To ensure that the nebulizer functions correctly the next time, clean it after use in accordance with the manufacturer’s recommendations.
Speak with your physician, respiratory therapist, or asthma educator for more specific instructions.
Conclusion
With the use of nebulizers, liquid drugs can be easily taken into the lungs in the form of a fine mist. They are sometimes used in conjunction with inhalers and are utilized for a number of medical disorders, such as cystic fibrosis, asthma, and COPD.
Nebulizers come in a few different varieties. Your doctor will let you know which kind works best for you. They will also go through how to utilize and maintain it.
FAQs
What is the purpose of a nebulizer?
A nebulizer is a machine that creates a spray of air from liquid medication, which is subsequently inhaled through a mask or mouthpiece.
Does nebulization help with coughing?
Nebulizers can indeed aid with a cough, although this will depend on the patient’s health and medicine.
What does nebulization therapy aim to achieve?
One common term for nebulized therapy is breathing treatment. Nebulizers can be used in conjunction with a range of drugs to manage asthma symptoms and provide immediate relief. Among them are: Corticosteroids (e.g., budesonide, flunisolide, fluticasone, and triamcinolone) for the treatment of inflammation
Is nebulizing beneficial to the lungs?
Nebulizer treatments can be beneficial in reducing airway or lung inflammation, particularly when respiratory conditions like asthma are present.
Does the nebulizer have any adverse effects?
The following side effects should be reported as soon as possible to your care team: Skin rash, itching, hives, and swelling of the lips, tongue, or throat are examples of allergic reactions.
Can we use water in a nebulizer?
Only water can be used with the nebulizer. Verify that the water is boiled and cooled.
Is using a nebulizer every day okay?
Nebulizers are not recommended for long-term COPD or asthma treatment, according to some doctors. On the other hand, others claim that nebulizers with long-acting medication can be utilized as a daily treatment for certain COPD patients.
Which is preferable, an inhaler or nebulizer?
A nebulizer distributes a thin mist of medication through a mask worn over the mouth and nose, whereas an inhaler uses pressure to deliver medication through a mouthpiece. Inhalers may be more difficult to use than nebulizers, particularly for younger users.
Who requires a nebulizer?
Many sufferers of long-term lung conditions like COPD or asthma
References
- Professional, C. C. M. (n.d.). Home Nebulizer. Cleveland Clinic. https://my.clevelandclinic.org/health/drugs/4254-home-nebulizerCopy
- Nebulizer. (2024, March 15). WebMD. https://www.webmd.com/asthma/home-nebulizer-therapy
- Kerr, M. (2024, May 13). Is There a Relationship Between GERD and Asthma? Healthline. https://www.healthline.com/health/gerd/asthma#treatment
- How to Use a Nebulizer Machine. (2020, April 28). Allergy & Asthma Network. https://allergyasthmanetwork.org/what-is-asthma/how-is-asthma-treated/how-to-use-a-nebulizer/





One Comment