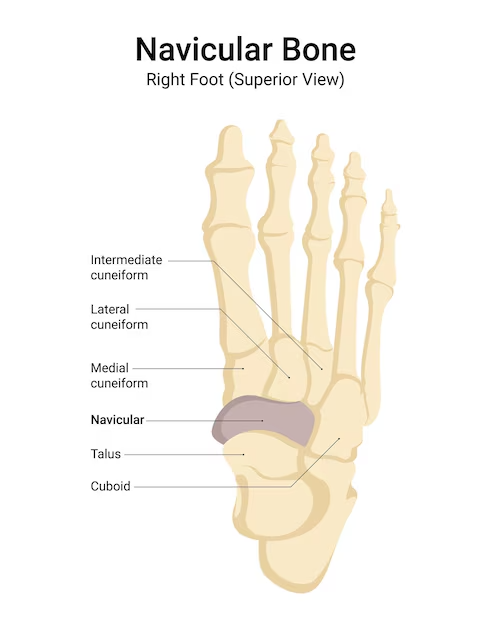
Navicular Bone
The navicular Bone, also called the nevicular bone, is a tiny, boat-shaped bone found in the foot. Human feet are constructed of 26 bones and 33 distinct joints. Seven tarsal bones, including this form the ankle and foot. The navicular bone is a wedge-shaped structure. It is seen within the central area of the upper inner side of the foot.
Anatomy
The ankle and foot’s tarsal region is composed of seven bones, including the navicular bone. The navicular bone stands next to the cuboid bone on the medial edge of the foot, underneath the cuneiform bones, and in front of the talus head. It is one of the midfoot’s five bones. This is the only remaining bone in the foot that can calcify completely.
The structure
- The navicular bone is pyriform in form, small in size, and irregular. Two weak depressions on the front side and a concave back aspect match the articulating surface of each of the cuneiform bones.
- The location directly anteroinferior to the medial malleolus is sometimes the simplest place to palpate the navicular tuberosity, a visible protuberance on the anteromedial face of the navicular bone.
Articulation
- In the posterior talocalcaneal joint, the talocalcaneonavicular joint and the subtalar articular complex in nature which is additionally known as the acetabulum pedis, merge.
- Its name comes from the fact that it resembles a ball and socket joint in certain morphological ways.
- The calcaneus’s anterior and middle joint surfaces, the navicular bone’s posterior joint surface, and the talus’ anteromedial surface create ties with the head.
- The medial aspect’s plantar calcaneonavicular ligament, also known as the spring ligament, and the lateral aspect’s lateral calcaneonavicular ligament, which is a part of the bifurcate ligament, stabilize these bones.
Ligamentous and Muscular Attachments
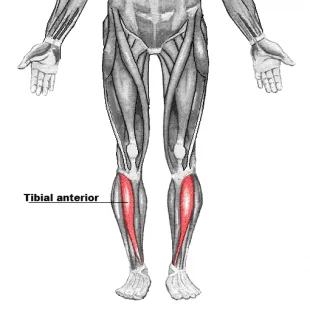
- The navicular bone has only one muscle attachment. The main muscle that ties is referred to as the tibialis posterior tendon. The muscle is located within the deep compartment of the posterior aspect of the tibia, and this tendon extends inferiorly across the medial malleolus to insert on the navicular tuberosity.
- Two ligaments, the dorsal ligaments, and plantar cuneonavicular ligaments, wrap with each cuneiform bone to the navicular. The medial cuneonavicular ligament has supplementary connections connecting it to the navicular bone, first, and medial cuneiform bones.
The Arterial Supply
- The dorsal pedis artery becomes split, producing approximately three to five supplementary minor branches that supply the navicular’s medial side. The posterior tibial artery comprises smaller branching on the bone’s side. The plantar surface of the bone receives additional blood supply via the medial plantar artery’s numerous divisions.
- Bone stress fractures are exacerbated by the blood supply part of the central navicular watershed.
Function
- The navicular has been frequently identified as the keystone of the foot’s medial longitudinal arch considering its position at the top of the arch and its function in sustaining the arch.
What is Accessory Navicular Bone?
- A big accessory ossicle that is visible next to the navicular bone’s medial side is called an accessory navicular.
- A different approach could speculate about the auxiliary navicular bone as a sesamoid in the rear tibial tendon, an extended version of the navicular, or in alignment with the navicular.
- Asian civilizations may have a much greater frequency of an accessory navicular bone (~45%), compared to a range of 4–21%.
- First manifests during adolescence.
- Frequently occurs in female patients.
- Both groups (both male and female) instances assemble up about 70% of cases (range: 50% to 90%).
Associated Conditions
The following conditions can affect the navicular bone:
- Fractures
- Kohler Disease
- Mueller-Weiss Syndrome
- Accessory Navicular Syndrome
Fractures
- Injuries can cause acute fractures of the navicular bone. Tension fractures can result from repeated tension.
- The navicular bone is typically cracked by competitive athletes as they kick, twist, or run. Pain and changes in walking style commonly accompany fractures. One of the most prevalent kinds of stress fractures involving racetrack athletes is navigational stress fractures.
- Treatment options include conservative or surgical procedures depending on the degree of the fracture. Casting is a conservative therapeutic option that allows the bone to recover.
- In addition to a cast to promote healing, surgery might be necessary to install screws to secure the bone.
Kohler Disease
- Kohler disease is classified as avascular necrosis or osteonecrosis, which indicates that bone tissue dies due to a lack of blood supply, which is required to maintain bones healthy. Kohler’s illness is most typically observed in young children aged 4 to 7. It is more prevalent in boys.
- Children’s navicular bones calcify around the age of three. As youngsters gain weight, the navicular bone becomes more susceptible to compression by other bones in the foot. This compression, combined with a lack of blood supply to the navicular bone, raises the risk of Kohler disease.
- Sensitivity and soreness in the central region of the foot are typical symptoms. Swelling could also be observed.
- This sickness is self-limiting and normally resolves itself as children mature. Anti-inflammatory drugs and immobilization with a brief walking cast are the recommended treatments for pain relief.
Muller-Weiss syndrome
- Muller-Weiss syndrome (MWS), often called Brailsford disease, is a bone degeneration illness that may influence adults in their middle decades. The prevalence of Muller-Weiss syndrome (MWS) is higher in women than in men.
- Although MWS can happen on its own, some people believe that trauma, bone migration, or congenital factors are responsible for the condition.
- Anti-inflammatories and immobilization are often effective treatments for pain. If necessary, surgical procedures might be used to relieve pain and restore the arch.
Accessory Navicular Syndrome
- Accessory navicular syndrome refers to the presence of an additional bone or cartilage fragment next to the navicular bone. Even so, it is congenital, meaning it exists from birth. It affects 4–14% of the population.
- Until the additional bone becomes an issue, the majority of people with accessory navicular syndrome do not even realize that they have it.
- Pain can be caused by trauma, sprains of the foot or ankle, and long-term irritation from shoes rubbing against these additional bones.
- Flat feet or falling arches can also put tension on the tendon that links to the bone, exacerbating accessory navicular syndrome and causing additional inflammation and pain.
The indications of accessory navicular syndrome are listed below:
- Midfoot and arch pain or throbbing, usually during or after exercise, noticeable protuberance or lump on the inside of the foot, above the arch
- Bony prominence edema and redness
Bone is formed throughout adolescence when cartilage calcifies. Symptoms of accessory navicular syndrome frequently manifest at this phase. Some people wait until later in life to start showing symptoms.
The diagnosis of accessory navicular syndrome can be verified by X-rays, examination, and pain history.
Treatment options include immobilization in a cast, physical therapy to strengthen muscles and reduce inflammation, anti-inflammatory drugs, and ice to minimize swelling. A customized orthotic device, which is placed within the shoe to support the arch, is an additional therapeutic alternative. Surgery to remove the additional navicular bone may be required if symptoms return following conservative treatment.
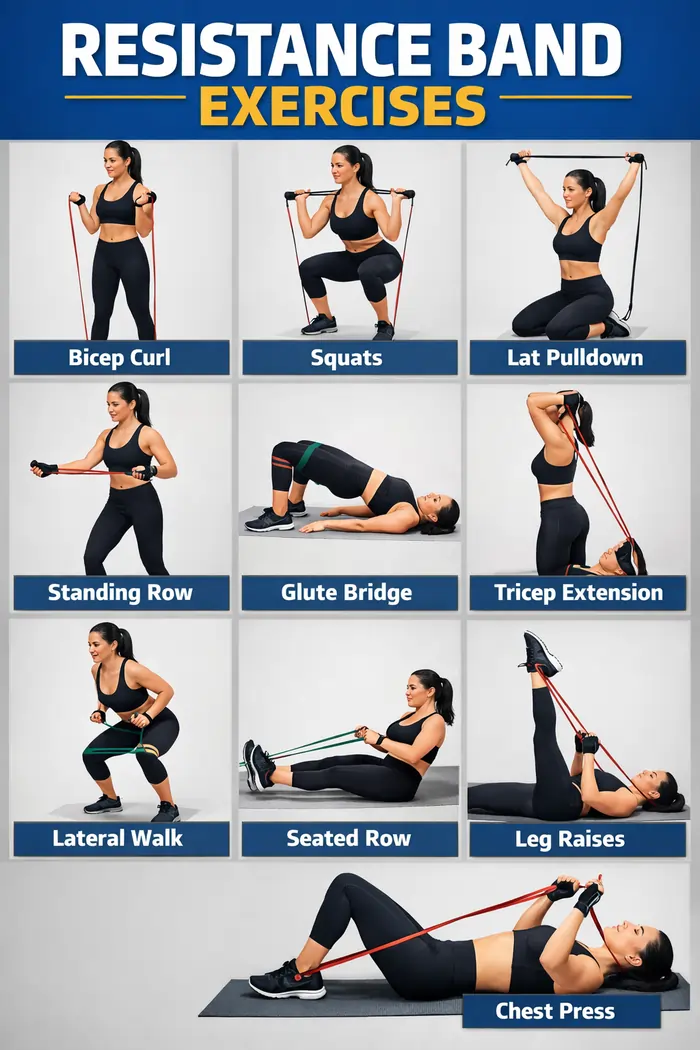
Treatment
- Both immobilization and anti-inflammatory medications are commonly used in the treatment of navicular bone-associated disorders.
- Specialized shoe inserts and physical treatment are frequently used to help prevent re-injury.
FAQs
What causes pain in the navicular bone?
The vast majority of auxiliary navicular sufferers are asymptomatic. This additional bone, however, may cause pain and swelling by irritating the posterior tibial tendon. Individuals who do have accessory navicular syndrome may have pain as a result of prolonged shoe irritation, direct trauma, or overuse.
With a navicular fracture, can I walk?
You will benefit from elevating your ankle because the edema normally grows worse at the end of the day. It will be simpler to walk with crutches in the beginning, but you can walk on your feet as long as it feels comfortable.
Why does the navicular bone stick out?
Sports overuse, flat feet, foot/ankle sprains, and poorly fitting shoes can all contribute to accessory navicular syndrome. The auxiliary navicular calcifies and hardens as children get older. The skin between the shoe and the auxiliary navicular may be directly compressed as a result.
Who treats the navicular bone?
By performing a physical examination, a foot and ankle surgeon can identify accessory navicular syndrome. To assess the condition and validate the accessory navicular diagnosis, MRIs and X-rays may be performed.
Is navicular bone healing possible?
If a navicular stress fracture is treated appropriately, it normally heals, but if left untreated, it can cause persistent foot pain.
Is navicular bone growing?
The auxiliary navicular bone develops and hardens during adolescence, just as other bones. The pressure of shoes or recurrent sprains where the extra piece of bone attaches can cause pain and swelling in those with auxiliary naviculars.
References:
- Ortho-pinion – What Is an Accessory Navicular – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/ortho-pinion-accessory-navicular/
- Rackley, D. (2023, August 16). Anatomy of the Navicular Bone. Verywell Health. https://www.verywellhealth.com/navicular-bone-anatomy-5088389
- Navicular bone. (2022, July 7). Kenhub. https://www.kenhub.com/en/library/anatomy/navicular-bone
- Patel, D. (2023a, July 9). Navicular Bone – Anatomy, Function, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/navicular-bone/


One Comment