Knee Joint
Introduction
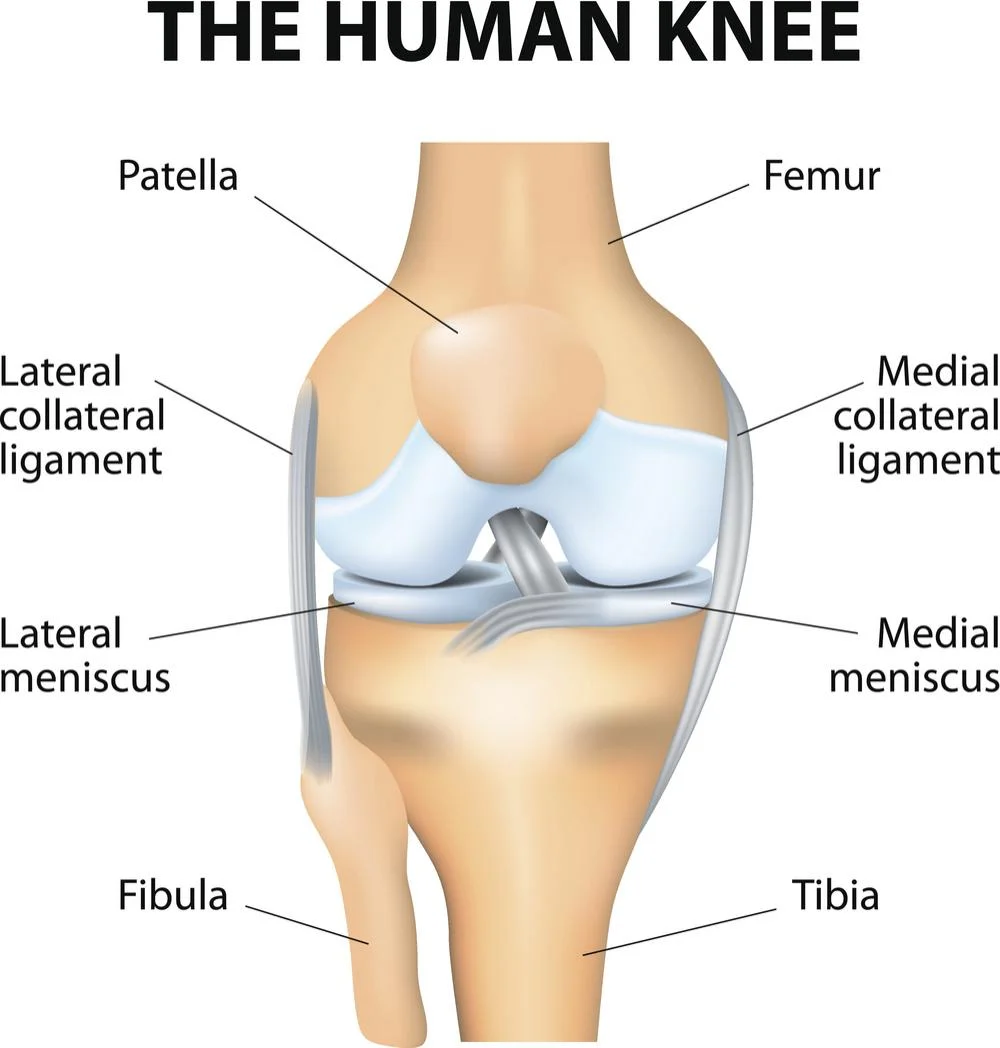
The knee joint is one of the largest and most complex joints in the human body, playing a crucial role in our ability to move and bear weight. It connects the thigh bone (femur) to the shin bone (tibia) and includes other structures like the kneecap (patella) and cartilage, which help in smooth movement. The knee joint is vital for activities such as walking, running, and jumping, making it susceptible to injuries and degenerative conditions.
The knee is an improved hinge joint, a type of synovial joint, made up of three functional compartments: the medial and lateral tibiofemoral articulations attach the tibia, the main bone of the lower leg, to the femur, the thigh bone, and the patellofemoral articulation, which involves the patella, or “kneecap,” and the patellar groove on the front of the femur through which it slides.
Synovial fluid, which resides inside a synovial membrane known as a joint capsule, around a joint. Recently, there has been a renewed focus on and research on the posterolateral corner of the knee.
The largest and most important joint in the body is the knee. This has an important influence on motion involving moving the body in both vertical (jumping) and horizontal (running and walking) directions.
The kneecap’s initial structure is cartilage, which will ossify (turn into bone) between the ages of three and five. Its ossification process takes somewhat longer because it’s the largest sesamoid bone in the human body.
Anatomy of Knee joint
The knee is known as the joint in the middle of your leg. It is the femur’s (thigh bone) and tibia’s (shin bone) connective tissue.
The joint of the knee is synovial. They are formed up of one bone with an oral cavity in it that another bone can go into. The ends of the bones that make up a synovial joint are covered in slick hyaline cartilage. The synovial membrane, a fluid-filled sac that protects and covers the joint, is what is found in between the bones. Synovial joints can move with the least friction possible because of this additional cushioning.
The knee is a hinge joint for function. Imagine the hinges that provide support for a door. A few sections are stationary, while the rest move to open and close by traveling a predetermined distance. Similar to your knee, hinge joints only open and close in a single direction.
Articulating Surfaces of the knee joint
The tibiofemoral and patellofemoral joints enable the thigh bone (femur), the shin bone (tibia), and the kneecap (patella) to articulate.
Articular cartilage, a very smooth and strong material intended to lessen friction forces, covers these three bones. The patella is situated in the intercondylar groove, which is a common femur indentation.
The superior tibiofibular joint, which attaches the smaller fibula to the tibia, is not involved in the knee joint, but it does provide a surface on which vital muscles and ligaments can attach.
The proximal articulating surface of the knee, which is made up of two massive condyles, is formed by the distal portion of the femur. A medial as well as lateral. Even though the short shallow groove between these two condyles anteriorly—which is known for having either a patella groove or patella surface, or even a femoral sulcus—connects them inferiorly by an intercondylar notch. The patella develops an early flexion.
Two asymmetrical, relatively flat condyles on a tibia are termed the tibial plateau. These are seen on both the medial and lateral surfaces. The diameter of the proximal tibia is significantly greater than the posterior shaft, which is sloped at a 7 to 10-degree angle to allow the flexion of the femoral condyles on the tibia. The medial tibial plateau is longer than the lateral anteroposteriorly.
Intercondylar tubercles—two roughened bony spines—separate the two tibial condyles, and they play an aspect in knee extension. The stability of the knee joint is increased when they are caught in the femur’s intercondylar notch. Given the plateaus’ minor anterior and posterior convexity, the tibiofemoral joint is often considered to be an unstable joint. This indicates the import of the menisci, one of the other knee structures.
Menisci
The region between the tibial and femoral condyles is mostly the location of two menisci. Their cross-section is triangular, and they have crescent-shaped lamellae with anterior and posterior points on each. Each meniscus’s surface is flat inferiorly according to the tibial plateau’s relative flatness and concave superiorly to give a congruous surface with the femoral condyles.
Although relative to a lateral meniscus, which has a more “O” shaped meniscus, the horns of a medial meniscus are farther apart and have a “C” shape. The larger medial meniscus, which consequently leaves a wide exposed portion that may be vulnerable to damage, is the reason for this.
Menisci increase the surface of contact, weight distribution, and stress absorption by correcting alignment between the articular surfaces of the tibia and femur. They are also highly important knee stabilizers because they help control and arrange knee movements.
Menisci’s fiber arrangement enables axial loads to be distributed radially, lessening the strain on the hyaline articular cartilage. It is crucial as, according to the gait and stair climbing, a compressive force through the knee can be as much as 1-2 times body weight, and as much as 3–4 times body weight when running.
Cardiovascular ligaments connect the menisci to the tibia. The medial meniscus has a significantly lesser range of motion than the lateral meniscus because of its strong attachment to the medial collateral ligament (MCL) and the knee joint capsule. A meniscus has no attachment to the lateral collateral ligament (LCL) and is less tightly connected to the joint capsule on its lateral side. However, a tendon of the popliteus muscle, which descends from the lateral epicondyle of a femur, completely separates the posterior horn of a lateral meniscus from the posterolateral side of the knee joint capsule.
The menisci are vascularized during the first year of life, but after weight bearing begins, the vascularity decreases to the outer third (red zone), where the only area with a slender healing capacity. Through the flow of synovial fluid within the joint, the white zone, an inner non-vascularized area, is nourished.
Bursa
In a bag filled with fluid, the bursa lessens friction between two tissues. There are several bursae surrounding a knee. When a knee injury occurs, the suprapatellar bursa, the most substantial sac in the body, frequently fills with fluid.
Bursae in front of the patella and pes anserine bursa at the point when the three medial muscles of the knee joint insertion connect are the most often injured bursae.
Structure of Knee Joint
What makes up your knee is:
- Bones.
- Cartilage.
- Ligaments.
- Muscles.
- Nerves.
Bones in the knee
In the knee joint, there are three bones:
- Femur (thigh bone).
- Tibia (shin bone).
- Patella (kneecap).
These points of intersection between the bones are referred to as articulations or articulating surfaces. Your knee has two locations where it can be articulated.
- Your femur’s patellofemoral joint is situated where it defines up with your patella.
- Tibiofemoral: The point on your tibia and femur that joins.
Bones
The bones of the knee are the patella (kneecap), tibia (shin bone), and femur (thigh bone). These bones are maintained in place by the knee joint.
The patella is a very small, triangular bone that is located inside the quadriceps muscle at the front of the knee. Due to the extreme stress of its activities, it has the thickest layer of cartilage in the body.
Cartilage
The knee’s cartilage is formed of two types:
Meniscus: these are crescent-shaped discs that serve as a “shock absorber” or cushion to allow the knee’s bones to move easily without contact with one another directly. The nerves in the menisci relate to increased stability and balance as well as proper weight distribution between the tibia and femur.
Two menisci exist in the knee:
- The medial side of the knee is the smaller of the two regions.
- lateral: on the knee’s outside surface
The thin, smooth layer of cartilage known as “articular cartilage” sits on the back of the patella, the top of the tibia, and the femur. It helps bones run easily over one another and act as a shock absorber.
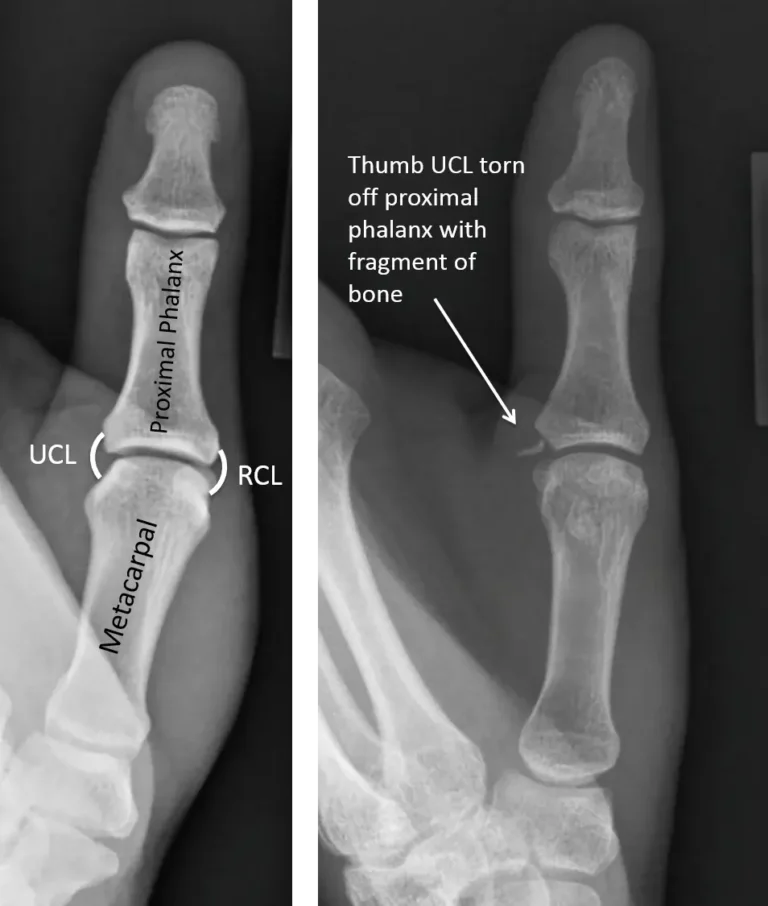
Ligaments Of Knee Joint
A joint capsule has a structure of smaller layers deep down and thicker, fibrous layers on the outside. It maintains the stability of the knee as part of the capsule ligaments. As is usually the case with other knee structures, they are most stable when extended (closed packed), as opposed to when flexed (open packed), when there is laxity.
The specialized membrane known as the synovial membrane, which supplies sustenance to all surrounding structures, is located inside the capsule. A knee joint is lubricated by synovial fluid, which forms a synovial membrane. The bursa and infrapatellar fat pad are two more tissues that mostly serve as cushions for external stresses on the knee.
The synovial fluid that lubricates the knee joint is pushed anteriorly during extension and posteriorly during flexion. The semi-flexed knee is the most relaxing posture in the event of a knee joint effusion since the fluid is under the least tension at this point.
A knee’s stability is preserved by its ligaments. Every ligament serves a specific purpose in helping to preserve the best possible knee stability.
Medial Collateral Ligament (MCL)
There are two types of fibers in this medial collateral ligament: superficial fibers and deep fibers. This band usually appears along the superior portion of the tibia’s medial surface and extends from the medial epicondyle of the femur to the medial condyle. The superficial fibers attach to the medial aspect of the proximal tibia, which is distal to the pes anserinus, and start from the medial femoral condyle. The deep fibers emerge on the inferior aspect of the medial femoral condyle, run the length of the knee joint capsule, and insert into the proximal aspect of the medial tibial plateau.
The deep fibers of a ligament attach to the medial meniscus in the middle. The medial collateral ligament generally opposes valgus forces acting on the outside of the knee, but it also opposes a tibia’s lateral rotation on the femur. The flexibility of a ligament in the open-packed position (flexed) allows the medial collateral ligament to resist the valgus stress more successfully in the closed-pack position (extension).
The medial collateral ligament indeed has another purpose in avoiding a tibia from anteriorly shifting onto the femur. Anterior cruciate ligament protection must therefore be taken into consideration when someone suffers an MCL injury.
Lateral Collateral Ligament (LCL)
The tendon of the biceps femoris, or hamstring muscle, and the cord-like ligament that rises on the lateral epicondyle of the femur to form a conjoined tendon. It is thought that the ligament is called the extracapsular ligament, which is different than the medial collateral ligament.
Anterior Cruciate Ligament (ACL)
The anterior tibial translation on the femur is the main purpose of the anterior cruciate ligament (ACL), an essential element of the knee joint. The cause of the cruciate ligaments being so well-known is that they create a cross in the center of the knee joint. As it shifts proximally, the anterior crucial ligament twists medially. The ACL is thought to be formed of two bundles of fibers: the posterolateral bundle (PLB) and the anteromedial bundle (AMB). The knee’s resistance to anterior shearing pressures is due to the anterior important ligament.
Posterior Cruciate Ligament (PCL)
This ligament comes from the tibia’s posterior surface and grows superiorly and anteriorly between the menisci’s two posterior horns prior to establishing the lateral aspect of the medial femoral condyle. According to the anterior cruciate ligament, the posterior cruciate ligament is shorter, less oblique, and has a much larger cross-sectional area. As it crosses to a tibial connection, the posterior cruciate ligament matches with a posterior capsule.
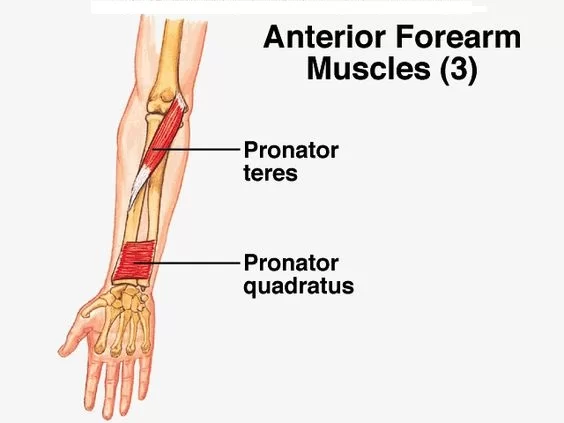
Muscles Around the Knee joint
Articularis genus muscle
- Origin: First femoral shaft distal end.
- Insertion: A knee joint capsule extended proximally.
- Blood supply: Femoral artery
- Nerve supply: Femoral nerve
- Action: Pulling a suprapatellar bursa while extending the knee.
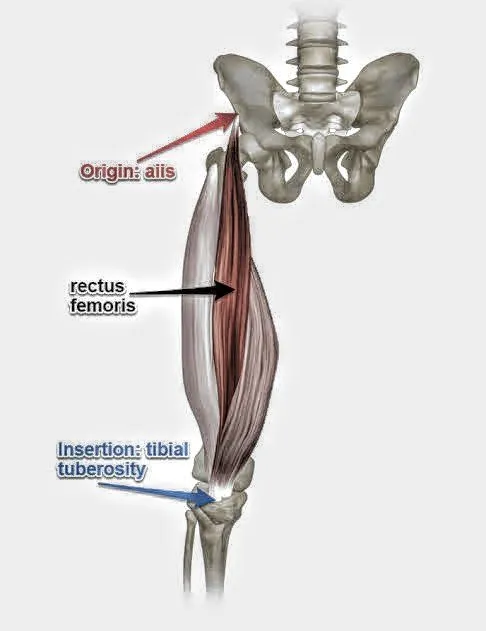
- Origin: Anterior inferior iliac spine or a portion of the acetabulum are passed on by the outer layer of a bony ridge.
- Insertion: via the patellar ligament, including the patella and the tibial tuberosity.
- Blood supply: Femoral artery.
- Nerve supply: Femoral nerve.
- Action: Both hip flexion and knee extension.
- The hamstring muscle is the antagonist.
Vastus lateralis
- Origin: Ankle, trochanter, and femur’s linea aspera as well as the intertrochanteric line.
- Insertion: At the patellar ligament, both the patella and the tibial tuberosity.
- Blood supply: Femoral artery.
- Nerve supply: Femoral nerve.
- Action: Stabilizes and extends the knee.
- The hamstring muscle is the antagonist.
Vastus intermediates
- Origin: The lateral intermuscular septum of the thigh, as well as the superior two-thirds of the anterior and lateral sides of the femur.
- Insertion: The deep part of the quadriceps tendon is inserted by the lateral edge of the patella.
- Nerve: Femoral nerve
- Blood supply: Lateral circumflex femoral artery
- Action: Knee extension
Vastus medialis
- Origin: the lower part of an intertrochanteric line, medial intermuscular septum, adductor magnus aponeurosis, and spiral line to medial lip of a linea aspera.
- Insertion: Into the quadriceps tendon’s medial side, where it connects the rectus femoris and other quadriceps muscles. It then surrounds the patella after passing through a patellar ligament and into the tibial tuberosity.
- Blood supply: Femoral artery.
- Nerve supply: Femoral nerve.
- Action: A knee extension.
- The hamstring muscle is the antagonist.
Knee Flexors muscles
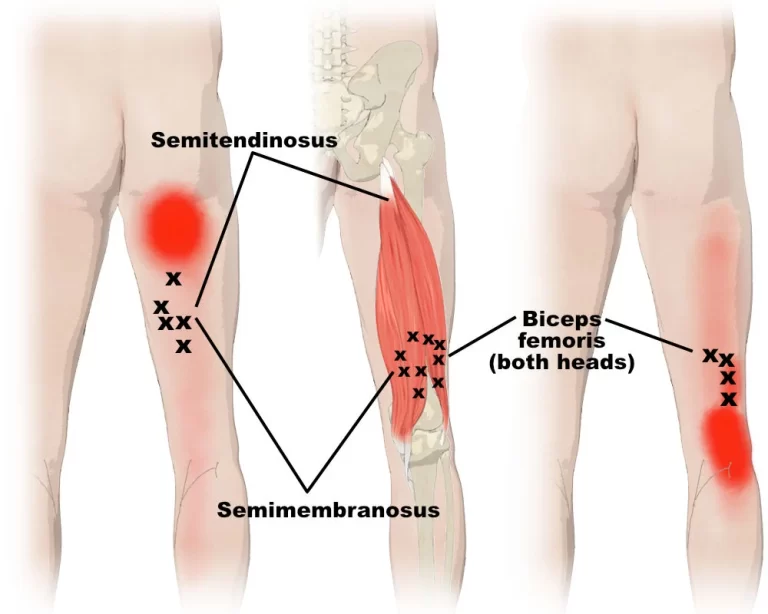
The main knee flexor muscles are the hamstrings.
Posterior compartment
Sartorius
- Origin: The pelvic anterior superior iliac spine.
- Insertion: Anserinus pes.
- Blood supply: The femoral artery, the descending geniculate artery, the lateral femoral artery, the deep femoral artery, or the superficial circumflex iliac artery.
- Nerve supply: Femoral nerve.
- Action: Abduction, flexion, and lateral rotation at the hip joint. The two flexions when medial rotation happens at the knee joint.
- Antagonism: partial quadriceps muscle
- Origin: Short head: a femur’s linea aspera; long head: the tuberosity of an ischium.
- Insertion: It connects the fibula’s afterward lateral tibial condyle.
- Supply of blood: Perforating arteries, popliteal artery, and inferior gluteal artery.
- Nervous system supply Short head: a lateral (common fibular) part of the sciatic nerve, long head: the medial (tibial) portion of the sciatic nerve.
- Action: Raising the hip joint (long head only), flexion of the knee, and laterally moving the leg at the knee (while the knee is in flexion).
- Quadriceps muscles are the antagonists.
Semitendinosus
- Origin: Ischial tuberosity impression from the posterior part of the skull.
- Insertion: Pes anserinus links the proximal end of the tibia to the medial condyle below.
- Action: Thigh extension, internal rotation, and pelvic support are the activities at the hip joint. The knee joint allows for internal rotation and leg flexion happen.
- Nerve supply: Sciatic nerve (L5-S2) tibial division
- Blood supply: inferior gluteal artery, medial femoral circumflex artery, first perforating branch of the deep femoral artery, and inferior medial geniculate artery.
Semimembranosus
- Origin: Ischial tuberosity superolateral impression.
- Insertion: Tibial condyle medially.
- Action: Do thigh extension and internal rotation at the hip joint.
- Knee joint: The pelvis is supported by flexion and internal rotation of the leg.
- Nerve supply: Sciatic nerve (L5–S2) tibial division
- Blood supply: It also involves popliteal and femoral artery perforating branches.
Gastrocnemius muscle
- Origin: Lateral head: The posterolateral borders of the lateral condyle on the femur. Medial head: The popliteal surface of the femoral shaft and the posterior surface of the medial femoral condyle.
- Insertion: Via the calcaneal tendon, the posterior element of the calcaneus.
- Nerve supply: Tibial nerve (S1, S2)
- Action: Plantar flexion of the foot at the talo-plantar joint and flexion from the leg at the knee joint.
Plantaris
- Origin: The popliteal ligament of the knee, and the lateral supracondylar line of the femur.
- Insertion: The calcaneal tendon connects to the posterior part of the calcaneus.
- Joint action: Plantar flexion of the talo-plantar and flexion of the knee.
- The tibial nerve (S1, S2) is the nerve’s root.
- Blood travels superficially via the lateral sural and popliteal arteries, and further below by the superior lateral genicular artery.
Popliteus
- Origin: The posterior horn of the knee joint’s lateral meniscus and the lateral condyle of the femur.
- Insertion: The front side of the proximal tibia.
- Nerve supply: The L4-S1 tibial nerve
- Blood supply involves the posterior tibial recurrent artery, posterior tibial artery, and tibia’s nutrient artery as well as the inferior medial and lateral genicular arteries (popliteal artery).
- Action: Loosens and stabilizes the knee joint.
Medial compartment
Gracilis
- Origin: The anterior pubic area body, ischial ramus, and proximal ramus.
- Insertion: Pes anserinus to the medial surface of the proximal tibia.
- Action: Leg internal rotation and flexion at the knee joint; Leg flexion and adduction at the hip joint.
- Nerve supply: The L2-L3 obturator nerve
- Blood supply: The adductor arteries take blood from the deep femoral artery.
Blood supply of knee joint
The plexus, or vascular network, around the knee joint, is partially formed by the femoral and popliteal arteries. The anterior tibial artery’s recurrent branch, the descending genicular artery, two superior genicular arteries, and two inferior genicular arteries form the six main branches. Into the knee joint are the medial genicular arteries.
The popliteal and femoral arteries are the primary donors to the genicular anastomosis that forms the abundant vascularization of the knee joint. Approximately 10 arteries are involved in the genicular anastomosis growth method:
- Descending branches: The genicular branch of the femoral artery and the descending branch of the lateral circumflex femoral artery.
- Ascending branches: anterior and posterior tibial recurrent branches of the anterior tibial artery, and the circumflex fibular branch of the posterior tibial artery.
- Three main branches develop in the popliteal artery: the lateral superior and inferior genicular arteries, the medial superior and inferior genicular arteries, and the middle genicular artery.
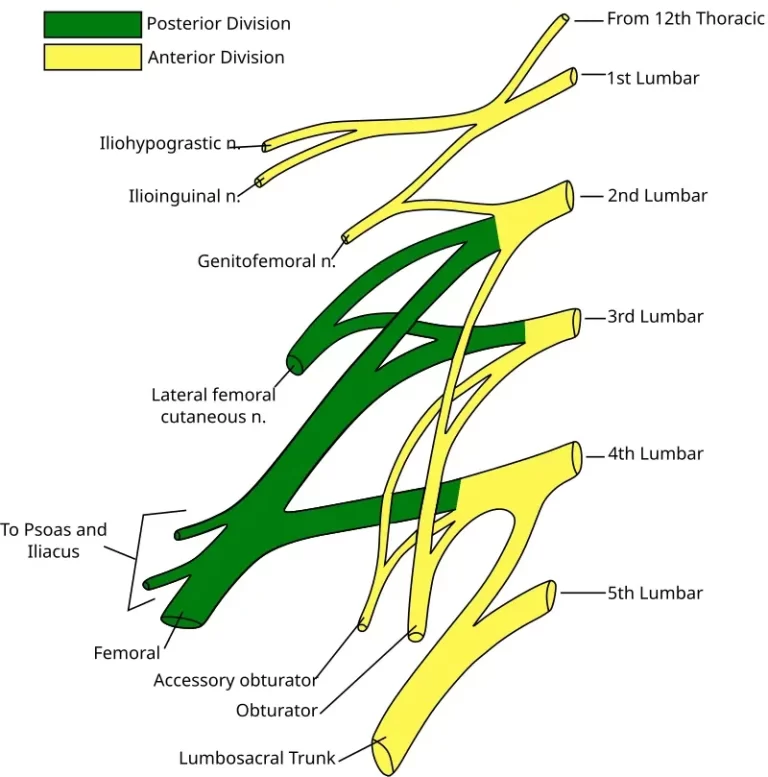
Innervation of the knee joint
The saphenous nerve and muscle branches supply the femoral nerve’s innervation to the knee joint. The posterior division of the obturator nerve, as well as the tibial and common fibular (peroneal) nerves, all assist the joint.
Movements of the knee joint
Since the knee joint is a hinge, its primary motions are flexion and extension in the sagittal plane. When the knee is flexed and at the final stage of extension, it permits limited medial rotation as well as lateral rotation. The knee joint, which is sometimes referred to as a modified hinge joint, is not a true hinge like the elbow joint since it has a moving component, an auxiliary motion that goes along with flexion and extension.
The knee joint enables four main types of movements:
- As the quadriceps femoris inserts into the tibial tuberosity, it generates extension.
- The hamstrings, gracilis, sartorius, and popliteus create flexion.
- The biceps femoris produce lateral rotation.
- The semimembranosus, semitendinosus, gracilis, sartorius, and popliteus are the five muscles that generate medial rotation.
The function of the knee joint
The knee can be grew and flexed about a virtual transverse axis. When the knee is flexed, it may pivot partially medially and laterally about the lower leg’s axis. The femur rolls and glides over both menisci during extension-flexion, and the lateral meniscus goes over the tibia during rotation, giving it the term “mobile” for the knee joint.
Located anterior to the transverse axis center of the extension/flexion movements is a connection among the collateral and cruciate ligaments. The femur’s center moves in both directions during flexion, and as the femoral condyles’ curvature reduces, this affects the distance between the center and the articular surfaces of the femur. Several factors, including tight hamstrings, active insufficiency, and soft-tissue restrictions, affect the general range of motion.
Clinical Significance
- Patellofemoral syndrome, or chondromalacia patella, is an irritation of the patella cartilage that ends in knee pain. The young knee pain can often be caused by this.
- Osteoarthritis: The most common kind of arthritis, osteoarthritis usually impacts the knees. Knee pain, stiffness, and swelling are some of the symptoms of osteoarthritis, which come from aging and cartilage deterioration.
- Knee effusion: a formation of fluid, usually brought on by inflammation, inside the knee. An injury or arthritis of any kind may end in a knee effusion.
- Meniscal tear: Twisting the knee may cause damage to the meniscus, which is the cartilage that cushions the knee. Knee stiffness may result from large rips.
- Tear or strain of the anterior cruciate ligament (ACL): The stability of the knee is dependent on the ACL. An ACL tear may need surgical repair since it often leads the knee to “give out.”
- PCL (posterior cruciate ligament) strain or tear: Inflammation, pain, and instability in the knee may occur from PCL tears. Usually, the best plan of action is physical therapy rather than surgery for these injuries, which are less prevalent than ACL tears.
- Tear or strain of the medial collateral ligament (MCL): This injury can result in pain as well as instability on the inner side of the knee.
- Patellar subluxation: When a person is active, their kneecap could move or dislocate along their thigh bone. Pain around the kneecap is what happens.
FAQs
Which joint is the knee?
Synovial joint in the hinge style
The primary range of action for the knee joint, which is a hinge-type synovial joint, is flexion and extension (with small medial and lateral rotation as well). It forms by the patella, femur, and tibia articulations.
How many components make up the knee joint?
The actual knee is formed up of four joints: one relates the patella (kneecap) and femur (thigh bone); a different divides the tibia and fibula (a smaller lower leg bone); and two join the tibia (shin bone) to the femur.
\Where is cartilage found in the knee?
The knee’s articular cartilage
Articular cartilage protects the surfaces of the tibia’s higher the kneecap’s back, and the femur’s lower bone. The substance known as articular cartilage is extremely durable, flexible, and smooth.
What three knee joints are there?
The knee’s medial compartment, or the inner joint between the tibia and femur. The joint on the outside where the femur and tibia relate is called the lateral compartment of the knee. The area where the kneecap connects the femur’s groove is known as the patellofemoral compartment.
Which three components make up the knee joint?
In the knee joint, there are three bones:
The femur, or the thigh bone
Lower leg bone: tibia
Kneecap Patella
References
- Physiotherapist, N. P. (2023b, December 13). Knee Joint: Anatomy, Physiology, Movement, Exercise, Importance. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/knee-joint/
- Dhameliya, N. (2023, August 10). Hip Joint – Anatomy, Structure, Function. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/hip-joint/
- Professional, C. C. M. (2024b, May 1). Knee Joint. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24777-knee-joint
- Knee. (2024, July 14). Wikipedia. https://en.wikipedia.org/wiki/Knee
- Knee joint. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/the-knee-joint

36 Comments