Humerus Bone
Introduction
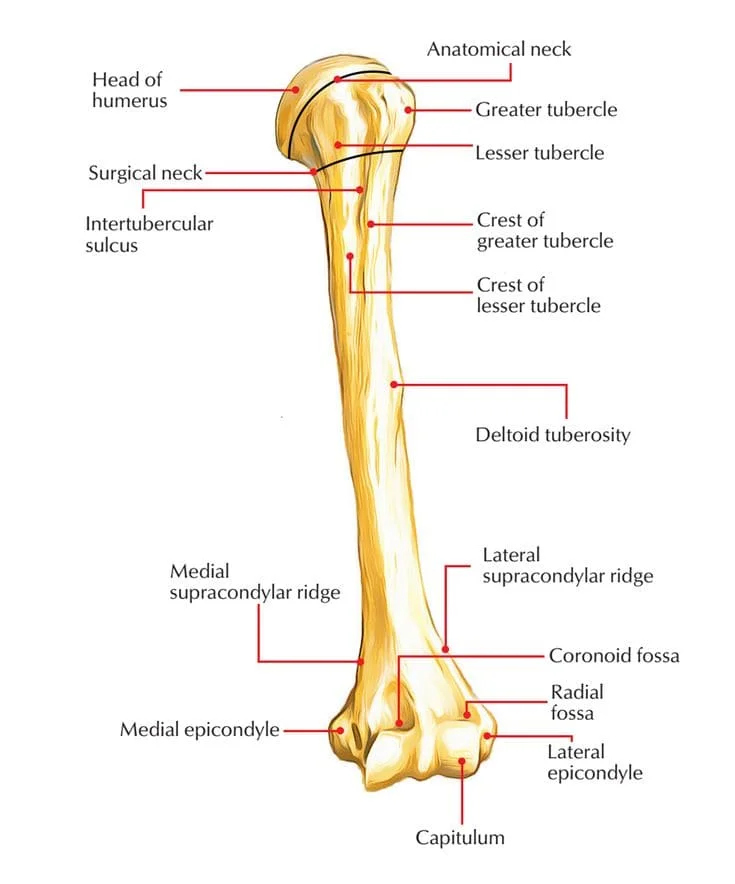
The humerus, the biggest bone in the upper extremities, makes up the human brachium, or arm. It articulates with the radius and ulna distally at the elbow joint and proximally at the glenohumeral (GH) joint with the glenoid. The humerus’s most proximal portion is its head, which connects to the glenoid cavity on the scapula.
The anatomical neck of the humerus, which splits The humeral heads from the larger and smaller tubercles is located just behind the humeral head. The humerus’s anatomical neck is made up of the remaining epiphyseal plate. This creates a ball and socket. An intertubercular groove seen proximally separates the two tubercles vertically. Following the tubercles comes the humeral surgical neck, which is frequently prone to fractures.
The posterior surface of the humerus’s cylindrical shaft, which extends distally and has a deltoid tubercle on the lateral side, is the site of the radial groove, also referred to as the spiral groove. Near the distal end of the humerus, the bone that comprises the medial and lateral epicondyles enlarges. The distal portion of the humerus finishes at the condyle, which is made up of the radial fossae, trochlea, capitulum, olecranon, and coronoid.
The condyle’s anterior medial surface trochlea articulates with the trochlear notch of the ulna bone, whereas the anterior lateral side condyle’s lateral capitulum articulates with the head of the radius bone. Located on the anterior side of the condyle, superior to the capitulum and the coronoid process of the ulna, is the radial fossa, which receives the head of the radius during flexion of the elbow joint. Above the trochlea is a structure known as the coronoid fossa. The olecranon fossa, located on the posterior aspect of the condyle, articulates with the olecranon of the ulnar bone during elbow flexion.
Structure and Function
The articulation of the humeral head with the glenoid fossa of the scapula forms the synovial ball and socket joint known as the glenohumeral joint. The activation of the rotator cuff muscles (teres minor, subscapularis, supraspinatus, infraspinatus, pectoralis major, and deltoid) determines the range of motion in this joint, which includes internal and external rotation, abduction and adduction, flexion, and extension.
Numerous synovial bursae, including the subacromial, subdeltoid, subcoracoid, and coracobrachial bursae, which allow frictionless movement, are found in the glenohumeral joint. The GH joint is stabilized and the humerus is kept from migrating proximally by the acromioclavicular and coracoacromial ligaments.
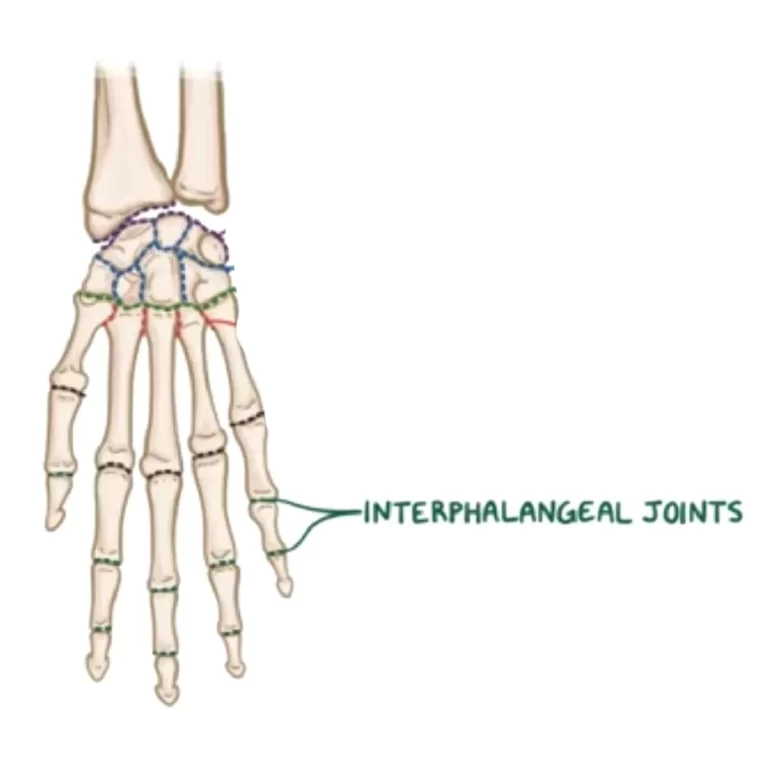
The elbow joint, a synovial hinge joint, is formed by the articulation of the capitellum and trochlea of the humerus with the head of the radius bone and the trochlear notch of the ulna. This joint is supported by the complexes of the ulnar (medial) and radial (lateral) collateral ligaments.
Three components comprise the ulnar collateral ligament (UCL):
Anterior oblique band: The most potent and significant stabilizer against valgus stress, it reaches the humerus’s medial epicondyle from the proximal ulna’s sublime tubercle.
Posterior oblique band: The highest shift in elbow ROM tension from flexion to extension is seen in the posterior component of the UCL.
Transverse ligament: provides support to the elbow joint.
In this case, an olecranon bursa also helps reduce friction while in motion. At this joint, only flexion and extension are possible. The muscles that control elbow mobility primarily include the triceps, coracobrachialis, and biceps brachii. It should be noted that the humerus and antebrachial do not line up exactly in terms of anatomy;
Embryology
The humerus is a long bone that grows by endochondral ossification, one of the several long bones in the appendicular skeleton. The replacement of a cartilage template with bone defines this process. Mesenchymal cells that produce cartilage-secreting chondrocytes first lay down a comparatively small cartilage model. Second, the ossification center, the heart of the cartilage template, is host to substances that create and promote the calcification of that cartilage, including chondrocyte hypertrophy and alkaline phosphatase. This results in a nutritional barrier and chondrocyte loss.
Furthermore, the VEGF secreted by these cells promotes angiogenesis in the calcifying tissue cartilage before passing away. Meanwhile, the Indian hedgehog homolog (IHH) protein stimulates cells outside the perichondrium to become osteoblasts, generating the bony collar—a bone layer covering the cartilage core. A core area of dead chondrocytes develops over time, encircled by a vascular supply, a shell of bone, and tiny pieces of calcified cartilage. The vascular supply brings in internal mesenchymal cells that differentiate into more osteoblasts and monocytes that make osteoclasts.
The bone is resorbed on the inside and deposited outside in the center of the original cartilage template, causing the hollow entity (forming a marrow) to develop. cartilage’s proximal and distal ends begin simultaneously. Cartilage development at the end of the bones is made possible by this mechanism, which permits vertical growth. Ultimately, the junction of bone and cartilage forms the linear zone of cartilage known as the epiphyseal plate. In this particular case, bone is constantly replaced by cartilage until bone development fully fuses at puberty.
While the ossification of the humeral head occurs at delivery or soon after, the ossification of the shaft occurs during the last eight weeks of pregnancy. The larger tubercle ossifies in the first year of life, whereas the smaller tubercle ossifies in the first six years. By the time an adolescent reaches puberty, every proximal ossification center on the humerus has merged with the shaft entirely. The distal ossifications at the condyle, trochlea, and olecranon occur between early and later adolescence. By late adolescence, they fuse with the humerus’ shaft.
Blood Supply and Lymphatics
The anterior and posterior circumflex humeral arteries are anastomose, providing the proximal humerus with its main blood supply. These branches start at the distal portion of the axillary artery.
According to recent research, the posterior humeral circumflex artery may be the main source of blood flow for the humeral head. Where the anterior humeral circumflex artery ends is where the arcuate artery, which supplies the majority of the larger tuberosity, comes to an end.
The axillary artery will give blood to the profunda brachii artery, one of the brachial artery’s branches, and the remaining portion of the humerus as it matures into the brachial artery. Nutrient arteries, which split off from the brachial artery around halfway down the bone, supply blood to the interior parts of the humerus.
Nerves
The Axillary nerve: which is derived from the posterior cord of the brachial plexus, surrounds the humeral surgical neck and stimulates the rotator cuff and deltoid muscles, with the teres minor receiving particular attention.
The Musculocutaneous nerve: The anterior portion of the brachium is innervated by the musculocutaneous nerve, which is a division of the lateral cord of the brachial plexus. The coracobrachialis muscle and the biceps brachii mark the termination of the forearm’s lateral cutaneous nerve.
The Radial nerve: It crosses the posterior cord of the brachial plexus, the spiral groove of the humerus, the long head of the triceps, and the brachial artery. It stimulates the muscles of the posterior arm, the skin around it, and the forearm. The radial nerve also communicates with the lateral and medial epicondyles of the humerus. It is important to remember that the ulnar and median nerves do not supply the brachial plexus, although they also begin there and descend to the brachium.
Muscles
Many muscles of the upper limb, including the scapulohumeral, anterior compartment, and posterior compartment muscles, originate from the humerus.
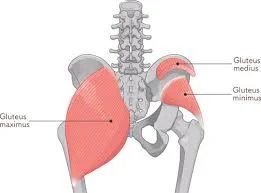
Scapulohumeral muscles: The deltoid muscle, which gives the upper limb the shoulder shape, originates from three locations on the scapula: the clavicle, the acromion of the scapula, and the scapula’s spine. Each of these components enters into the deltoid tuberosity of the humerus. The deltoid muscle allows for both internal and external rotation, as well as humeral abduction and adduction. Originating from the clavicle, manubrium, sternum body, and true ribs is the pectoralis major muscle. It enters the humerus’s intertubercular sulcus. The humerus is capable of medially extending, flexing, and adducting.
The rotator cuff is made up of four muscles – teres minor, supraspinatus, infraspinatus, and subscapularis muscles. The scapula’s subscapular fossa is the source of the subscapularis muscle, which attaches to the humerus’s lesser tubercle to enable internal rotation of the joint. To assist with humeral abduction, the supraspinatus muscle enters into the larger tubercle of the humerus from the supraspinous fossa of the scapula. The larger tubercle of the humerus is where the infraspinatus muscle enters after leaving the scapula spinale and infraspinous fossa. The humerus may rotate outward due to this muscle. The teres major, which enters the humerus’s smaller tuberosity from the scapula’s inferior angle, permits internal rotation and adduction. To assist in external rotation, the teres minor originates on the lateral edge of the scapula and inserts into the larger tubercle.
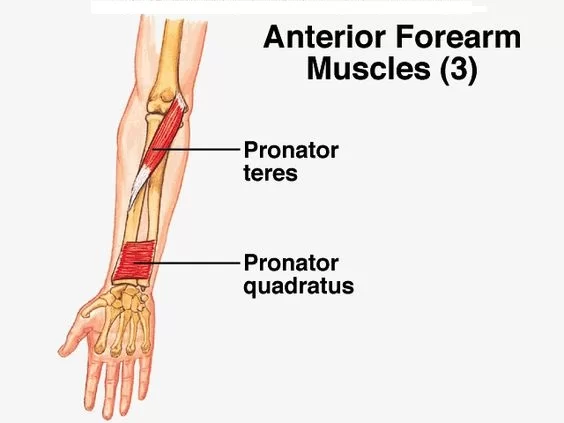
Anterior Compartment Muscles: Despite having a long and short head, the biceps brachii muscle has an origin or insertion site on the humerus. However, the transverse humeral ligament, which runs from the humerus’s smaller to greater tubercles, crosses the biceps brachii long head tendon, converting the humeral intertubercular groove into a canal. This tendon terminates at the radius and starts at the supraglenoid tubercle of the scapula. To allow flexion and internal rotation, the coracobrachialis arises from the coracoid process of the scapula and inserts into the medial side of the humerus. To flex the forearm, the brachialis muscle enters the ulna from the front of the distal humerus.
Posterior compartment muscles: The brachialis muscle enters the ulna from the front of the distal humerus to flex the forearm. The medial head of the triceps brachii muscle originates on the posterior part of the humerus, inferior to the spiral groove, whereas the lateral head originates on the posterior side. Forearm extension at the elbow joint is made possible by both heads entering the olecranon process of the ulna. The posterior circumflex artery, vein, and nerve pass via a quadrangular area that is made up of the humerus, the long head of the triceps, the teres major and minor, and the radian nerve.
Surgical Considerations
Older people who fall on their shoulders or with their arms extended may suffer proximal humeral fractures. This injury appears as rigidity of the limbs and soreness in the shoulders. Several breakdowns of these proximal fractures may lead to post-traumatic osteonecrosis along with long-term illness. Most proximal humerus fractures don’t require surgery for treatment. However, elderly patients with significant displacement may benefit from surgery since their bones are not remodeling and developing as much. For internal fixation, percutaneous alternatives include needle wires, smooth wires, cannulated screws, and intramedullary nailing.
Reverse shoulder arthroplasty can also be used to treat glenohumeral dislocations, rotator cuff tears, joint arthritis, and proximal humerus fractures in the elderly. Inflammatory arthritis and osteoarthritis may also require shoulder arthroplasty. Anterior dislocation of the glenohumeral joint is common in young, active patients. Subacromial impingement and damage to the rotator cuff muscles can result from humeral fractures affecting the greater tuberosity of the humerus. Usually, when there are displacements of more than 3 mm, surgery is necessary.
Children three years old and younger may get distal humerus transphyseal fractures following a fall or other trauma. The cubitus varus will be clearly visible on radiologic imaging, and the humerus and forearm bone will not align with the usual carrying angle. During surgery, closed reduction and percutaneous anchoring techniques should be used. Common side effects include condyle osteonecrosis and growth stop. Dome, multi-planar, or lateral closure wedge osteotomies are common surgical procedures.
An olecranon osteotomy is a common surgical procedure used to treat distal humerus intercondylar fractures. Because the trochlear blood supply is cut off post-traumatic supracondylar humeral fractures may develop in avascular necrosis. At the time of the injury, patients may not show any symptoms; however, within six months, pain associated with necrosis or loss of movement can occur.
Clinical Significance
Radial Nerve Injury
One of the most frequent injuries to peripheral nerves that results from a humeral fracture is radial nerve palsy. Therapy typically consists of the normal course of treatment includes monitoring until nerve healing—as assessed by EMG/NCS testing—occurs within three to six months. Damage to the radial nerve may result from an injury or break at the mid-shaft radial groove.
Conditions of the Shoulder
Two more common conditions with unclear and/or complicated causes are calcific tendinitis of the rotator cuff and adhesive capsulitis of the shoulder, sometimes referred to as frozen shoulder syndrome. Surgery is rarely required; the primary types of therapy are rest and exercise. On the other hand, frozen shoulder syndrome can be surgically treated under general anesthesia.
Metastatic Disease
Metastatic bone disease usually affects the humerus and presents with severe bone lesions and strong localized pain. Lesions can raise the risk of a humeral fracture. For those whose injuries do not involve 50% of the cortex, externally administered radiation is one type of treatment. For serious lesions that extend more than half of the cortex, however, intramedullary nailing along with postoperative external beam radiation is the preferred course of treatment. It can be essential to remove or restore bone if the condition gets worse.
Supracondylar Fractures of the Distal Humerus
Most cases of this kind of elbow fracture happen to young persons. The superior condyles, fracture site, and medial and lateral condyles are all present. Surrounding the elbow joint, supracondylar fractures of the distal humerus may cause nerve and vascular problems, depending on the degree of displacement of the fracture. Anterior dislocation puts the median nerve and brachial artery in harm. The radial artery might be in danger from a posterior displacement.
Palpation of the distal pulse should be done as part of the initial examination to ensure that the blood supply is intact. For accurate diagnosis and treatment, radiographs from the front, back, and side are needed. A posterior splint is used as a first therapy for nondisplaced fractures, and thereafter casting is applied. Displaced fractures are retracted and connected subcutaneously. The following conditions are linked to this fracture: malunion, compartment syndrome, and neurovascular issues.
Radial nerve palsy is among the most common damage to peripheral nerves following a humeral fracture. Therapy typically consists of the normal course of treatment includes monitoring until nerve healing—as assessed by EMG/NCS testing—occurs within three to six months. Damage to the radial nerve may result from an injury or break at the mid-shaft radial groove.
Conditions of the Shoulder
Two more common conditions with unclear and/or complicated causes are calcific tendinitis of the rotator cuff and adhesive capsulitis of the shoulder, sometimes referred to as frozen shoulder syndrome. Surgery is rarely required; the primary types of therapy are rest and exercise. On the other hand, frozen shoulder syndrome can be surgically treated under general anesthesia.
Metastatic Disease
Metastatic bone disease usually affects the humerus and presents with severe bone lesions and strong localized pain. Lesions can raise the risk of a humeral fracture. For those whose injuries do not involve 50% of the cortex, externally administered radiation is one type of treatment. For serious lesions that extend more than half of the cortex, however, intramedullary nailing along with postoperative external beam radiation is the preferred course of treatment. It can be essential to remove or restore bone if the condition gets worse.
Supracondylar Fractures of the Distal Humerus
Supracondylar Fractures of the Distal Humerus occur mainly in young people. The superior condyles, fracture site, and medial and lateral condyles are all present. Surrounding the elbow joint, supracondylar fractures of the distal humerus may cause nerve and vascular problems, depending on the degree of displacement of the fracture. Anterior dislocation puts the median nerve and brachial artery in harm. The radial artery might be in danger from a posterior displacement.
Palpation of the distal pulse should be done as part of the initial examination to ensure that the blood supply is intact. For accurate diagnosis and treatment, radiographs from the front, back, and side are needed. A posterior splint is used as a first therapy for nondisplaced fractures, and thereafter casting is applied. Displaced fractures are retracted and connected subcutaneously. The following conditions are linked to this fracture: malunion, compartment syndrome, and neurovascular issues.
Other/Miscellaneous Conditions
Hematologic, viral, genetic, or neurological disorders can cause humerus varus. In this case, the proximal humerus’s lateral portion will grow faster than its medial region, which will not develop normally. This condition causes the humerus to rotate the varus, which reduces arm abduction and restricts flexion at the shoulder joint. However, impairment in function is not common. A valgus osteotomy of the humerus is surgically performed using a plate screw fixation.
Disappearing bone disease is a rare musculoskeletal condition marked by loss of bone, impaired bone development, and inadequate vascular growth. Similar to this, Gorham-Stout disease of the humerus is defined by erosion of the osseous matrix along with a lack of bone growth. It is unclear what is causing the illness, however there is a lymphovascular irregularity in the bone. Common signs include aching pain, weakening, and eventually fractures. Surgery, medication, and radiation therapy are all used for the treatment.
An uncommon condition called Charcot arthropathy is characterized by extreme joint deterioration. The illness may make it difficult to regulate muscles and result in the loss of bone and soft tissue around the humerus. A shoulder arthroplasty is the course of treatment.
Humeral osteochondrosis has been linked with Panner disease and osteochondritis dissecans. Panner disease is characterized by avascular necrosis of both illnesses have similar indications and symptoms. capitulum and often occurs between the ages of 7 and 10, which is one year earlier than osteochondritis dissecans. In general, panner disease is not treated with surgery.
FAQs
What does humerus mean in medical terms?
It’s essential to your arm’s range of motion. Numerous essential muscles, tendons, ligaments, and parts of your circulatory system are also supported by the humerus.
What is the function of the humerus bone?
In addition to providing structural support for the arm, the humerus is where several significant upper body muscles, including the rotator cuff muscles, pectoralis major, and latissimus dorsi, arrive.
What nerve is in the humerus?
The brachial artery, the long head of the triceps, the humerus’ spiral groove, and the posterior chord of the brachial plexus are all crossed by the radial nerve. It innervates the muscles of the posterior arm, the skin around it, and the forearm.
What is a humerus fracture called?
The humerus, often called the upper arm bone, is a lengthy bone that extends from the shoulder, or scapula, to the elbow. There are two types of humerus fractures: proximal humerus fractures and humerus shaft fractures.
What is the head of the humerus?
The humerus’s almost hemispherical head articulates with the scapula’s glenoid cavity and faces upward, medially, and somewhat rearward.
References
- Mostafa, E., Imonugo, O., & Varacallo, M. (2023, August 7). Anatomy, Shoulder and Upper Limb, Humerus. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK534821/
- Rohit, B. (2023, April 17). Humerus Bone – Anatomy, Location, Function – Samarpan Physio. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/humerus-bone/


5 Comments